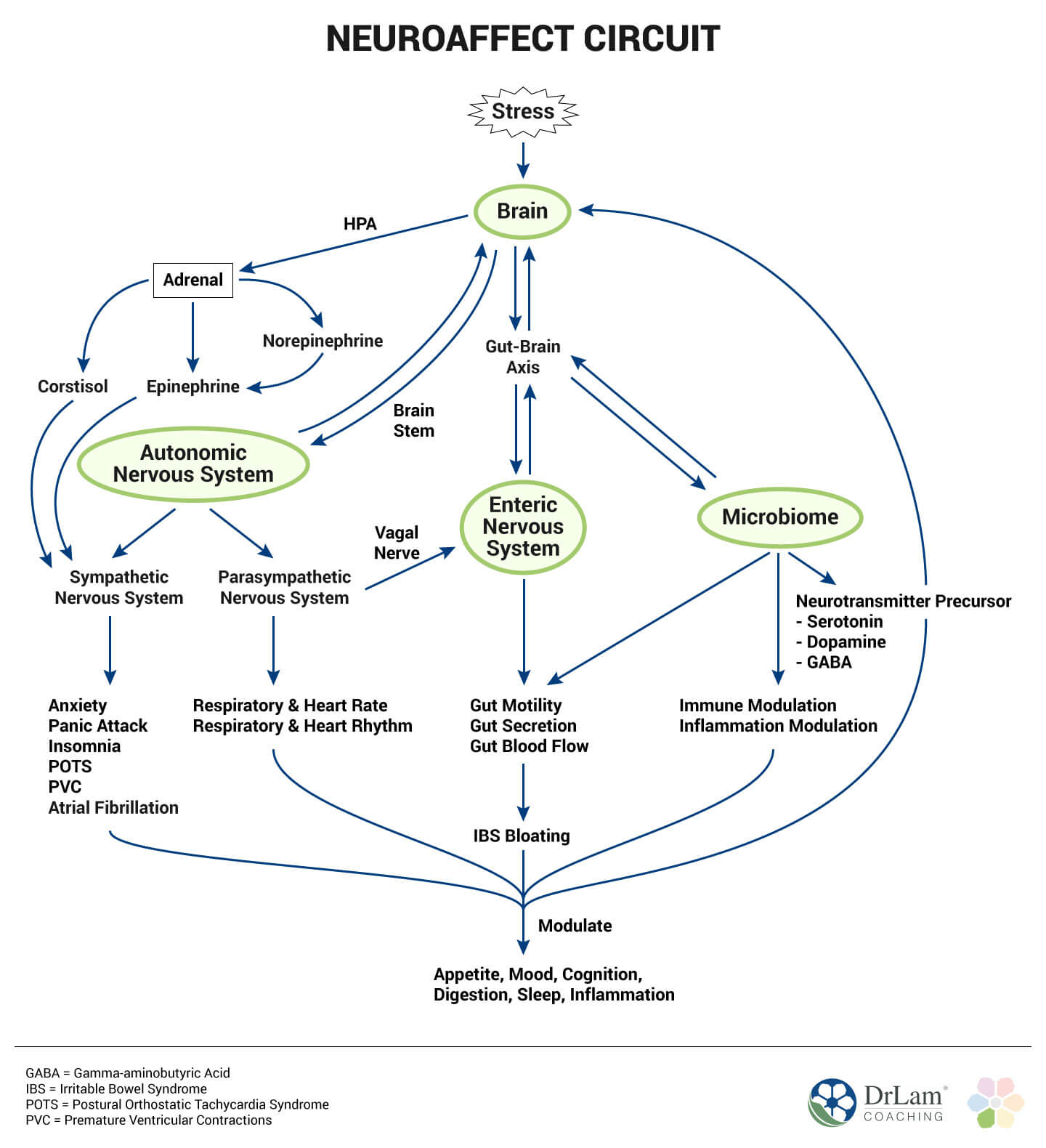
 Our body has an internal built in mechanism to handle stress. It is called the NeuroEndoMetabolic Stress Response. This is a biochemical orchestra that consists of 6 biological circuits, with 3 associated physiological systems within each. Each circuit plays a critical role in neutralizing stress when it arrives at our doorstep. Collectively, they work together to keep our body operating optimally. The six circuits are the hormonal, cardionomic, neuroafect, inflammation, detoxificaiont, and bioenergetics circuit. The Neuroaffect circuit of the NeuroEndoMetabolic (NEM) Stress Response model is composed of the brain, autonomic nervous system, and the microbiome. A combination of neurological and affective parts, it is not neuropsychiatric in nature. Rather, it describes the biological aspects of any mental health issues. This triad of gut-brain-autonomic nervous system uses neurotransmitters as its means of communication.
Our body has an internal built in mechanism to handle stress. It is called the NeuroEndoMetabolic Stress Response. This is a biochemical orchestra that consists of 6 biological circuits, with 3 associated physiological systems within each. Each circuit plays a critical role in neutralizing stress when it arrives at our doorstep. Collectively, they work together to keep our body operating optimally. The six circuits are the hormonal, cardionomic, neuroafect, inflammation, detoxificaiont, and bioenergetics circuit. The Neuroaffect circuit of the NeuroEndoMetabolic (NEM) Stress Response model is composed of the brain, autonomic nervous system, and the microbiome. A combination of neurological and affective parts, it is not neuropsychiatric in nature. Rather, it describes the biological aspects of any mental health issues. This triad of gut-brain-autonomic nervous system uses neurotransmitters as its means of communication.
The autonomic nervous system, consisting of multiple branches of the sympathetic nervous system (SNS), the adrenomedullary hormonal system (AHS), and the parasympathetic nervous system (PNS), works without conscious control to regulate a number of body systems.
The SNS comes into play when stress is mild and works to gear the body up to deal with stress. The AHS becomes activated when stress is more severe. The PNS serves to help the body slow down, rest, and recuperate from stress effects.
The “fight or flight” response is triggered when the body comes under stress from any source. This is the function of the SNS. Norepinephrine is the neurotransmitter used most often with mild or moderate stress. With increasing stress, the AHS is triggered to respond and epinephrine, a more potent neurotransmitter, is released. Ideally, once the stress is dealt with, the PNS is triggered to help the body rest and recover from the effects of stress.
However, in the current social climate stress is often continuous. This stimulates the AHS to continue releasing epinephrine, which puts a heavy burden on the adrenal glands to produce more and more cortisol to fight the stress. Eventually, the adrenals become exhausted and unable to produce sufficient cortisol. This is adrenal fatigue.
A problem that soon occurs here is that there is no hormone that counters epinephrine. Thus, the more the AHS releases, the more that is produced. This leads to significant physical problems such as panic attacks, a sense of impending doom, and a literal burn-out in the body.
The increased activity of the sympathoadrenal system (SAS) can trigger a Reactive Sympathoadrenal Response (RSR) in which a flood of epinephrine is released into the system. A flood of norepinephrine is called a Reactive Sympathetic Overload (RSO), also called Sympathetic Overload (SO).
SO is not as intense as RSR, because of the different level of epinephrine in the latter. However, both result in symptoms related to an activation of the body to deal with stress.
Two of the more challenging of these symptoms are sleep disorders and dysregulation of your biological clock.
 Good quality sleep is necessary for recovery from stress. However, with Adrenal Fatigue Syndrome (AFS) flooding the body with both norepinephrine and epinephrine, it is very difficult to get good sleep. This sleep deprivation then becomes another stressor on the body and begins the stress response all over again. When cortisol levels rise with the onset of the stress response, epinephrine levels also rise. These two chemicals lead either to sleep onset sleeplessness or sleep maintenance sleeplessness.
Good quality sleep is necessary for recovery from stress. However, with Adrenal Fatigue Syndrome (AFS) flooding the body with both norepinephrine and epinephrine, it is very difficult to get good sleep. This sleep deprivation then becomes another stressor on the body and begins the stress response all over again. When cortisol levels rise with the onset of the stress response, epinephrine levels also rise. These two chemicals lead either to sleep onset sleeplessness or sleep maintenance sleeplessness.
Sleep is affected by a number of other hormones as well. DHEA is released by the adrenals and converted into cortisol. As more DHEA is converted into cortisol, its level decreases, possibly stimulating the release of norepinephrine which inhibits your ability to sleep. Melatonin is negatively affected by cortisol and light. This is the hormone which helps instigate sleep.
The biological clock works to regulate the rhythms of the body, including the circadian rhythm. A number of factors affect the biological clock. Neurotransmitters affect the information coming into the brain that affects the biological clock, work within it, and influence its output. Likewise, the biological clock regulates neurotransmitters. If the biological clock is disrupted, neurotransmitters can become imbalanced.
A large number of neurotransmitters and hormones affect the functioning of the biological clock. Low levels of serotonin and melatonin, an imbalance of these two chemicals, high levels of cortisol, a lack of GABA, high levels of catecholamines, excess histamine, and excess glutamate are some of the imbalances that can affect the biological clock.
As is only common sense, a healthy brain is necessary for a healthy body. High levels of cortisol, as are seen in AFS in the early stages, has a negative effect on the brain. Several notable chemicals play an important part in brain health.
Imbalanced neurotransmitters can lead to very significant health problems. There are many ways this kind of imbalance can occur. Some of those ways include poor dietary choices, toxins that are ingested or found in the environment, genetics, dysfunctional bowels, and especially chronic stress.
The ‘wired and tired’ phenomenon is often encountered with AFS. It is a result of the continuing flood of excitatory neurotransmitters such as norepinephrine and epinephrine in the body and the feeling of exhaustion common to AFS. The body is tired but still in a state of arousal.
The microbiome of the human body is home to multiple trillions of organisms. As long as they work in balance, the gut functions well. However, an imbalance brought on by chronic stress can lead to multiple physical issues.
It is important to keep in mind the connection and communication between the gut and the brain that takes place primarily through the vagus nerve. This communication is two-way, and any imbalance or dysfunction in one system affects the other.
 Dysbiosis in the gut is any change in the makeup of the flora in the gut that is away from the normal diversity and stability found there. This kind of dysbiosis can lead to leaky gut in which the junctions between the epithelial cells lining the small intestine become loose, allowing bacteria and other pathogens access to the bloodstream and the rest of the body. The result is a triggering of the immune process and significant inflammation. Inflammation originating in the gut has been theorized to be a cause of mental health issues.
Dysbiosis in the gut is any change in the makeup of the flora in the gut that is away from the normal diversity and stability found there. This kind of dysbiosis can lead to leaky gut in which the junctions between the epithelial cells lining the small intestine become loose, allowing bacteria and other pathogens access to the bloodstream and the rest of the body. The result is a triggering of the immune process and significant inflammation. Inflammation originating in the gut has been theorized to be a cause of mental health issues.
Whatever the cause, however, the microbiota has been shown to have massive effects on mental health as well as physical health. Several serious disorders such as depression, anxiety, and even autism spectrum disorder have been linked to dysbiosis of the gut.
Gut dysbiosis can lead to several serious physical changes in the gut as well. Irritable bowel syndrome, inflammatory bowel disease, colorectal cancer, atherosclerosis, obesity, and Type 2 diabetes are some of these changes.
Cytokines produced in the gut have been found to influence sleep. Likewise, disrupted sleep has been shown to increase the presence of pro-inflammatory cytokines.
And all of these interconnections point to how problems in the Neuroaffect circuit can be worsened by stress.
Stress, either acute or especially chronic, affects brain functioning. Some of these effects are a result of long-term exposure to stress hormones. Higher than normal levels of stress hormones affect the brain centers responsible for regulating emotional response and cognitive abilities. This can lead to inaccurate and distorted perceptions of the world that can lead to inappropriate emotional responses.
 Stress can also bring on some significant physical changes to the brain. Learning difficulties come from increased myelin in the hippocampus. There is an increased stroke risk with chronic stress due to changes in blood pressure. A greater risk of developing depression comes as a result of the effects of inflammation generated by chronic stress. Shrinking of the medial prefrontal cortex has been seen as a result of a loss of gray matter. Increases in white matter as a result of stress leads to increased difficulty in neurons making connections with each other.
Stress can also bring on some significant physical changes to the brain. Learning difficulties come from increased myelin in the hippocampus. There is an increased stroke risk with chronic stress due to changes in blood pressure. A greater risk of developing depression comes as a result of the effects of inflammation generated by chronic stress. Shrinking of the medial prefrontal cortex has been seen as a result of a loss of gray matter. Increases in white matter as a result of stress leads to increased difficulty in neurons making connections with each other.
The autonomic nervous system suffers from the effects of stress also. Under normal conditions, the SNS and PNS work in balance to keep the body functioning well. With chronic stress, however, the SNS continues to be stimulated, keeping the body in a fight or flight response. If the stress becomes severe, the AHS may begin releasing epinephrine to give the body the energy needed to fight stress. Under these conditions, the PNS never has the opportunity to slow the body down for rest and recovery.
Stress affects the microbiome in a number of ways also. It can lead to leaky gut, an immune response, and high inflammation levels. Stress can cause an imbalance of the bacteria in the microbiome. Small intestine bacterial overgrowth may occur, leading to serious problems with digestion. A slowing of gut motility also leads to serious problems with digestion and absorption of nutrients.
The connection between changes in the gut microbiome and adrenal fatigue are clear. Many of the factors that affect the microbiome also affect adrenal fatigue. The inflammation and increase in the bad bacteria in the gut can lead to systemic problems as well as problems in the GI tract. The increase of inflammation further disrupts the microbiome and causes problems with absorption of nutrients. As the body is deprived of nutrients, it weakens. For people with AFS, already in a weakened condition, this is very serious.
The effects of stress on the gut-brain axis is just beginning to be investigated. Likewise, diet and the effects of the early development of the microbiota are also being investigated for their effects on later physical health.
However, it is clear that stress can have serious effects on the Neuroaffect circuit by worsening existing issues and creating new ones. While it is possible to address these issues with diet, lifestyle changes, and a health improvement plan, it helps to be aware of early symptoms as they appear.
When the Neuroaffect circuit is dysfunctional, there are several symptoms that can result.
 The Neuroaffect circuit is composed of the brain, microbiome, and the autonomic nervous system, and each of these three work together and can be seriously affected by stress. Imbalances in one of these systems can create imbalances in essential hormones and neurotransmitters that seriously affect the others, as well as the rest of your body.
The Neuroaffect circuit is composed of the brain, microbiome, and the autonomic nervous system, and each of these three work together and can be seriously affected by stress. Imbalances in one of these systems can create imbalances in essential hormones and neurotransmitters that seriously affect the others, as well as the rest of your body.
There are steps you can take to care for and gently rebalance Neuroaffect circuit problems. However, it is a good idea to seek care from a professional who understands how these organs work together holistically. Benzodiazepines are often given by medical professionals to help a person deal with the effects of a dysfunctional Neuroaffect circuit. There are many dangers to this. Addiction is one of the most frequent. Avoiding this type of medication in favor of more natural methods is often a better option, but every body is different, and it is important to seek out what is best for yours individually.
Symptoms of dysregulation in the Neuroaffect circuit include anxiety, depression, difficulty falling asleep or staying asleep, feelings of impending doom, reduced cognitive health, and more. Dysregulation in hormone and neurotransmitter production can cause widespread issues, so it is important to get help if you suspect this is a problem for you.