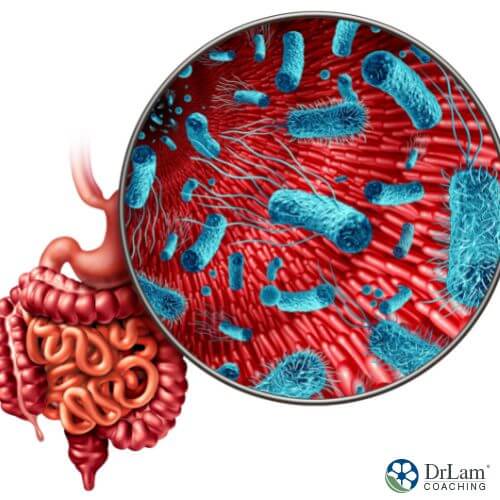
 Your gut microbiome, or the balance of bacteria in your gut, plays a huge role in your health. When you experience dysbiosis, or an imbalance of this bacteria, it can lead to a host of health problems, including abdominal pain, nausea, and diarrhea. A Fecal Microbiota Transplantation (FMT) is an unorthodox but highly successful procedure used to relieve certain of these chronic digestive disorders.
Your gut microbiome, or the balance of bacteria in your gut, plays a huge role in your health. When you experience dysbiosis, or an imbalance of this bacteria, it can lead to a host of health problems, including abdominal pain, nausea, and diarrhea. A Fecal Microbiota Transplantation (FMT) is an unorthodox but highly successful procedure used to relieve certain of these chronic digestive disorders.
Recently, numerous trials have demonstrated FMT to be an effective way of addressing for recurrent Clostridium difficile infection (CDI). It has even proven helpful in those with coexisting illnesses or those who are immunosuppressed. FMT has alo been used more broadly to address microbiome imbalances in a variety of conditions. However, it is an emerging therapy, and it also has some serious risks.
During a Fecal Microbiota Transplantation (FMT), some of the “bad” bacteria in your colon are replaced with “good” bacteria. You might need this procedure after taking antibiotics, which kill or severely restrict beneficial microorganisms. These microorganisms can be restored through this process. Other names for this process include stool transplant and fecal bacteriotherapy.
A Fecal Microbiota Transplantation involves collecting a stool specimen from a healthy donor. The majority of respondents pick a relative or long-time friend. The donor must have gone at least two to three days without taking antibiotics. They will undergo a blood and stool examination to check for abnormalities and infections. Once the donor has been cleared, and the doctor deems the recipient ready, you are able to move on to the following stages of transplantation.
The donor's stool is retrieved, combined with saline water, and screened. After that, the stool combination is introduced into your colon via a tube that passes through a colonoscope (which is a thin, flexible tube with a tiny camera attached to the end).
The donor stool can also be delivered via a tube that enters the stomach through the mouth. Taking a pill containing freeze-dried donor feces is another option.
In general, FMT works by adding healthy gut bacteria into your digestive tract. These bacteria compete against bad bacteria, helping to maintain a healthy balance in your microbiome.
For example, in a healthy gut population, a bacterium known as Clostridioides difficile (C. difficile) is controlled by numerous other bacterial species. However, if you have been using antibiotics, it can damage this environment by eliminating the other, defending bacteria. Worse, antibiotic-resistant spores are produced by C. difficile, making it difficult to get rid of.
This bacterium, which is no longer outcompeted, can then establish itself in the stomach and release toxins. These can lead to symptoms such as severe diarrhea, abdominal discomfort, and frequent fever.
However, studies show that C. difficile can be held in check by a boost of germs from a healthy donor's feces.
Additionally, researchers are investigating FMT's potential application in the management of Irritable Bowel Syndrome (IBS) and Crohn's disease.
 The majority of recent clinical experience with FMT has been with recurrent CDI. Several studies show restoring normal microbiota after FMT may be responsible for the extraordinary successes. In CDI, the intestinal mucosa is suited for FMT because of the dysbiosis brought on by the use of antibiotics. FMT restores weakened flora.
The majority of recent clinical experience with FMT has been with recurrent CDI. Several studies show restoring normal microbiota after FMT may be responsible for the extraordinary successes. In CDI, the intestinal mucosa is suited for FMT because of the dysbiosis brought on by the use of antibiotics. FMT restores weakened flora.
Clinical trials are also investigating FMT as a possible therapy for Inflammatory Bowel Disease (IBD). Encouraging case reports have shown that FMT may be an effective first-line treatment. However, response rates have not been as striking as with CDI.
Furthermore, step-up or intensive-dosing multi-donor FMT was used in IBD patients, suggesting more aggressive therapy is needed. However, the results showed positive therapeutic outcomes.
Crohn's disease patients have also been successfully aided with FMT. However, unresponsive instances have also been documented.
Other conditions Fecal Microbiota Transplantation may be used for include:
A Fecal Microbiota Transplantation is a helpful therapy for treating a C. difficile infection and other forms of dysbiosis, but it comes with significant hazards.
A complicated living mashup of bacteria and other species makes up stool. Despite extensive screening for recognized infectious agents in stool donors, there is always a chance that a pathogen may slip between the cracks.
Additionally, obtaining an FMT by colonoscopy or another form of delivery could come with discomfort and potential procedural complications.
Another worry is Fecal Microbiota Transplantation's long-term consequences for your immune system. However, there isn't much research on this topic.
Numerous case studies have suggested a potential connection between receiving FMT and a number of illnesses, including rheumatoid arthritis, idiopathic thrombocytopenic purpura, Sjögren's disease, and peripheral neuropathy.
Other risks might include:
You should be aware that if you had an FMT, the therapy might have some side effects. Some undesirable outcomes include:
Every individual has a microbiome that is entirely unique. The microbiome is made up of bacteria that can be both beneficial and detrimental. The majority are symbiotic (beneficial to both human health and the microbiota), while a tiny number are harmful (promoting disease).
When balanced, the host receives help from the microbiota in metabolizing foods into substances that promote a positive host/microbiota connection. These metabolites support the human and microbiota barrier, reduce inflammation, and improve the immune system.
Dysbiosis, however, prevents these typical interactions. An imbalance can be brought on by infectious diseases, particular diets, or the extended use of antibiotics or other therapies that kill bacteria. The body might become more prone to illness as a result.
 Stress and diet alter the gut flora, but research into how they interact in people is still in its early stages. Evidence points to reciprocal interactions between stress/mood, food, and gut flora. These interactions can result in either a vicious cycle or a beneficial cycle, depending on the factors involved.
Stress and diet alter the gut flora, but research into how they interact in people is still in its early stages. Evidence points to reciprocal interactions between stress/mood, food, and gut flora. These interactions can result in either a vicious cycle or a beneficial cycle, depending on the factors involved.
Stress causes a rise in gut leakage, particularly at tight junctions. This is the ordinarily-impermeable space between the cells lining the gut. Pathogens, toxins, and bacterial antigens can penetrate this barrier and infiltrate the bloodstream. Locally, a mucosal immune response is triggered, changing the makeup of the microbiota. This can lead to a variety of gut problems and wider systemic problems.
In this way, the health of our gut bacteria is directly influenced by our ability to manage stress and the function of our adrenal glands. When stress is chronic, adrenal fatigue can result, along with a host of digestive problems. Cramping, food sensitivity, gastrointestinal discomfort, intolerance to medications and supplements, and others are GI symptoms that are linked to Adrenal Fatigue Syndrome (AFS). As the balance of good gut bacteria improves, these symptoms typically get better. Research on the microbiota and adrenal fatigue may provide fresh perspectives on preventative care options.
As adrenal fatigue progresses to the advanced phases, harmful bacterial overgrowth and GI dysbiosis present significant therapeutic problems. Beneficial bacteria may be reduced or overwhelmed. Our intestines can become overrun with fungi and harmful bacteria, which can cause inflammation and localized damage to the gut lining. As adrenal fatigue worsens, systemic inflammation might develop, worsening stress levels and symptoms in turn.
However, a Fecal Microbiota Transplantation may help restore normal microbiome levels. This could help improve dysbiosis and AFS symptoms. On the other hand, there is a risk that potentially introducing other bacteria and pathogens from donor stool could worsen AFS. You should discuss options with your doctor.
Your body was designed to handle occasional bouts of severe stress. It has many organs and systems to help deal with stressful situations. These organs and systems constantly collaborate to restore and preserve homeostasis. Your NeuroEndoMetabolic (NEM) Stress Response is made up of various defense mechanisms.
A good and natural reaction against dangerous stimuli is acute inflammation. On the other hand, chronic inflammation can seriously harm your health. These damaging stimuli can be internal, like aberrant cells, or external, like diseases or toxins. Inflammation aims to get rid of these irritants as well as damaged cells and tissues. It also helps support tissue repair.
Your Inflammation circuit is made up of your immune system, microbiota, and gut. The Inflammation circuit is a vital response mechanism when your body is under stress. This link between stress and the Inflammation circuit explains how stress can have a substantial impact on your gut flora.
According to research, you can balance the gut flora and reduce inflammation in the body by correcting microbiota imbalances. Studies have found that inflammation markers decrease following a Fecal Microbiota Transplantation from two distinct donors. Additionally, they noticed a reduction in symptoms. This could help Inflammation circuit imbalances associated with AFS.
 The microbiome in your gut is made up of trillions of live bacteria. Neurotransmitters like serotonin and dopamine are produced continuously by these little mood enhancers. This is why ensuring that your microbiome is diverse and robust can benefit your mental health as well as your physical and digestive health. It can also help prevent problems like overeating.
The microbiome in your gut is made up of trillions of live bacteria. Neurotransmitters like serotonin and dopamine are produced continuously by these little mood enhancers. This is why ensuring that your microbiome is diverse and robust can benefit your mental health as well as your physical and digestive health. It can also help prevent problems like overeating.
Remember to check with your doctor or nutritionist before making any major changes to your diet, especially if you have other health conditions. However, for most people, these tips are good ways to support your microbiome.
Vegetables are packed with fiber, which humans cannot digest but which are eaten by the healthy bacteria in your gut. People who eat a diet high in fruits and vegetables have been found to have a lower risk of developing inflammation and better digestive health.
Monosaccharides, also known as fast-digesting sugars, are broken down so rapidly that your gut bacteria never get a chance to eat them. Your microbiota may actually starve to death if you consume a lot of simple sugars on a daily basis. The lining of your intestine could also be attacked by ravenous microorganisms, which can cause inflammation.
In order to ensure a contented and healthy microbiota, try to ensure your diet incorporates foods with complex carbohydrates like whole grains, vegetables, and legumes.
Probiotics consist of live bacteria that will help make sure mostly beneficial germs occupy your gut. Be careful to research any probiotic supplements, because many probiotic products on the market falsely claim to contain live cultures. You can also get probiotics from fermented foods such as yogurt, kefir, and sauerkraut.
With the use of donor stool, Fetal Microbiota Transplantation may help restore gut health for certain conditions, especially CDI. However, there is a possibility of disease transmission between the donor and recipient, unfavorable outcomes, and ambiguous effects on the recipient's immune system. You can also support a healthy microbiome by eating more complex carbohydrates and probiotics.
The Dr. Lam Coaching team can be of assistance if you need help improving your microbiome health. Call us at +1 (626) 571-1234 for a free, no-obligation phone consultation, where we will discreetly discuss your symptoms and your alternatives. By clicking here, you can also ask a question via our Ask The Doctor page.
Fecal Microbiota Transplantation (FMT), is a technique that involves giving someone healthy human donor stool through a colonoscopy, enema, nasogastric (NG) tube, or capsule form. This procedure is generally performed for crippling gastrointestinal infections like Clostridium difficile infections.
