 Adrenal hyperplasia and adrenal fatigue syndrome, or AFS, share a number of symptoms, and they can be confused for each other without good assessment. It’s important for you to know the similarities and differences in order to inform your healthcare professional and so you can help yourself deal with symptoms.
Adrenal hyperplasia and adrenal fatigue syndrome, or AFS, share a number of symptoms, and they can be confused for each other without good assessment. It’s important for you to know the similarities and differences in order to inform your healthcare professional and so you can help yourself deal with symptoms.
This article will deal with non-classic congenital adrenal hyperplasia, or NCAH, and its relationship to AFS.
This form of adrenal hyperplasia is a fairly common autosomal recessive condition. It results from a 21-hydroxylase deficiency. Androgen excess is the most frequent clinical feature, instead of adrenal insufficiency with the classic form of the disorder. Females have this condition more frequently than males.
Clinical and research findings show this condition occurs in between 0.6% to 9% of women with excess androgen. Higher prevalence has been seen in some populations, including those of Ashkenazi Jewish, Mediterranean, Middle Eastern, and Indian heritage.
This condition is a milder form of congenital adrenal hyperplasia and has a later onset of symptoms. With this mild form, some people exhibit few, if any, symptoms. Many show an excess of the male hormone androgen. NCAH is caused by mutations in the CYP21A2 gene and is recessive.
Generally speaking, NCAH is one of the three forms of congenital adrenal hyperplasia. The other two types are known as simple virilizing adrenal hyperplasia and salt wasting adrenal hyperplasia.
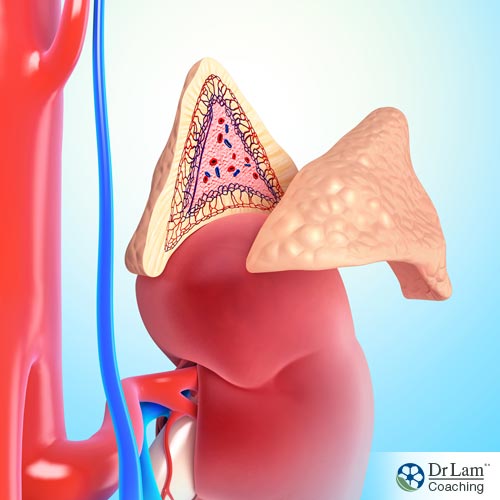
Congenital adrenal hyperplasia (CAH) affects the adrenal glands which produce several hormones, including corticosteroids, mineralocorticoids, and androgens. The first two of these hormones affect the body’s illness or injury response and the body’s salt and water levels, respectively. Androgens are the male hormones.
Enzyme deficiencies affect the adrenals’ ability to produce these hormones. A deficiency in the enzyme required for one of these hormones will result in an overproduction of the others.
A lack of 21-hydroxylase is the most common cause of CAH. Not having this enzyme prevents you from making cortisol and aldosterone, for salt-losing adrenal hyperplasia, and causes you to produce excess androgen. The excess of this male hormone will typically bring symptoms of abnormal sexual development.
CAH is the more severe form of this condition and is most often found early in life. If left unaddressed, adrenal crisis and even death may occur. There is no cure for CAH, but with appropriate care, sufferers can live a full life.
In the salt-wasting form of CAH, the body has trouble maintaining an appropriate level of salt in the blood. There is also a lack of cortisol and aldosterone produced by the adrenal glands. This form of CAH can result in shock, coma, or death if it isn’t found and remediated.
In the non-salt-wasting form of CAH, the shortage of the enzyme is not as severe. This shortage leads to sufficient levels of aldosterone, but insufficient cortisol production.
Those with CAH are much more likely to have adrenal fatigue than the general population. A person with CAH who comes under significant stress could easily progress much more quickly to the later stages of AFS due to natural low cortisol production.
Any time the body comes under stress no matter the source, the response is the same. The hypothalamic-pituitary-adrenal (HPA) axis is activated, resulting in the adrenal glands secreting cortisol, the stress-fighting hormone. If the stress continues, as it does so often in our stress-filled culture, ultimately adrenal fatigue will set in. This means the adrenals no longer can produce enough cortisol, and symptoms of AFS begin. Continuing stress leads to more and more symptoms. In the later stages of this condition, the person suffering from it may become bedridden.
Conventional physicians are not adequately trained to assess or remediate AFS. Their approach is to deal with individual symptoms or organs and suppress the symptoms to attempt relief. However, this is not adequate for AFS. Natural medicine practitioners who are trained in the NeuroEndoMetabolic (NEM) model of stress response will be enabled to assess how a person’s six major organ systems interact in the face of continuing stress. This interaction allows them to get to the root causes of the symptoms of AFS, and then put together a remediation plan that will not just control symptoms, but address these root causes.
The two forms of adrenal hyperplasia, congenital and non-classical congenital, have both common and different signs and symptoms.
To begin, there are those who show no signs or symptoms of NCAH.
With NCAH, the symptoms typically are related to excess androgen.
 Children who are assessed with this condition often will exhibit early signs of puberty such as growing pubic hair, underarm hair, and body odor. These signs may occur as early as 8 or 9 years of age.
Children who are assessed with this condition often will exhibit early signs of puberty such as growing pubic hair, underarm hair, and body odor. These signs may occur as early as 8 or 9 years of age.
Other signs of NCAH in children include greater height, faster growth, and faster maturation of skeletal bones. In girls, there may be an enlarged clitoris, while boys may show an enlarged penis. The increased maturation of the skeleton may lead to early epiphyseal fusion, resulting in shorter adult height.
Females are more often assessed with this condition in adolescence and adulthood. Much of this is due to the abundance of adrenergic symptoms. Typical symptoms include hirsutism, acne, hair loss, loss of ovulation, and menstrual dysfunction. One large study showed the most common symptoms to be hirsutism, followed by light or infrequent menstrual periods, and acne.
Another study that investigated women with NCAH showed the most common presenting symptoms to be hirsutism, difficulty with menstruation, and reduced fertility.
As mentioned before, not all people with NCAH exhibit symptoms. A large genetic study of 330 family members showed a distribution of symptomatic versus non-symptomatic individuals. Of these subjects, nine were seen to have symptoms, and 42 individuals were asymptomatic but were affected by NCAH. The largest number, 242, were heterozygotic carriers. Out of the entire subject cohort, 37 were not affected by NCAH.
In that same study, the majority of males were not symptomatic. Most of the time, they were assessed only after a female in the family was determined to have NCAH.
The most frequent presenting symptom in women was lack of menstruation, either primary or secondary. Also seen frequently in women were chronic lack of ovulation and infertility. A similarity with polycystic ovary syndrome (PCOS) was also evident. Approximately half of women with NCAH will show physical changes in line with PCOS.
Fertility can be an issue in women with NCAH. The issue is not necessarily infertility, but subfertility. This comes due to the problems with ovulation often seen in adrenal hyperplasia.
Classical congenital adrenal hyperplasia in women appears to bring on increased levels of progesterone that interfere with the menstrual cycle and fertility. Elevated levels of progesterone may also be seen in women with NCAH. This leads to decreased quality of mucus in the cervix that can interfere with penetration by sperm and thus can cause infertility. In the follicular phase of the menstrual cycle, increased 17-OHP (a steroid hormone related to progesterone) or P4 (another steroid hormone related to progesterone) can lead to difficulties in the maturation of the endometrium and to difficulty with implantation of the embryo.
There are several risk factors for metabolic disorder seen in women with non-classic congenital adrenal hyperplasia. Insulin resistance, obesity, and high blood pressure are included in these risk factors. High androgen levels complicate issues contributing to atherogenic lipid profiles and thus increase the risk of metabolic disorders. Insulin sensitivity has been shown through research to be present in women with NCAH who are not obese. Much of the research into insulin sensitivity has resulted in mixed findings and typically use women with classical CAH as subjects.
© Copyright 2018 Michael Lam, M.D. All Rights Reserved.
Adrenal hyperplasia and AFS share similar symptoms. In both CAH and NCAH, lower cortisol is problematic. In AFS, lower cortisol leads to significant problems. In CAH, lower cortisol leads to increased ACTH and continued pressure on the adrenals. In AFS, the adrenals are pressured to exhaustion and the development of symptoms. With adrenal hyperplasia, the enzymatic process that supplies hormones to the adrenals is insufficient, and AFS is more likely.