 When you’re sick, the impulse is to do what you can to feel better before trying to figure out the cause for your ailment. Sometimes this resolves your symptoms and the problem goes away, but, just as often, it means that the underlying issues go unaddressed and get worse. The body is a series of connected circuits and organs, so when something goes wrong in one part of the body, it naturally causes problems with others as well. Medical research seems to be catching up with this idea and has unearthed a link between infections and mental illness that could have far-reaching implications for your mental and physical health. So if you suffer from one or the other, it’s worth looking for a deeper cause to stop the cycle.
When you’re sick, the impulse is to do what you can to feel better before trying to figure out the cause for your ailment. Sometimes this resolves your symptoms and the problem goes away, but, just as often, it means that the underlying issues go unaddressed and get worse. The body is a series of connected circuits and organs, so when something goes wrong in one part of the body, it naturally causes problems with others as well. Medical research seems to be catching up with this idea and has unearthed a link between infections and mental illness that could have far-reaching implications for your mental and physical health. So if you suffer from one or the other, it’s worth looking for a deeper cause to stop the cycle.
Around 43.8 million adults in the US suffer from some type of mental illness in any given year. This is around 1 in 5 adults, with 1 in 25 adults experiencing a severe mental illness that interferes with their daily activities. As if this wasn’t bad enough, the statistics are even worse for young people. Around 1 in 5 youths aged 13-18 will experience a severe mental illness at some point in their lives. And these are truly terrifying statistics.
There are several different types of mental illnesses, each with their own pathology, symptoms, and issues. Some of the most common are:
Mental illness can have a devastating effect on your life. It causes high rates of homelessness, with around 26 percent of homeless adults living with a severe mental illness. It also has implications for the criminal justice system, with approximately 20 percent of state prisoners suffering from a mental illness and a staggering 70 percent of youths in the justice system. It increases your chances of suffering from chronic medical conditions and increases your chances of early death from other, treatable medical conditions. In fact, adults with an untreated medical illness die an average of 25 years earlier than those without.
These are sobering statistics and highlight the importance of research and development of strategies for recovery from mental illness. And this is why the new research linking infections and mental illness is so important.
A recent study has shown that there’s a strong link between infections and mental illness. The researchers gathered data on hospitalizations and prescriptions for over a million children between January 1st, 1995 and June 30th, 2012. This study, located in Denmark, then used two national registries to determine which hospitalizations were due to severe infections and to identify prescriptions given on an outpatient basis for less serious infections. Both of these types of infections are very common in the general population. More severe infections include pneumonia and less severe infections include fungal infections.
Only about four percent of the children in the study had a mental illness such as schizophrenia or anxiety disorder and 5.2 percent were taking medication for mental disorders. These pieces of data were used to explore the link between infections and mental illness. These are some of the results the researchers found:
However, these high percentages did fall once other factors were taken into account. To eliminate the influence of genetics and environment on the data, the researchers compared outcomes for siblings of the study participants. They compared the same information for siblings who had infections with those who did not.
Using this data, the increased risk of a mental illness following hospitalization fell to 21 percent from 84 percent. And the risk of being prescribed a medication for a mental illness after hospitalization fell from 42 percent to 17 percent. This might sound like a significant drop and it is. But even more important is the fact that the risk didn’t drop to zero. This indicates that there is still an important link between infections and mental illness.
 Researchers have suggested that the effects of infection on the immune system may be responsible for the link between infections and the mental illness. This may be due to the body’s inflammatory response. Mental illnesses of all kinds naturally cause high pro-inflammatory protein levels and low anti-inflammatory protein levels in the body. So people with a mental illness have higher levels of inflammation. However, what isn’t known is whether the inflammation causes the mental illness or is a consequence of it.
Researchers have suggested that the effects of infection on the immune system may be responsible for the link between infections and the mental illness. This may be due to the body’s inflammatory response. Mental illnesses of all kinds naturally cause high pro-inflammatory protein levels and low anti-inflammatory protein levels in the body. So people with a mental illness have higher levels of inflammation. However, what isn’t known is whether the inflammation causes the mental illness or is a consequence of it.
When you have an infection, your body naturally causes inflammation. This is part of your body’s defense system and it helps to remove the foreign substance and keep the body healthy. The fact that this process occurs first, before the mental illness, indicates that the activation of the immune system in this way might have caused the mental illness.
However, this connection isn’t solid proof of the nature of the link between infections and mental illness. There have also been some suggestions that the pathogens that cause the infections may be to blame. Some pathogens can start in one part of the body and then cross the blood-brain barrier and cause damage to the brain, increasing the risk of mental illness. Some examples of pathogens that can do this are herpes and Toxoplasma Gondii, which is spread through contact with cat feces.
Another reason for the link between infections and mental illness could have to do with how the infection or its treatment affects the gut microbiome. This is the balance of bacteria in your gut, and it’s pivotal to the health of your body and of your brain. However, there’s just not enough information on the gut microbiome and how it affects the brain to support or dismiss this idea.
Despite the confusion about this link, the findings of the study have important implications for your general health. And it’s even more important when you have disorders such as Adrenal Fatigue Syndrome (AFS) which can have an impact on your immune system and on your mental health.
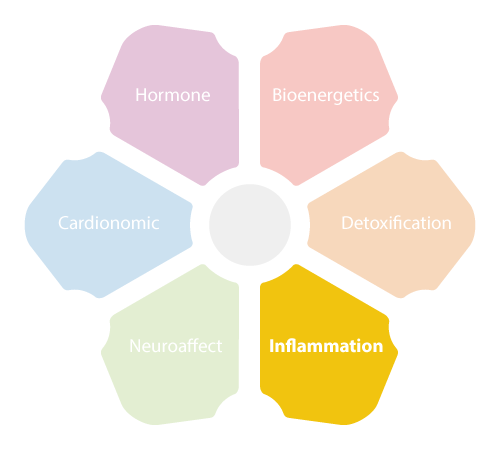 People who have adrenal fatigue often experience a build-up of inflammation in their body because of stress. Chronic stress is very common today, as the modern world seems to be designed to cause stress in every way possible. As a result, many people live in a constant state of stress, and this can tax the NeuroEndoMetabolic (NEM) Stress Response, the system that helps your body cope with stress. The NEM stress response activates the adrenal glands, which are the first organs to become overworked with this stress response is overused. And when the adrenal glands become fatigued, it affects their ability to excrete cortisol, which will affect every system and organ in your body and cause widespread malfunctions.
People who have adrenal fatigue often experience a build-up of inflammation in their body because of stress. Chronic stress is very common today, as the modern world seems to be designed to cause stress in every way possible. As a result, many people live in a constant state of stress, and this can tax the NeuroEndoMetabolic (NEM) Stress Response, the system that helps your body cope with stress. The NEM stress response activates the adrenal glands, which are the first organs to become overworked with this stress response is overused. And when the adrenal glands become fatigued, it affects their ability to excrete cortisol, which will affect every system and organ in your body and cause widespread malfunctions.
Stress can cause a build-up of inflammation in the body. This inflammation is meant to protect and help the body cope with stress, but when the stress is ongoing, the inflammation will start to cause damage. This is a major problem because inflammation is a known cause of heart disease, certain types of cancer, and multiple diseases. And now it seems that inflammation may be the most likely reason for the link between infections and mental illness.
The build-up of inflammation that occurs when you have AFS is due to imbalances with the inflammation circuit. This circuit consists of the immune system, the gut, and the microbiome, and one of its primary duties is to protect the body from invaders like viruses and parasites. However, when you have AFS, the balance between the three systems in this circuit is disrupted.
Stress causes the ongoing activation of the immune system, which caused a buildup of inflammation throughout the body. This upsets the delicate balance of the gut and the microbiome, causing an increase of bad bacteria and overloading the body with toxic metabolites, which are put out by every cell as a result of metabolic activity.
This combination of consequences weakens the body’s protective systems and creates conditions that encourage infections to flourish in the gut and throughout the body. And this will cause even more inflammation, which will make an already bad situation even worse. And the evidence for the link between infections and mental illness suggests the situation is even more serious.
Many people who have AFS also experience mental illnesses. Depression and anxiety symptoms are fairly common as this disorder progresses, and the new information linking infections and mental illness may explain why.
AFS causes chronic inflammation throughout the body. And according to the new evidence, this inflammatory response may markedly increase the chances of experiencing a mental illness. But it gets worse. Infections are common with AFS due to the malfunctioning immune system and the dysregulation of the inflammation circuit. People who have AFS often experience low-grade infections that take longer than usual to heal. So, if you experience infections because of AFS, you may be even more likely to experience mental illness as inflammation increases because of the combination of causes.
And the situation can go the other way as well. If you experience a bad infection and then a mental illness because of the infection, it could overload your body and the NEM stress response. It could be the last straw for your overtaxed body and bring on AFS, which will make the whole situation even worse.
This doesn’t mean that you will definitely develop a mental illness if you have an infection or AFS. Instead, it means that you need to be aware of the risks and take steps to keep your body and your mind as healthy as possible. If you have AFS, this means working towards recovery and lowering your stress levels, along with addressing any infections and other issues that could be complicating your condition as soon as possible.
 Unfortunately, nothing in the body is an isolated system. So, when something goes wrong in one part of your body, it often affects other systems and organs. Researchers are only just starting to understand the depth of these connections and how this could affect your health. The connection between infections and mental health isn’t completely understood, but it obviously has implications for your physical health and your quality of life. So, if you’re suffering from these problems, it’s essential to take a multifaceted approach to your recovery that addresses all of the issues that could be contributing to your health issues.
Unfortunately, nothing in the body is an isolated system. So, when something goes wrong in one part of your body, it often affects other systems and organs. Researchers are only just starting to understand the depth of these connections and how this could affect your health. The connection between infections and mental health isn’t completely understood, but it obviously has implications for your physical health and your quality of life. So, if you’re suffering from these problems, it’s essential to take a multifaceted approach to your recovery that addresses all of the issues that could be contributing to your health issues.
© Copyright 2020 Michael Lam, M.D. All Rights Reserved.
It turns out that there is evidence of a link between infections and mental illness, particularly in children and adolescents. So if you’re struggling to manage your emotions or your mental state, it’s worth investigating the possibility of a physical cause.
