 Dysautonomia, a genuine nervous system disorder, involves surges of adrenaline that can result from a variety of triggers. These surges speed up your entire body and give the disorder its name: Adrenaline dysautonomia.
Dysautonomia, a genuine nervous system disorder, involves surges of adrenaline that can result from a variety of triggers. These surges speed up your entire body and give the disorder its name: Adrenaline dysautonomia.
This sudden dumping of adrenaline (also known as epinephrine) into your body can happen at any time but frequently happens at night. Triggers consist of anything that normally sends a thrill of some kind through your body: Loud music, getting frightened, or even having a dream in which you’re very active.
But triggers don’t always play a part in the onset of adrenaline dysautonomia.
As a general term, "dysautonomia" refers to a number of conditions that involve a dysregulation of the involuntary nervous system. This kind of dysregulation often involves the Cardionomic and Hormonal circuits of the NeuroEndoMetabolic (NEM) Stress Response, the global system your body uses to deal with stress.
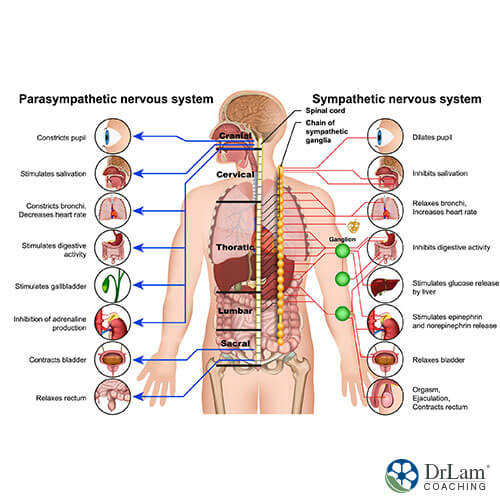
As part of the Cardionomic circuit of the NEM, the autonomic nervous system (ANS) contains two components: the sympathetic nervous system (SNS) and parasympathetic nervous system (PNS). The SNS speeds up your body in response to stress while the PNS allows your body to calm down after stress leaves.
Normally, these two parts of the ANS work together in balance to maintain homeostasis in your body. Therefore, this balance helps you respond adequately to stress and to recover from it.
In adrenaline dysautonomia, an excessive sympathetic nervous system response and an underactive parasympathetic nervous system response comes into play. When this condition occurs, most of the time the sympathetic nervous system continues to be dominant while the parasympathetic nervous system seldom becomes active. Consequently, this condition describes sympathetic dominance.
In essence, your stress response continues to be active day after day. It keeps you in the ‘fight or flight’ response common to your innate stress reaction. A significant part of this response consists of the flood of adrenaline throughout your body.
As your body continues in this revved-up state, a number of degenerative health conditions can develop. These develop because this state of being should only persist for short periods of time as your body deals with significant stress.
Three primary hormones should receive attention when discussing adrenaline dysautonomia. Cortisol, noradrenaline (norepinephrine), and adrenaline (epinephrine) make up your hormonal response to stress. These three hormones are released by your adrenal glands and brain in the face of stress.
When the hypothalamic-pituitary-adrenal (HPA) axis becomes stimulated by stress, your adrenal glands release cortisol first to combat the effects of stress. As long as stress remains mild, cortisol usually takes care of it.
 However, if stress continues and the adrenals can no longer produce and release sufficient cortisol, noradrenaline comes into play. Noradrenaline, produced in the brain, works to make you more alert, more active, and more ready to deal with stress.
However, if stress continues and the adrenals can no longer produce and release sufficient cortisol, noradrenaline comes into play. Noradrenaline, produced in the brain, works to make you more alert, more active, and more ready to deal with stress.
Unfortunately, people who suffer from Adrenal Fatigue Syndrome (AFS) experience the fatigue that comes with the condition. When noradrenaline hits the body, it speeds you up, producing the ‘wired but tired’ sensation that AFS sufferers know so well.
With continuing and increasing stress, noradrenaline may not adequately handle chronic stress. Because of this, adrenaline comes into play. Adrenaline is the most potent stress-fighting hormone that is released from the adrenals. Therefore, it remains under tight control because of this potency.
Only if both cortisol and noradrenaline no longer can sufficiently deal with stress will the adrenomedullary hormonal system (AHS) become super-aroused and release a flood of adrenaline into your body.
This flood of adrenaline (reactive sympathetic response or RSR, also known as adrenaline dominance) can become the reason behind adrenaline dysautonomia. Adrenaline is a very powerful vasoconstrictor, and when it floods your body, it overpowers all other hormones. It signals that your body now exists in an emergency state.
Your body senses this due to the presence of the last weapon it uses to deal with stress. No other hormones or biochemicals work to oppose adrenaline. So, once adrenaline hits your body, its only counter is a series of metabolic steps that take time to work. This lies behind its use as a last resort in dealing with stress. However, one clinical use suggests intravenous norepinephrine can act as a counter to excess adrenaline.
If this release of adrenaline becomes dysregulated and continues, it can become the foundation for adrenaline dysautonomia and the serious health conditions that result.
Much of the time, dysautonomia results from a number of causes, many of them linked to other health conditions. If the dysautonomia is primary, it most often results from an inherited condition or from a degenerative illness condition. However, dysautonomia can also come from an injury or excessively stressful situation.
Some of the more common conditions that may prove triggering for dysautonomia include:

Severe stress or trauma occurring early in life can lead to irreversible, permanent damage to your stress response system. This kind of very significant trauma can cause your stress circuits to constantly stay in a hypersensitive state and can lead to a continual condition of sympathetic dominance for your entire life.
Some of the events and circumstances that may bring on this kind of trauma include:
Any or all of these events, or any like them, can lead to a high risk of developing adrenaline dysautonomia.
As with causes, the symptoms of adrenaline dysautonomia can vary depending on the individual. Often, these symptoms appear internally more than externally. However, there are some common symptoms that occur among most people with dysautonomia. All of these can defy prediction, vary in severity, and come and go.
Some of these common symptoms include:
In AFS, these two terms describe what happens with excessive noradrenaline (RSO, also known as adrenaline dominance) and adrenaline (RSR). These two conditions typically occur in stage 3 of AFS where both fatigue and stress continue to build. At this time, the sympathoadrenal system (SAS) really increases its activity and releases both noradrenaline and adrenaline.
Some major differences exist between RSO and RSR. For example, RSO is somewhat less intense than RSR because of the presence of an overload of adrenaline in the latter. You may feel your heart pounding with RSO, but the heartbeat remains regular. On the other hand, RSR can bring with it PVCs, atrial fibrillation, and tachycardia.
Many of the symptoms encountered with both RSO and RSR can stay subclinical and thus hard to detect. Some of these symptoms include the following:
Much of the time, the irregular heart rate becomes the first ‘real’ clinical sign that conventionally-trained medical professionals see. This leads them to focus on your heart as the body organ of most importance. Thus, they miss the bigger picture of all that happens with adrenaline dysautonomia.
Considering the effects of excessive adrenaline on the heart, it comes as no surprise that most medical professionals will focus here. The excess adrenaline that forms the basis for adrenaline dysautonomia affects the cardiac nodes, the ‘spark plugs’ of the heart that regulate heartbeat. This makes your heartbeat irregular, resulting in PVCs, unstable blood pressure, idiopathic supraventricular tachycardia, and atrial fibrillation.
These cardiac nodes control the timing of your heartbeat. Their firing must continue at a regulated rate in order for your heart to properly fill with blood and then eject that blood out to the periphery of your body.
 In cases of adrenaline dysautonomia, the excessive amount of adrenaline in your body disturbs this timing, making it much too fast. This reduces the amount of blood that enters your heart and thus the amount that is ejected into your body to carry oxygen and nutrients. Circulation to the periphery becomes compromised, blood pressure becomes unstable, and you can feel dizzy or even faint.
In cases of adrenaline dysautonomia, the excessive amount of adrenaline in your body disturbs this timing, making it much too fast. This reduces the amount of blood that enters your heart and thus the amount that is ejected into your body to carry oxygen and nutrients. Circulation to the periphery becomes compromised, blood pressure becomes unstable, and you can feel dizzy or even faint.
Another issue that comes to the fore with adrenaline dysautonomia involves overstimulation of the cardiac nodes. Sustained overstimulation of this kind can lead to physical damage to the electrical nodes. This may lead to an irregular heartbeat. Very significant symptoms such as those listed above may result.
When your heart rate becomes much too fast, it can cause more reactive metabolites at the cellular level. Due to their inflammatory potential, these metabolites become corrosive to the cardiac nodes. A decompensatory cycle begins that ultimately leads to more instability.
Therefore, the dysregulation of these hormones that normally modulate the Cardionomic circuit affects other systems throughout the body. With adrenaline dysautonomia, your entire body is affected.
These difficulties with heart rhythm tend to appear late in the process of adrenaline dysautonomia, but they can bring very significant disruptions to the Cardionomic circuit. With this continuing disruption of the Cardionomic circuit, more severe symptoms emerge. Some of these symptoms include:
The condition attention deficit hyperactivity disorder, or ADHD, affects a significant number of children and adults. Many of them take medications designed to control symptoms. Some of the symptoms commonly encountered with ADHD include:
One interesting hypothesis regarding ADHD involves a variant in the COMT enzyme. This enzyme works to break down adrenaline and noradrenaline. A variance in this enzyme allows these hormones, along with dopamine, to stay around in the synapses of neurons longer. This could lead to the kinds of symptoms that typically describe ADHD.
Everybody experiences the kinds of small events that set in motion the process of your body dealing with the stress generated. This includes the release of the chemical family of catecholamines that adrenaline, noradrenaline, and cortisol belong to. But with the variance in COMT described above, the hormones meant to deal with stress can accumulate around neurons and make small stressors seem like emergencies.
Other factors can make the symptoms of ADHD, depression, and anxiety worse. Many of these other factors can stem from adrenaline dysautonomia. Poor or inadequate sleep heads the list. Deficiencies in nutrition, additives from processed foods, and poor digestion worsen these conditions. Also known to make cognitive issues worse are the toxins in our foods and in the environment. Likewise, food sensitivities, food allergies, and hormonal changes can bring on cognitive difficulties.
 With the medications typically prescribed to counter the symptoms of ADHD, the root cause may only retreat deeper. Most of these medications fall into the category of stimulants, so they may bring more burden to already-overburdened adrenal glands. Therefore, they can increase the stress that drives those suffering from AFS.
With the medications typically prescribed to counter the symptoms of ADHD, the root cause may only retreat deeper. Most of these medications fall into the category of stimulants, so they may bring more burden to already-overburdened adrenal glands. Therefore, they can increase the stress that drives those suffering from AFS.
In addition, the medications typically prescribed for ADHD symptoms increase the amount of noradrenaline in your brain. This causes you to become more alert, aware, and able to focus attention. Norepinephrine outside your brain speeds up your heart, dilates your pupils, makes you breathe faster, increases the strength of your muscle contractions leading to jitteriness, and makes you sweat.
As mentioned previously, increased norepinephrine is also the cause of that ‘wired and tired’ feeling you have with AFS. So, it’s important not to take these medications too close to bedtime if you want to sleep.
Sometimes, it becomes difficult to distinguish the rapid heartbeat you feel with POTS from that you feel with adrenaline surges. For example, if you were lying down and felt the tachycardia coming on quickly like when you have a panic attack (but without the anxious thoughts that precede a panic attack), you most likely experienced an adrenaline surge.
One of the symptoms of POTS is this kind of unexpected adrenaline surge or rush. This comes because of the hyperactive state of the sympathetic nervous system. Some other key symptoms include a lightheaded feeling when you stand up, a rapid heartbeat at the same time, inability to tolerate exercise, and problems regulating your body temperature.
A number of other symptoms from other parts of the body can come with POTS as well, making it hard to know whether what you feel may result from the condition. And not all people experience the same symptoms.
The random surges of adrenaline make life difficult. When these occur at night, as they so often do, they prevent the good night’s sleep that your body needs. In addition to the surges of adrenaline, feelings of anxiety keep many people awake. Once they do get to sleep, they go through bouts of tachycardia, sweating, and little times of awakening called microarousals. Consequently, these all contribute to sleeplessness and awakening in the morning no more rested than when you went to sleep.
All of these add to the sleeplessness that so often plagues people who suffer from AFS. The sense of fatigue becomes overwhelming.
Most of the time, POTS is considered secondary dysautonomia. In a majority of cases, high levels of autoimmune markers come with an examination of those with POTS. Thus, people with this condition are more likely to suffer from an autoimmune disorder than the general population, as well.
A condition called adrenal medulla hyperplasia occurs rarely. In fact, only 32 cases have been reported in the U.S. It happens when the middle part of the adrenal gland starts growing. However, the added tissue doesn’t change the shape of the adrenal gland, making the condition difficult to assess.
Causes of this condition include excessive stress from any source. This increased stress leads to more secretion of cortisol. In addition, increased secretion of adrenaline takes place.
This increase in adrenaline can cause significant effects on the cardiovascular system. Adrenaline particularly affects the heart in ways already mentioned above. The kind of increase found with adrenal medulla hyperplasia only adds to the effects of adrenaline secreted due to your body’s attempts at dealing with chronic stress. Therefore, it may add to the risk of adrenaline dysautonomia.
Common symptoms of adrenal medulla hyperplasia include:
Any kind of dysautonomia involves the autonomic nervous system. With adrenaline dysautonomia, sudden and unexpected surges of adrenaline can hit. These come because your sympathetic nervous system becomes hyperactive and the balancing parasympathetic nervous system becomes so inactive that it can’t function. Therefore, you stay activated almost all of the time.
The sympathetic nervous system is responsible for the ‘fight or flight’ reaction when faced with stress. Remaining constantly geared up for this stress response defines adrenaline dysautonomia. A number of events can function as triggers for the adrenaline surges that come with it.
Continuing in this state can lead to serious health conditions. These conditions result because the activation of your body by the sympathetic nervous system should only continue for a short time as a way of dealing with stress.
Dysautonomia typically comes from an inherited condition or due to a chronic illness condition. However, it also may derive from significant early childhood trauma that leaves your body’s stress circuits sensitized to any form of stress. As a result, this kind of trauma also may condition your sympathetic nervous system to remain ‘on’ all the time.
Symptoms of dysautonomia can vary in presentation and severity. They may come and go at random. Common symptoms include the inability to stand upright, dizziness or lightheadedness, chest pain, nausea, mood swings, fatigue, and weakness, among others.
The major reason behind adrenaline dysautonomia comes from the flood of adrenaline that hits your body when cortisol and noradrenaline no longer deal with stress adequately. Consequently, your body then releases its last and most powerful weapon to deal with stress: Adrenaline.
As stress continues, your sympathetic nervous system increases the amount of adrenaline in your body, leading to some significant symptoms, particularly in the cardiovascular system. Your heart rate increases and becomes irregular. Your blood pressure becomes variable. You sweat, get dizzy, maybe even faint.
 You may develop symptoms that appear like ADHD. However, these symptoms may come because of a variant in the COMT enzyme. This enzyme typically breaks down adrenaline and noradrenaline. So, if you have this variant and the enzyme doesn’t complete its task, the resulting pattern of symptoms can be mistaken for ADHD.
You may develop symptoms that appear like ADHD. However, these symptoms may come because of a variant in the COMT enzyme. This enzyme typically breaks down adrenaline and noradrenaline. So, if you have this variant and the enzyme doesn’t complete its task, the resulting pattern of symptoms can be mistaken for ADHD.
Another condition that can develop from adrenaline dysautonomia is POTS. The symptoms appear similar and may take a very close examination to differentiate. Random adrenaline surges tend to show up in people who suffer from POTS.
A rare condition called Adrenal Medulla Hyperplasia can also express symptoms similar to adrenaline dysautonomia. This condition results in a growth of cells in the medulla of your adrenal glands.
If you are suffering from adrenal dysautonomia, here are a few things you can do to help alleviate the situation:
If the root of this condition starts at the adrenals, it is imperative to focus on rebuilding and supporting the adrenals as the most effective way towards total recovery. This can often be done with Dr. Lam's Nutritional Adrenal Fatigue Recovery Program, which helps you identify your stage of adrenal fatigue along with educating you on how to recover from adrenal fatigue. It not only gives you all the information on what to eat, how to exercise, and what to expect in each stage of recovery, but it also provides 4 vital supplements that are key to adrenal fatigue recovery.
Whatever course of action you decide to take, however, please do so with the guidance of your healthcare professional who will assess the benefits of each one.
If you would like to know more about or need assistance with any choice you make regarding adrenaline dysautonomia, the team at Dr. Lam Coaching can help. We offer a free** no-obligation phone consultation where we will privately discuss your symptoms and various options.
Soothe Adrenaline: Adrenal Calm for Dysautonomia
Adrenaline dysautonomia occurs when the sympathetic nervous system becomes over-active, causing a flood of adrenaline throughout the body. It is similar to Reactive Sympathoadrenal Response in its symptoms. There may be triggers that set off the surge of adrenaline often experienced.