 Neurodegenerative conditions and issues with cognitive function are on the rise. And although those are problems that usually come with age, we’re seeing more and more people affected by them earlier in life. Thankfully, there’s now more awareness about dietary approaches to these issues. This article outlines the best nutrition for brain health and how you can make use of these foods yourself.
Neurodegenerative conditions and issues with cognitive function are on the rise. And although those are problems that usually come with age, we’re seeing more and more people affected by them earlier in life. Thankfully, there’s now more awareness about dietary approaches to these issues. This article outlines the best nutrition for brain health and how you can make use of these foods yourself.
The Standard American Diet (SAD), which is also referred to as the Standard Western Diet, is correlated with a decline in cognitive function. When you look at a map of where Alzheimer’s disease (AD) is most concentrated, you’ll see that it’s where these diets are eaten. Countries like the US, the UK, France, Spain, Australia, and the Scandinavian countries have the highest rates. The same is true for Multiple Sclerosis.
The ApoE4 allele is one of the biggest risk factors for developing AD. In fact, the Yoruba people of Nigeria have the highest frequency of the ApoE4 allele yet some of the lowest rates of AD in the world.
So, how is that? What this tells us is that neurodegenerative conditions are not just a matter of genetics. It seems that having the gene is not the same thing as activating the gene. And what activates disease genes are environment and lifestyle. Mainly, your diet, stress levels, physical activity, and sleep.
And the Western diet is also correlated with many other health problems, including cardiovascular disease, obesity, diabetes, endocrine dysfunction, and adrenal fatigue. That’s why one of the main areas we focus on with our clients is undoing the damage that the SAD has caused. The adrenal fatigue diet, adjusted to each individual, is the cornerstone of our recovery programs.
Research shows that what we eat and lifestyle factors can change how our genes are expressed, turning some on and others off. There are several diets that can be especially helpful for undoing the damage of the SAD diet, encouraging healthier genetic expression, and supporting nutrition for brain health. The adrenal fatigue diet, the Mediterranean Diet, the MIND Diet, and the KetoFlex Diet, in particular, are ways of eating that can help you improve cognition and manage neurodegenerative conditions. We'll be getting into more detail on each diet later.
First, however, it's important to understand the mechanism behind how your food can affect your genetics.
Your genome is quite the miracle. It’s composed of 23 pairs of chromosomes that add up to around three billion DNA base pairs, with DNA being the biological foundation of heredity. Your genes, which are what contain your DNA, are located on your chromosomes. These chromosomes you got as copies from your father and mother.
 DNA is what contains the information your body needs to make proteins. It’s like a code made out of the order of the bases on the DNA strand. What’s really mind-boggling is that we only understand around 3% of human DNA, and we don’t know what the other 97% does or affects. Pretty much all the cells of your body, except your red blood cells, contain your DNA.
DNA is what contains the information your body needs to make proteins. It’s like a code made out of the order of the bases on the DNA strand. What’s really mind-boggling is that we only understand around 3% of human DNA, and we don’t know what the other 97% does or affects. Pretty much all the cells of your body, except your red blood cells, contain your DNA.
When scientists first realized just how pervasive DNA is, the medical community began to see many diseases as mostly predetermined by DNA. It seemed that there wasn’t much we could do about disease risk, since it depended on family history. And that kind of perspective made diet and lifestyle take the backseat. The thinking was, "You have a family history of AD? Well, there’s not much you can do about it except wait and see."
However, this very deterministic view is quickly becoming outdated - all thanks to newer research in epigenetics. Epigenetics is the study of how gene expression can change as a result of environmental and lifestyle factors.
Having a gene and expressing a gene is not the same thing. A genotype is the specific genetic makeup you inherit from your family. This is not something that changes during your lifetime, except via mutation, if a spontaneous genetic variation occurs in your DNA sequence.
A genotype can express itself in various ways. That expression then becomes a phenotype.
Your phenotype is the result of your genotype’s interaction with your environment. It’s what makes it so that you have your own unique biochemical and physical traits rather than just being a copy of your parents. Your particular gene expressions, or which genes are activated and which are not, are something that can change without there being a change to the DNA sequence. Your phenotype is flexible and adaptable.
In fact, your genetic expression is changing all the time. It responds to your environment, your stress levels, your activities, and your food choices. These changes can range from what types of organ cells your stem cells become, to how your memory is encoded, to whether you develop a disease that you’ve inherited the gene for or not.
If we take the Yoruba people of Nigeria as an example, we can say that the AopE4 allele is present in their genotype, but they don’t express it at high rates in their phenotypes. And that’s likely thanks to the epigenetic influence of their diet, lifestyle, and environment.
The growing research on epigenetics is good news for all of us. If you have a family history of a certain condition, it means you have a certain measure of control here. And nutrition is key. And the research supporting that perspective is getting bigger every day.
Food can either become your biggest ally or your biggest enemy when it comes to health. It can be what keeps genes that increase your risk of specific diseases switched off. It can also be what switches them on. Food can be what causes or stops chronic inflammation. It can be what harms or heals your gut. And it can be what supports or dysregulates your stress response system.
 These epigenetic effects of food influence your whole body, but when it comes to nutrition for brain health, the Neuroaffect Circuit is particularly relevant.
These epigenetic effects of food influence your whole body, but when it comes to nutrition for brain health, the Neuroaffect Circuit is particularly relevant.
The NeuroEndoMetabolic (NEM) Stress Response is the global system your body uses to handle stress. It is composed of six circuits, of three related organs/systems each, that work together to manage stressors.
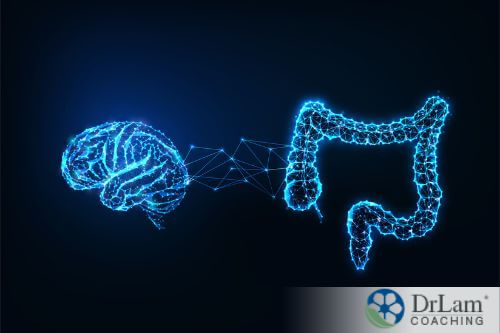
The NEM’s Neuroaffect Circuit is the triad of organs and systems that help you deal with mental and emotional stress. This triad is composed of your brain, autonomic nervous system (ANS), and microbiome. It uses neurotransmitters as its main method of communication. The neurotransmitters produced by these components are what regulate how you think and how you feel.
Your ANS is the part of your nervous system that helps regulate different functions without the need for conscious control. It consists of different subdivisions, like the sympathetic nervous system (SNS), the parasympathetic nervous system (PNS), and the adrenomedullary hormonal system (AHS). Your gastrointestinal (GI) tract has its own branch of the ANS, called the enteric nervous system (ENS).
Your SNS is the subdivision responsible for dealing with mild stress. The neurotransmitter norepinephrine is the one mostly used for this function, and it puts your body into the “fight or flight” mode, making your brain more alert, your heart beat faster, and getting more oxygenated blood circulating throughout your system. If your stress is more severe, then the AHS steps in. This subdivision uses adrenaline, which is your body’s most potent stress hormone and neurotransmitter.
Once the stress has passed, your PNS takes over and puts your body back into a state of rest and digestion. Your ENS, which is responsible for regulating the movement of your GI tract muscles and moving food throughout, reacts to what’s happening with the rest of your ANS. During a stress response, it slows down in order to allow your body to use the energy elsewhere. Once the PNS takes over, it can then get back to its regular functioning.
A few years ago, when we would mention the microbiome as playing a central role in mental health, our readers would be somewhat confused. But nowadays, the research on this link has gotten a lot more advanced and mainstream. And you are likely not very surprised to read now that the gut microbiome is part of the Neuroaffect Circuit.
The gut-brain-microbiome axis is actually one of the most interesting networks that we work with. It’s extremely useful when it comes to mental health and cognitive function because it makes these more accessible to nutrition for brain health.
 Your microbiome is a collection of trillions of microorganisms, working together in a kind of balance. Your gut also contains two-thirds of your immune system cells and is where most of your neurotransmitters are made. The communication between your gut and brain happens mainly via the vagus nerve, and it is bi-directional. That means if one component is affected, the other is as well.
Your microbiome is a collection of trillions of microorganisms, working together in a kind of balance. Your gut also contains two-thirds of your immune system cells and is where most of your neurotransmitters are made. The communication between your gut and brain happens mainly via the vagus nerve, and it is bi-directional. That means if one component is affected, the other is as well.
When your microbiome is in balance and your gut is working well, you’re much more likely to have better mental health and cognitive function. But if your microbiome is not balanced – a state called dysbiosis – you are at risk of mental health issues and cognitive decline. Oftentimes, the component that dysregulates the entire Neuroaffect Circuit is the microbiome. And one of the main causes of dysbiosis is chronic stress.
Chronic stress is a root cause of many chronic conditions. This is, in part, because our bodies did not evolve to deal with chronic stress. They evolved to deal with acute stress, and then to get back to a parasympathetic state as quickly as possible. But modern life is filled with stressors. Many of them are mild in comparison to what our ancestors had to face, yet they are constant. These stressors include things like:
The list goes on. But the idea here is that the stress isn’t just once in a while, it’s something your body has to face constantly. Usually on a daily basis.
Chronic stress means that your NEM Stress Response is chronically triggered. Its main responders are the adrenal glands. They secrete your body’s main anti-stress hormone, cortisol. And although cortisol fluctuates throughout the day naturally, if its levels are too high or too low for a sustained period, Adrenal Fatigue Syndrome (AFS) can result.
Symptoms of AFS include fatigue, weight gain, hair loss, dry skin, loss of libido, PMS, infertility, hypoglycemia, salt and sugar cravings, heart palpitations, unstable blood pressure, frequent colds and flus, estrogen dominance, dysbiosis, chronic inflammation, brain fog, sleep disturbances, anxiety, and mild depression.
AFS symptoms are so varied because of how it affects all six NEM circuits: the Hormone, the Bioenergetics, the Cardionomic, the Neuroaffect, the Inflammation, and the Detoxification circuits. But since we are talking about the best nutrition for brain health, we’re mostly interested in how nutrition can help with symptoms like anxiety, depression, insomnia, brain fog, and inflammation.
Usually, symptoms progress something like the following. Chronic stress causes ldysbiosis, which then leads to the tight junctions in the gut lining loosening, creating leaks. These leaks then allow toxins, pathogens, and food substances to enter your bloodstream.
These gut leaks affect your brain in two ways:
The first is that some of these substances can actually cross your blood-brain barrier. This puts your neurons in defense mode and activates your brain’s specialized immune cells, the microglia.
 This immune response in your brain will cause what all immune responses cause, inflammation. It does so mainly via the inflammatory cytokines the microglia secrete to coordinate their activity. Neuroinflammation, like all inflammation in the body, is an important and necessary defense mechanism. But just like all types of inflammation, when it becomes chronic, it wreaks havoc on your health.
This immune response in your brain will cause what all immune responses cause, inflammation. It does so mainly via the inflammatory cytokines the microglia secrete to coordinate their activity. Neuroinflammation, like all inflammation in the body, is an important and necessary defense mechanism. But just like all types of inflammation, when it becomes chronic, it wreaks havoc on your health.
The second way these substances affect your brain is by triggering a localized immune response in your gut. In fact, most inflammation begins in the gut. It’s the biggest interface we have with the environment, as we assimilate what we ingest there. But a localized immune response will create inflammation, and if that inflammation in the gut turns chronic, it will spread.
Inflammation that spreads to the skin causes skin problems. If it reaches the joints, it causes joint pain. And if it reaches the brain, it causes neuroinflammation. Chronic low-grade inflammation has been theorized as a significant contributor to anxiety, depression, brain fog, and other mental and cognitive health issues. That’s why nutrition for brain health has taken a forefront in the effort to resolve the mental health crisis. At least by functional medicine and holistic health practitioners. It can be essential in helping to reduce these levels of inflammation.
Now you have an idea about how chronic stress affects your Neuroaffect Circuit and how it can lead to cognitive decline and psychiatric issues. The next thing to understand is how one of the best ways to combat these negative effects is through diet.
The traditional Mediterranean diet is the diet that’s been studied the most when it comes to overall health benefits as well as specifically for nutrition for brain health. The studies on it show that it can be protective against our biggest killers: cancer, diabetes, and cardiovascular disease. And it seems to be quite effective in reducing chronic inflammation.
Specifically, its nutrition for brain health has been correlated with a reduction in the risk of cognitive impairment, Alzheimer’s disease, and dementia. It’s also been shown to actually improve cognitive function.
It is also one of the easiest diets to adopt if you’ve been eating the Standard American Diet. It’s not very restrictive, and it has room for a lot of what you're used to. But generally speaking, it is mostly whole-foods based, mostly vegetarian, and mostly seasonal.
It’s high in extra virgin olive oil, legumes, fruits, vegetables, nuts, seeds, whole grains, and fish. It has a moderate amount of yogurt, wine, and cheese. And meat, eggs, and other animal products are eaten occasionally, and never as the central component of a meal. It contains very few processed foods, if any.
This diet also most closely resembles the adrenal fatigue diet, the diet we most frequently recommend for AFS and other health issues. The main difference is that the adrenal fatigue diet recommends avoiding gluten and alcoholic beverages, at least until most health issues have subsided.
 The MIND diet stands for Mediterranean-DASH Intervention for Neurodegenerative Delay. It combines elements of the Mediterranean diet with the DASH diet. DASH stands for Dietary Approaches to Stop Hypertension. MIND was developed after researchers noticed how both of these diets were associated with better cognitive health in the elderly. And the more these elderly people adhered to the diets, the better their outcomes.
The MIND diet stands for Mediterranean-DASH Intervention for Neurodegenerative Delay. It combines elements of the Mediterranean diet with the DASH diet. DASH stands for Dietary Approaches to Stop Hypertension. MIND was developed after researchers noticed how both of these diets were associated with better cognitive health in the elderly. And the more these elderly people adhered to the diets, the better their outcomes.
After it was developed, researchers studied its effects on cognitive health in older adults. And they found that it may be even more protective against cognitive decline than the Mediterranean diet alone.
Since you already have an idea of what the Mediterranean diet is, let’s take a look at DASH and how it is included in the MIND diet.
With DASH, the focus is on the following principles:
What that ends up looking like is a diet full of fruits, vegetables, legumes, beans, whole grains, and lean proteins. So far, it sounds similar to the Mediterranean diet. But there are certain extra restrictions. First of all, dairy has to be low-fat or fat-free. It also limits oil intake, including olive oil, to 2-3 teaspoons a day. It also really focuses on reducing sodium intake. And, lastly, the other big difference is that the DASH diet has specific recommendations of what to eat on a daily and weekly basis.
The MIND diet is a combination of the two diets, and its specific recommendations are to include:
It also recommends to reduce:
The KetoFlex 12/3 diet is a special ketogenic diet. It was developed by Dr. Dale Bredesen and is part of the Bredesen Protocol. It’s mildly ketogenic and mainly plant-based, unlike the more mainstream ketogenic diets. It also incorporates a form of intermittent fasting. Of all the diets mentioned, it is the most restrictive, yet it does have some specific advantages that the others don’t.
First of all, the focus of this diet is not so much about going into full ketosis. It’s more about developing what’s called metabolic flexibility. The ability to easily shift from glucose to fat metabolism. It’s milder as well because it does allow for more carbohydrate intake than the typical ketogenic diet.
 The intermittent fasting is also a little different than your typical 16/8 or 18/4 (fasting/eating) windows. Here, the fasting total is for 12 hours and the 3 stands for fasting 3 hours before bed. So let’s say your bedtime is at 10 p.m. That means you stop eating at 7 p.m., go to sleep at 10 p.m., and can eat again at 7 a.m.
The intermittent fasting is also a little different than your typical 16/8 or 18/4 (fasting/eating) windows. Here, the fasting total is for 12 hours and the 3 stands for fasting 3 hours before bed. So let’s say your bedtime is at 10 p.m. That means you stop eating at 7 p.m., go to sleep at 10 p.m., and can eat again at 7 a.m.
As for what you actually eat, the biggest percentage is given to non-starchy vegetables and healthy fats. Fats from avocados, coconut oil, and olive oil are all good sources. Next, a smaller percentage is given to resistant starches, fatty fish, and low glycemic index fruits (such as berries). And, finally, you’re allowed a few indulgences once in a while, like dark chocolate or a glass of wine.
You need to avoid simple carbohydrates, processed foods, sweets, gluten, dairy, starchy vegetables, artificial sweeteners, food additives, and preservatives.
The KetoFlex diet was developed with Alzheimer’s disease (AD) in mind. And it was created because of the following observations:
But instead of having the goal of constantly bypassing these impaired glucose metabolism pathways, the KetoFlex diet just aims to offer metabolic flexibility. That way, those affected can easily switch back and forth between glucose and ketones while maintaining their cognitive health. Truly, this flexibility is one of the greatest assets to gain from focusing on nutrition for brain health.
The adrenal fatigue diet is similar to the Mediterranean diet in many respects. The main differences are that, in the adrenal fatigue diet, you should avoid gluten and alcohol intake until you are well on your way to recovery.
Compared to the DASH part of the MIND diet, the adrenal fatigue diet aims for the opposite when it comes to sodium and potassium. This electrolyte balance is switched in AFS, with too much potassium and not enough sodium. So, we actually advise our clients to limit their potassium and even sometimes add extra sodium.
As for the KetoFlex diet, the main difference is that we don’t try for ketosis with the adrenal fatigue diet. We also do not recommend any kind of fasting until your recovery is complete. That’s because, with AFS, your body is already quite depleted of not just nutrients, but energy stores. And, with AFS, you’re more at risk of hypoglycemic episodes. Instead, we advocate for eating every 3-4 hours.
The ideal eating schedule looks like this:

Overall, the adrenal fatigue diet is made of:
It’s important to note that these are general guidelines. Each person’s diet should be individualized to their condition and needs. That's actually the main bulk of our work with our clients, understanding their condition and needs to be able to customize their recovery protocol. That protocol includes diet as well as supplements, exercise, stress management tools, and sleep hygiene practices. If you’d like to learn more about how we approach nutrition for brain health and adrenal fatigue recovery, you can get in touch for a free initial consultation with one of our coaches.
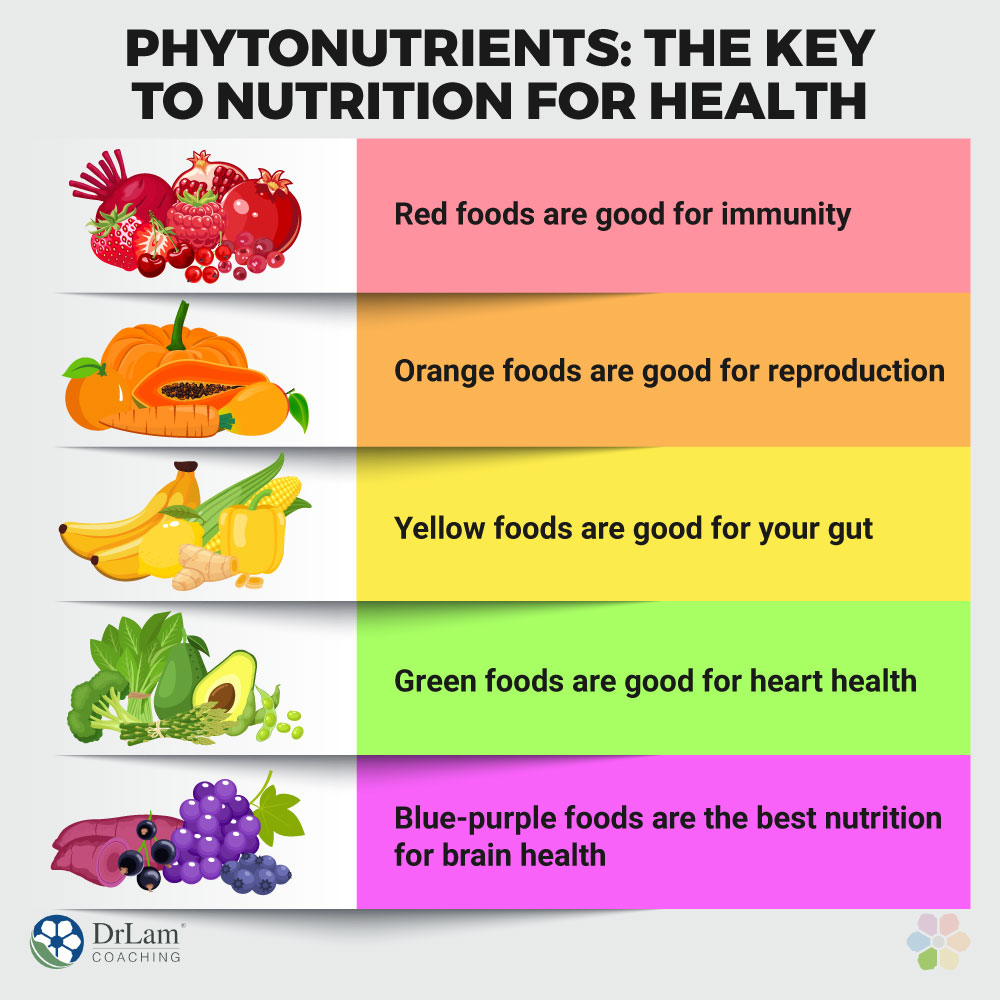
You’ll have noticed that all the diets above are mainly composed of plants. This includes the KetoFlex, even though more traditional ketogenic diets mainly focus on animal products and fats. This is because of the protective quality of phytonutrients. Phytochemicals in plants have specific benefits, and, interestingly enough, the color of plant foods can tell you about the types of benefits they provide.
And, don’t forget, plant foods here are not just limited to fruits and vegetables. Herbs, spices, nuts, seeds, and flowers are included too. Herbs and spices are especially useful as possible replacements for any artificial flavors or condiments you’re used to.
Neurodegeneration and cognitive decline can be hereditary. But that doesn’t mean that if you have a family history, you are doomed. Through strategic dietary and lifestyle changes, you can use the power of epigenetics to your advantage. You can keep disease genes switched off. And while mainstream medical treatments for these conditions are still quite limited, the potency of food and nutrition should not be underestimated.
Four diets are especially helpful for protecting your brain and cognitive function: the Mediterranean, the MIND, the KetoFlex 12/3, and the adrenal fatigue diets. Each one is different and has a different mode of action, but they all have two main things in common: they fight inflammation and they utilize the power of phytonutrients. That’s why they contain such a large percentage of plant-based foods.
Some of these diets are more restrictive than others. But with the right guidance and support, you’ll be able to fundamentally change the way you eat and the way you live without too much hassle. You can be healthier than you’ve ever been before. If you need help, you can get in touch with us for a free initial consultation. We’ll discuss your options and goals, as well as how we might be able to support you.
The power of food is not to be underestimated when it comes to cognitive function. But some strategies and diets count as the best nutrition for brain health. We cover those in detail in this article and offer tips on how to get started.
