
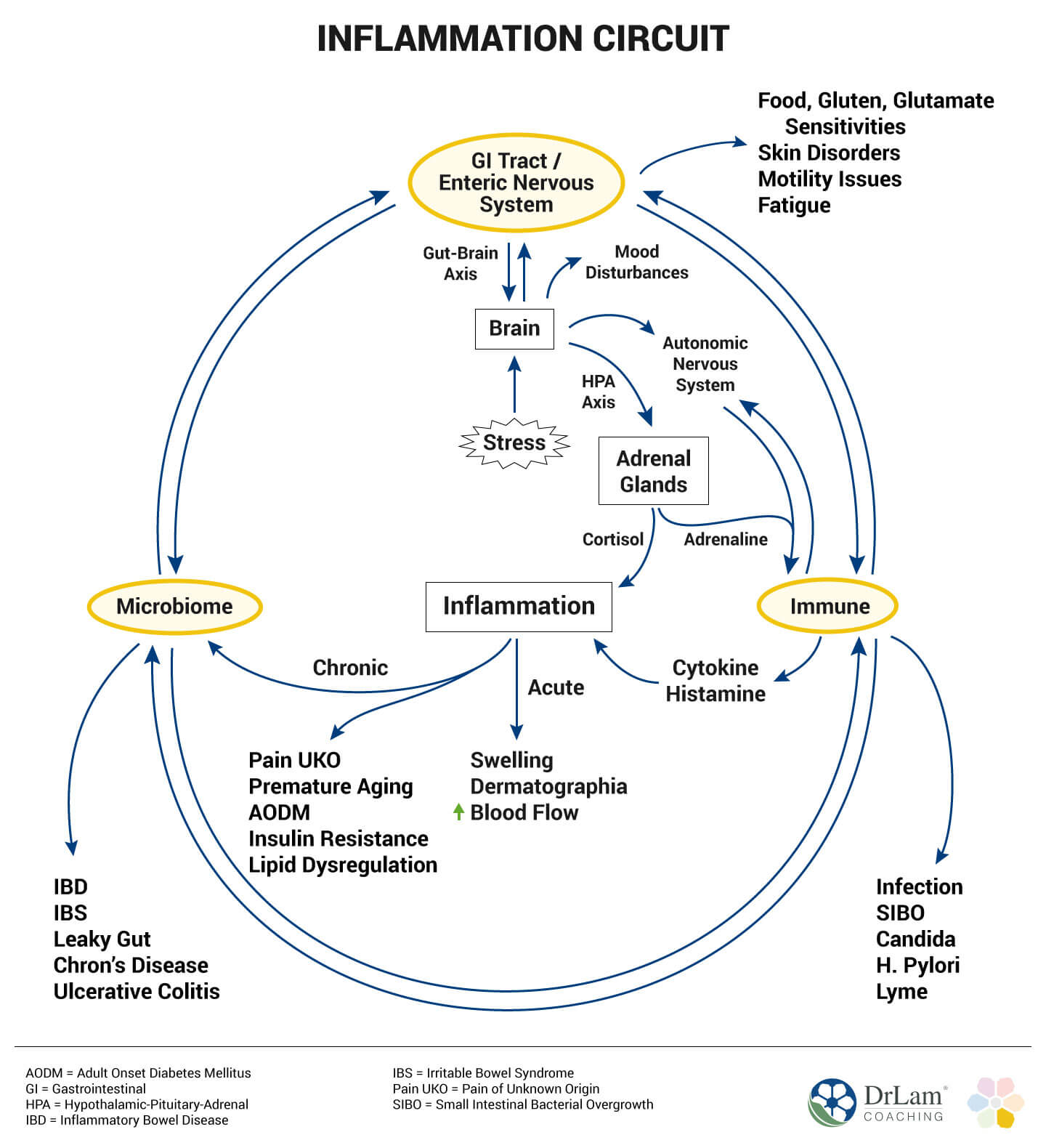
There is a close correlation between adrenal fatigue and chronic inflammation. Inflammation plays a role in the symptoms associated with Adrenal Fatigue Syndrome (AFS) such as brain fog, anxiety and depression, bloating, various bodily aches/pains, and low blood sugar levels. To best understand how this works, you need to take a look at your body’s inflammation circuit.
 Inflammation, essentially, is the result of the body’s response to stress of any kind. This implies it could be due to stress of a physical or a psychological nature. To illustrate, an example of physical stress may be where you fall and break your leg or you become ill with influenza. Psychological stress, on the other hand, is a result of your emotions, e.g. you get into a heated argument with a colleague at work.
Inflammation, essentially, is the result of the body’s response to stress of any kind. This implies it could be due to stress of a physical or a psychological nature. To illustrate, an example of physical stress may be where you fall and break your leg or you become ill with influenza. Psychological stress, on the other hand, is a result of your emotions, e.g. you get into a heated argument with a colleague at work.
Inflammation is the result of a series of changes in your body. These are signals arising at a molecular and cellular level that change your normal physiological responses. The results are the four cardinal signs of inflammation. It was Celsus, a Roman, who in the first century AD, first described and named these four symptoms of inflammation. He termed them:
Inflammation is extremely important when it comes to the body’s ability to repair itself, as the inflammation process allows the body to both fight against and get rid of whatever is causing it harm. The symptoms we feel – redness, swelling, pain, and heat – are the side effects of this process.
Inflammation starts the moment our body begins defending itself against the toxins and pathogens that invade our body or when the body starts healing. During this process, the blood capillaries dilate while the walls become more porous. This allows white blood cells to move through the walls of the blood vessels and thus reach the area where the damage due to the infection has manifest.
The swelling and associated pain in these areas are due to the buildup of fluid that in turn puts pressure on the nerves in these areas, thereby causing the pain and discomfort we feel. The molecular mediators (i.e. molecules fighting inflammation) also trigger pain, increasing your discomfort. The heat felt during the inflammation process is due to an increase in blood flow to that particular area of the body.
Generally speaking, the inflammation circuit responds to any situation in your body to keep itself healthy and working optimally. It is a natural, biological response. Problems arise, however, when inflammation is unchecked. Where your body’s natural inflammatory response is not curbed and controlled, the result may be chronic inflammation.
As mentioned, inflammation is the result of either physical or psychological stress. However, inflammation due to psychological stress usually has a lesser impact than that triggered due to physical (physiological) stress. Inflammation is an automatic response to any threat experienced by the body, no matter whether it is real or not.
 Short term pain usually associated with your body’s response to acute inflammation is of long-term benefit. The same, however, is not the case when it comes to low-grade, continuous inflammation that is so often the response to psychological stress and chronic infection, as is the case with Lyme Disease or the Epstein-Barr (EB) virus. Here, your body experiences a constant state of stress that results in the inflammation circuit working overtime. The result is a state of imbalance that makes you more susceptible to contracting different diseases and negatively impacts the effects associated with the aging process.
Short term pain usually associated with your body’s response to acute inflammation is of long-term benefit. The same, however, is not the case when it comes to low-grade, continuous inflammation that is so often the response to psychological stress and chronic infection, as is the case with Lyme Disease or the Epstein-Barr (EB) virus. Here, your body experiences a constant state of stress that results in the inflammation circuit working overtime. The result is a state of imbalance that makes you more susceptible to contracting different diseases and negatively impacts the effects associated with the aging process.
This kind of inflammation, although not noticeably perceivable, is present for years before actually manifesting itself. Interestingly, the length of time this inflammatory state is present not only directly impacts the severity of your diagnosed condition, but the prognosis as well. Your body’s inflammatory circuit’s response to certain conditions is, in many instances, the reason for certain chronic conditions.
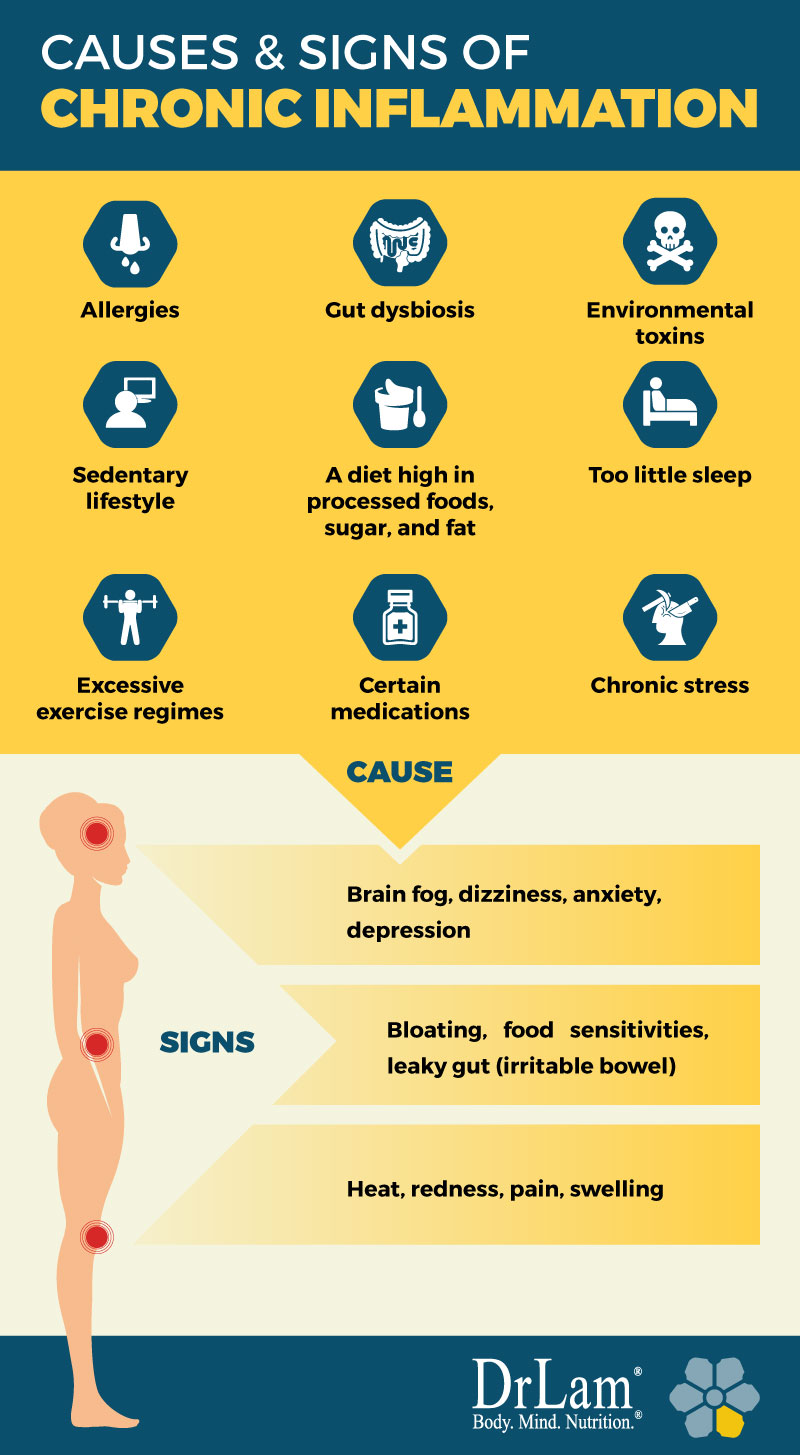
Although the typical signs of inflammation are easy to identify (heat, redness, pain, and swelling), signs pointing to chronic inflammation are not as easy to see. Among these are signs including: bloating, brain fog, food sensitivities, anxiety, depression, leaky gut (irritable bowel), dizziness, and many others.
Acute inflammation, in someone who is healthy, is easily controlled. It is activated when a threat is perceived. It then fights the infection and starts to repair any damage. It also, however, returns to normal once the threat has passed, allowing the body to function normally once more. The cortisol hormone secreted by the adrenal glands controls the inflammation ‘turn-off’ process. Cortisol is also your body’s stress reduction hormone.
Although inflammation is uncomfortable, it is necessary and the body is designed in such a way that it can both tolerate and control it. Research indicates that chronic low-level stress stays in the body for a period even when there is no physical sign of it and has a negative effect on both physiological and psychological health.
Inflammation pertaining to a specific chronic condition is local. This indicates that those with heart disease have localized inflammation in their arteries, those with diabetes have it in their pancreas, and those with Alzheimer’s have it in their brain. Inflammation is also, however, the result of certain toxins present in the environment or in the food we eat; in this case, they can affect different areas of the body, thereby affecting not only your health and mental acumen but even your length of life.
There are many diseases and health issues that include an aspect of inflammation. These include, among others:

There are many causes of chronic inflammation that result in the inflammation circuit becoming unbalanced. These include, among others:
Adrenal fatigue is commonly overlooked as the cause of an unbalanced inflammation circuit.
The inflammation circuit is one of the key responders when the body is subjected to any type of stress. The inflammatory response works in conjunction with other body systems and organs when reacting to stress, while still trying to keep up with their ‘normal’ bodily functions. The body systems that most directly affect the inflammation circuit include:
What are the individual functions of these different components and how do they affect inflammation?
Most of the different inflammatory diseases start in your body’s gut (gastrointestinal or GI tract). From there, they spread to different parts of your body. The gut’s lining is permeable, meaning it allows certain substances to pass through and enter the bloodstream.
When this permeability increases, however, unwanted substances also pass through, thereby triggering the body’s immune system in order to fight it. This may result in not only inflammation but also allergies and diseases consequently. In certain instances these toxins make their way to your brain, resulting in not only depression but certain neurological problems as well.
Once the problem becomes systemic in nature, in other words, it affects your entire system, your body is no longer able to digest properly. This makes it extremely difficult for you to get the different nutrients, vitamins, and minerals your body needs in order to work effectively, no matter how healthy your diet may be.
Let’s look at some symptoms that can arise from an inflamed gastrointestinal system.
Another issue that is on the increase is an increasing sensitivity to certain foods, especially gluten. The reason why food sensitivities often go undiagnosed for so long is because the symptoms are so similar to that of other gut disorders and conditions. They are usually mistaken for another ailment.
 Gluten, the protein responsible for making dough sticky, is made of glutenin and gliadin. This protein is found in most grains, e.g. wheat, barley, rye, semolina, Kamut (Khorasan wheat or Pharaoh grain), and barley. It is not, however, only limited to certain types of grain, but is usually found in many types of processed foods, medications, supplements, and health and beauty products.
Gluten, the protein responsible for making dough sticky, is made of glutenin and gliadin. This protein is found in most grains, e.g. wheat, barley, rye, semolina, Kamut (Khorasan wheat or Pharaoh grain), and barley. It is not, however, only limited to certain types of grain, but is usually found in many types of processed foods, medications, supplements, and health and beauty products.
The question, however, is why has the number of people with a gluten sensitivity increased by so much?
The reason is simple. Wheat has been cross-bred with other proteins to get a product that not only grows much faster, but that is able to survive in more difficult environmental conditions. Add to this the fact that it has been processed in such a way as to become even more water-soluble in order to mix with other ingredients. This means that we are actually consuming wheat in much larger quantities than our forefathers ever did. The result is an ever-increasing percentage of the population developing a sensitivity or intolerance to gluten.
Once eaten, gluten is broken down into gliadin and glutenin due to enzyme action. Once they reach your gut-associated lymphoid tissue (GALT), they are assessed to see whether they are harmful to your body. If you happen to be sensitive to gluten, the GALT attacks the proteins by means of antibodies. In those with Celiac disease, both the proteins and enzymes breaking down the gluten are attacked by the antibodies produced by the GALT.
Another function of this enzyme is to help with the absorption of nutrients. This it does by holding the gut’s microvilli together. Microvilli are hair-like structures that are found in the intestinal wall. Any attack on this enzyme results in the microvilli becoming damaged – which in turn has a negative impact on the gut wall, making it more permeable to toxins and resulting in a condition known as leaky gut. The antibodies could also attack your organs and other tissue, e.g. your skin and brain. The result is an autoimmune disorder.
However, it is not only gluten that causes inflammation. Other sources are dairy products, oils containing linoleic acid, e.g. peanut, sunflower, safflower, and corn oil, and refined and simple carbohydrates.
You can both heal your gut and calm down your inflammation circuit by identifying and eliminating foods to which you are sensitive. Chronic inflammation is closely linked to Adrenal Fatigue Syndrome (AFS) and the NeuroEndoMetabolic (NEM) stress response. By making dietary adjustments, you help yourself heal from adrenal fatigue while at the same time reducing the risk of contracting a GI disorder.
 Constipation is a condition where the bowels do not move regularly, resulting in difficult, and perhaps painful, defecation. Considered normal to be constipated now and then, regular constipation may result in a gut disorder that can affect the inflammation circuit.
Constipation is a condition where the bowels do not move regularly, resulting in difficult, and perhaps painful, defecation. Considered normal to be constipated now and then, regular constipation may result in a gut disorder that can affect the inflammation circuit.
You may ask ‘how normal is normal?’ It varies from person to person, but defecating once or twice a day is within the bounds of what is considered as normal in most instances. Going without a bowel movement for more than three days leads to constipation, as the stool dries out over time, making it more difficult and painful to defecate.
Using the bathroom while constipated is not only uncomfortable, but the straining causes a set of problems of its own, such as hemorrhoids or diverticular disease.
There are a number of reasons for constipation. Among these are included: a diet poor in fiber, drinking too little water, a diet high in dairy products, colon cancer, irritable bowel syndrome, long periods of inactivity, problems arising due to issues with the muscles or nerves of your colon, stress, certain types of medications, hypothyroidism, and pregnancy.
Constipation is often a complication that manifests during the latter stages of adrenal fatigue, as your body’s lowered energy levels make it difficult to defecate in a bid to conserve its energy. Your digestion slows down, causing waste materials to stay in the colon. This increases toxicity and results in inflammation. Symptoms usually associated with this state of affairs include: food allergies, brain fog, pain, irritability, yeast infections, anxiety, and a host of others.
If left alone, and as your adrenal fatigue progresses, things, over time, get worse. Toxins build up in the body overwhelming the inflammation circuit, possibly resulting in inflammation that in turn could lead to the breakdown of the musculoskeletal system. This would include the internal organs’ collagen structures. Your GI tract, over time, becomes compromised, causing a circular effect whereby your constipation and digestive issues worsen. Your stomach does not produce enough acid in order to break food down so that nutrients are assimilated. This depletes the cells. The result is a cycle causing the entire system to slow down in order to conserve energy. It can, however, result in a catabolic state characterized by a huge weight loss.
In most such instances, the thyroid gland is also compromised, slowing down in order to reduce your metabolic rate in an effort to conserve energy. This further compounds your fatigue and adds to the constipation problem. Because waste products build up, the toxins start affecting your liver and kidney function. Where the constipation is severe or persists, an enema may be necessary. Gut flora can be improved by means of probiotics. They help to improve the gut flora composition, help with bowel movement regulation, and help to prevent GI disorders.
Diarrhea is only a problem when it is persistent as it could cause you to become dehydrated and lose electrolytes. If persistent, however, it is also indicative of a more serious problem. If you notice blood and/or mucus in your stools, and have fever, pain, or suffer from weight loss, you need to consult with a healthcare practitioner as soon as possible as these are signs of an underlying, deeper problem.
 There are a number of common causes when it comes to diarrhea. These include bacteria, eating foods to which you are allergic or to which you are sensitive, or viruses. Other causes may include Crohn’s disease, Irritable Bowel Syndrome (IBS), diabetes, certain cancers, hyperthyroidism, and malabsorption, among others.
There are a number of common causes when it comes to diarrhea. These include bacteria, eating foods to which you are allergic or to which you are sensitive, or viruses. Other causes may include Crohn’s disease, Irritable Bowel Syndrome (IBS), diabetes, certain cancers, hyperthyroidism, and malabsorption, among others.
In most cases, however, diarrhea is not related to any of these conditions and the problem is usually alleviated by means of medications that can be purchased over the counter. In the majority of cases, light meals, enough rest, and staying hydrated help immensely.
People who have Adrenal Fatigue Syndrome (AFS) usually suffer more from constipation than diarrhea. On the other hand, very severe diarrhea is often to be found in those who have advanced adrenal exhaustion.
One of the gut’s most important purposes is to prevent toxins, microbes, undigested food, and foreign substances from gaining entrance to the bloodstream. When healthy, the mucosal cells’ junctions in the gut are tight, allowing only the nutrients needed by the body to pass. When you have leaky gut, these junctions are not as tight, and toxins and other particles are allowed through. These are seen, by the immune system, as foreign invaders. Your inflammation circuit then attacks them, resulting in inflammation.
Symptoms of Irritable Bowel Syndrome (IBS) include:
IBS is usually diagnosed by a process of elimination when lab tests rule out other conditions with similar symptoms. It is, in essence, an irritation of the GI tract.
Although many factors contribute to IBS, e.g. the use of certain medications such as antibiotics, anxiety, depression, a hormonal imbalance, and various other factors. Stress plays a major role.
The latter stages of AFS see the metabolism slow down to conserve energy. During this process, gut movement slows down as well. Food thus moves through the body at a much slower pace. The result is, more often than not, constipation, although diarrhea also manifests on occasion. This, of course, adds to your gut irritation and worsens the symptoms associated with IBS.
Certain supplements, like omega 3 fatty acids, Dehydroepiandrosterone (DHEA) hormone, activated charcoal, glutamine, pantothenic acid, plant sterol, quercetin, and pantethine all can potentially help with the occurrence of leaky gut. Adding fiber to your diet, as well as using peppermint oil, are great aids when it comes to combating diarrhea while helping in the prevention of GI disorders. Some types of fiber are even useful for helping your microbiome and strengthening your inflammation circuit.
 Your microbiome can be described as all the genetic material of all your different microorganisms within a certain environment in your body. It is the second part of the inflammation circuit. The word ‘microbiome’ is actually broken up into two parts: micro (meaning small), and biome, which includes all the characteristics found in an environment, including the biotic (living) and abiotic (non-living) components.
Your microbiome can be described as all the genetic material of all your different microorganisms within a certain environment in your body. It is the second part of the inflammation circuit. The word ‘microbiome’ is actually broken up into two parts: micro (meaning small), and biome, which includes all the characteristics found in an environment, including the biotic (living) and abiotic (non-living) components.
The term biome is not to be mistaken with the term microbiota which refers only to the microorganism within a certain environment, i.e. only the GI tract, as an example.
It has been estimated that approximately ninety percent of all cells in the body are not human. They are, for the most part, prokaryotic in nature. A prokaryote is unicellular, has no mitochondria, and the nucleus is without a membrane. These prokaryotic cells are the result of over forty thousand different strains of bacteria coming from over 1,800 different genera. In total, these smaller cells, of which our bodies have about 100 trillion, make up about five pounds of an adult’s weight. This means that taken as a mass, they are roughly the size of an adult human brain.
Prokaryotic cells are found everywhere in the human body where it is exposed to the environment. This includes the skin, vagina, and mouth, although the largest population is to be found in the gut. This is because this area has a constant supply of the nutrients it needs for survival. Taken collectively, they outnumber our other cells in a ratio of ten to one.

While you are a fetus, the gut is sterile. It only becomes populated with microbes from the mother’s vaginal and fecal microbiome during birth. Other (environmental) microbes are received during the first few days after birth. There are different factors influencing colonization at this time, including diet (breastfeeding or formula milk), possible antibiotic treatments, and hygiene. Interestingly, children born by C-section are often not as healthy as those born naturally and are often obese in later life.
The first microbes to colonize are known as facultative anaerobes, i.e Escherichia coli, and Streptococcus spp. and Escherichia coli, and obligate anaerobic species that present themselves as your gut’s oxygen levels decrease. Once a child is three years old, his microbiome has stabilized, although it continues balancing itself throughout our lives as the body strives to maintain homeostasis.
As we age, however, the microbiome changes as well. The result is an increase in inflammation due to a decrease in the body’s microbial diversity.
 The majority of microbes found in the body do no harm. Instead, they help in maintaining certain processes that ensure continued health. These microbes, although harmless under normal conditions, are considered part of the natural flora in a normal microbiome. Healthy gut bacteria is needed for the many functions carried out in our body. Among these are included the reactions associated with various enzymes. Our body cannot carry out these functions on their own, e.g. synthesizing certain vitamins in order to stay healthy.
The majority of microbes found in the body do no harm. Instead, they help in maintaining certain processes that ensure continued health. These microbes, although harmless under normal conditions, are considered part of the natural flora in a normal microbiome. Healthy gut bacteria is needed for the many functions carried out in our body. Among these are included the reactions associated with various enzymes. Our body cannot carry out these functions on their own, e.g. synthesizing certain vitamins in order to stay healthy.
The gut’s microbiome, when we are young, plays an extremely important role when it comes to the formation of our immune system. This is especially the case in early childhood when the immune system is still developing. It is as children that our body’s immune system is exposed to and becomes used to antigens and develops a tolerance towards them. Once the state of homeostasis (balance) is reached, foreign microbes and antigens will not be able to cause an inflammatory response in the body. It is only when our immune system is weak or underdeveloped that exposure to foreign allergens will trigger a response in the inflammation circuit resulting in autoimmune diseases, allergies, and a sensitivity issue when it comes to chemicals and certain foods.
A good example is that of mice kept in a sterile environment their whole life. Although they are healthy, their immune system is not fully developed. Once exposed to foreign microbes, they tend to develop autoimmune diseases and other health issues.
Research indicates an infant’s first gut microbiome has a profound effect on their health. Babies that were delivered via a C-section were compared with those born naturally. They found that the latter colonized their mother’s gut and vaginal biomes and the former, who were not exposed during birth, tended towards allergies and obesity.
Different microbes, seemingly, on certain parts of your body have a different functionality on different people. An example is where two people have a different microorganism on their tongues, yet they do exactly the same job when it comes to breaking down sugars. Microbes need a stable habitat that is rich in terms of the food we eat. In turn, we benefit from the heat energy released when they break down certain components that are digested by the gut.
This means there is a definite, beneficial interaction between our bodies and our microbe hosts, and that certain functions in the body are dependent on these microbes in order to stay healthy. When, for some reason, there is an imbalance in our microbiomes, we are in a state of dysbiosis.
 Inflammation is often the result of dysbiosis. It plays a role in a number of health issues, including diabetes, obesity, asthma, autism, and heart problems, among others. It is also associated with certain problems relating to the bowels, such as Crohn’s disease. It may also play a role in the brain and is thought to be one of the triggers of leaky gut syndrome (IBS). These conditions are all linked to dysbiosis in the gut.
Inflammation is often the result of dysbiosis. It plays a role in a number of health issues, including diabetes, obesity, asthma, autism, and heart problems, among others. It is also associated with certain problems relating to the bowels, such as Crohn’s disease. It may also play a role in the brain and is thought to be one of the triggers of leaky gut syndrome (IBS). These conditions are all linked to dysbiosis in the gut.
A common cause of dysbiosis is antibiotics. They destroy ‘good’ bacteria needed to keep your system in balance. When the ‘good’ microbiome is negatively impacted, so too is your immune system.
Dysbiosis in the gut may cause inflammation which in turn leads to damage of the mucosa. When the junction between different mucosal cells is compromised, your immune system responds accordingly. Proteins, bacteria, and toxins can easily move into the bloodstream through the damaged gut lining, causing what is known as leaky gut (IBS). The symptoms associated with this condition include: brain fog, depression, insomnia, and fatigue, along with a host of others.
Healthy gut bacteria, in conjunction with a diverse microbiome, results in a healthy gut supporting your inflammation circuit. People with a healthy gut are often healthier and less likely to get infections or recurrent illnesses as their body’s defense system is stronger.
Dysbiosis in the gut has been linked to a number of neurological disorders. Among these are the autism spectrum, multiple sclerosis (MS), and Parkinson’s. An initial symptom for a Parkinson’s sufferer is usually constipation, to be followed by a loss of smell and taste. The other symptoms, such as tremors and shuffling only appear long after the GI disturbance appears.
There are many environmental factors that influence neurological conditions and the inflammation circuit. One of these is where proteins are not correctly used in the brain, resulting in a number of neurodegenerative disorders. It may be the result of gut inflammation triggering certain inflammatory responses in the brain causing the inadequate use of proteins and the degeneration of the neural cells in the brain.
Inflammation and a gut imbalance may also be linked to certain autoimmune disorders. The populations of Western countries have a similar diet and a corresponding higher rate of MS. The diet followed may result in inflammation and thus a disruption in the proper functionality of the microbes present in the intestinal tract.
People suffering from Parkinson’s and MS show an increase in antibodies against a number of antigens due to the increased permeability of their intestinal lining. Evidence would suggest that constant stress, among various other reasons, is responsible for the dysregulation of the inflammation circuit.
Alzheimer’s and a decrease in cognitive functions are earmarked by oxidative stress, immune problems, and changes in the brain itself. Experiments show that these are all due to diet and the effect it has on the gut biome. Neurotrophin, a protein that both protects and encourages healthy neurons, is dependent on a healthy gut biome. Those with Alzheimer’s show a marked decline in this regard.
 Evidence shows a strong correlation between gut and brain health. This implies that certain psychological problems, such as depression, may be the result of inflammation, with the gut as the initial instigator. Research on animals shows a marked psychological decline in healthy mice when certain microbes are transplanted from those that are depressed.
Evidence shows a strong correlation between gut and brain health. This implies that certain psychological problems, such as depression, may be the result of inflammation, with the gut as the initial instigator. Research on animals shows a marked psychological decline in healthy mice when certain microbes are transplanted from those that are depressed.
Two of the most common symptoms associated with AFS are anxiety and depression. The evidence thus suggests it is imperative that those with the problem need to ensure a healthy gut microbiome. Not only will it help restore their neurological processing, but help the body in its recovery.
When the growth of bacteria in your small intestine grows beyond what is considered a healthy limit, the condition is known as Small Intestinal Bacterial Overgrowth (SIBO). These bacteria are usually to be found in the colon. Those with SIBO have very similar symptoms as those who have IBS, and many people suffer from both these conditions. Symptoms associated with the condition include abdominal pain, constipation, bloating, gas, and diarrhea.
There are a myriad of reasons why this condition develops. The most common causes include:
If SIBO is not treated, it has a debilitating effect on your health, resulting in chronic diarrhea, leading to malabsorption of the necessary nutrients your body needs, and ultimately, weight loss.
 Inflammation is an important component of your immune system. Chronic inflammation is usually the result of infections, an autoimmune reaction to your own bodily materials, or the result of an antigen from the environment, etc. In instances of chronic inflammation, the mediators are monocytes and macrophages, which are components of the immune system. They are leukocytes, otherwise known as white blood cells. Leukocytes, when confronted with a problem, release chemical agents that target that which has caused the inflammation circuit to response.
Inflammation is an important component of your immune system. Chronic inflammation is usually the result of infections, an autoimmune reaction to your own bodily materials, or the result of an antigen from the environment, etc. In instances of chronic inflammation, the mediators are monocytes and macrophages, which are components of the immune system. They are leukocytes, otherwise known as white blood cells. Leukocytes, when confronted with a problem, release chemical agents that target that which has caused the inflammation circuit to response.
The problem, however, is that these cells not only target the invaders but your own tissue as well, causing damage. These damaged tissues need constant repair. Chronic infection is also responsible for your body continuously developing new blood vessels.
The repair work completed often causes irritations, and by so doing, results in the inflammatory process being retriggered. If for whatever reasons, this becomes a cycle, your body stays in a constant state of inflammation that, in the long-term, has a debilitating effect.
Modern medicine does not provide a long-term solution to the problem in such cases. At times, certain steroids that suppress your immunity are prescribed. These medications, however, often only provide short-term, symptomatic relief, and do not address the underlying root cause of the problem.
The inflammation circuit does not necessarily function correctly due to a strong immune system, as the immune system could, on occasion, when overactive, cause autoimmune issues.
When under stress, the immune system finds and protects us against pathogens, triggering an inflammatory response to deal with the problem. The immune system thus attacks and gets rid of any potential dangerous pathogens. An immune system that functions as it is intended quickly gets rid of the danger posed by certain chronic pathogens and infections.
Although a weakened immune system is often responsible for recurring infections, or even those that are difficult to get rid of, it is not necessarily the cause of illness – an overactive immune system may also be responsible.
Under ‘normal’ conditions, your immune system identifies and targets enemy pathogens, while leaving those considered as beneficial alone. At times, however, this is not the case, and the inflammation circuit becomes overzealous, creating an immune response to even normal cells and conditions.
When this occurs, certain antibodies become confused between what they see as a normal cell and what is perceived as a pathogen. It then attacks indiscriminately. The result, when this happens, is that the inflammation circuit is then presented with flare-ups that happen to be consistent with certain autoimmune conditions.
Consider the following where the body can potentially recognize its own cell as foreign and mount an autoimmune type response:
Eating a food we are sensitive to can cause inflammation and leads our immune cells to see our tissue as foreign. The immune response is activated to rid itself of such unwanted guests.
Our gut is a complete ecosystem on its own, perfectly maintained by beneficial bacteria. When this system is off balance, as in someone who suffers from SIBO (Small Intestinal Bacterial Overgrowth), gastric reflux, H. pylori, irritable bowel, inflammatory bowel disease, catabolic state, or the gastric slowdown in advanced stages of adrenal fatigue, which can mean good beneficial bacteria are replaced by foreign non-beneficial bacteria. Gastric assimilation becomes suboptimal. Foreign opportunistic bacteria and stealth viruses transition from a dormant to active state. This causes the immune system to go into overdrive leading to chronic inflammation.
In this process, the immune system, especially if in a hyperactive state, can become easily confused about who the real enemy is. Attacks are made on the foreign opportunistic bacteria and itself concurrently, leading to various autoimmune diseases.
The HPA axis is the primary stress regulatory hormonal axis of the body. Cortisol is the main anti-stress hormone. In advanced stages of adrenal fatigue, insufficient cortisol produced leads to rampant systemic inflammation which in turn can contribute or trigger autoimmune symptoms.
 When food particles cross the gastrointestinal mucosa, inflammation is triggered. Undigested foods are supposed to be inside the GI tract. When it enters the hepatic circulation and the rest of the body, the immune system recognizes this as foreign and every attempt is made to try to attack and neutralize such foreign compounds. The persistent activation of the immune system can lead to immune cells cross-reacting with normal cells to trigger autoimmune diseases.
When food particles cross the gastrointestinal mucosa, inflammation is triggered. Undigested foods are supposed to be inside the GI tract. When it enters the hepatic circulation and the rest of the body, the immune system recognizes this as foreign and every attempt is made to try to attack and neutralize such foreign compounds. The persistent activation of the immune system can lead to immune cells cross-reacting with normal cells to trigger autoimmune diseases.
Environmental toxins are everywhere. It is impossible to escapes if one lives in the urban world. Excessive toxins accumulating in our body are triggers of our immune system to work in a hyperactive state to rid our body of such unwanted material. Those who are unable to carry this function naturally and properly can develop symptoms of autoimmune disease.
Living in the modern world exposes us to a constant barrage of viruses, fungi, bacteria, and protozoa, etc. Some pathogens tend to stay with us for a long time, in a dormant state. They become activated and flare up when our immune system is weak. These organisms include Borrelia burgdorferi, Babesia microti, Candida albicans, EBV, CMV and many others. The diseases created by these pathogens can lead to hyperactivity of the immune system.
Cross-reactions with normal tissues in the body are not uncommon. Many of these infectious diseases present with symptoms of an autoimmune disorder, such as swelling, joint pain, psoriasis, fatigue, and food sensitivities. Autoimmune laboratory markers may be elevated in blood tests.
This also lowers the barrier to invasion by a pathogen, triggering our immune system to go into overdrive. It can, therefore, be a conduit that initiates the autoimmune response. In other words, stress worsens any pre-existing clinical or sub-clinical autoimmune disorders.
 It is important to remember that such events are uncommon. However, when the body’s immune system is overly active, or in a hyperactive state, the collateral damage can be significant. Sufferers can begin to experience symptoms typical of autoimmune diseases, such as joint pain and fatigue.
It is important to remember that such events are uncommon. However, when the body’s immune system is overly active, or in a hyperactive state, the collateral damage can be significant. Sufferers can begin to experience symptoms typical of autoimmune diseases, such as joint pain and fatigue.
With a body inflamed from existing microbiome imbalance, GI tract irritation, or reactive metabolite overload, it is hard to fully decipher for sure if there is a true autoimmune disease (such as primary Hashimoto’s thyroiditis or Lupus), or just symptoms resembling autoimmune disease surfacing when the body’s good cells are attacked in the crossfire.
Laboratory tests such as RA, CRP, ANA titers and anti-TPO antibodies may add to the confusion. They may be normal or borderline high in these situations rather than sky high as with a true primary autoimmune state. Other laboratory studies are generally unremarkable.
Unfortunately, few clinicians are on the alert for this differentiation that depends on a detailed history for proper assessment. When normal or borderline high laboratory tests are accompanied by fatigue, joint pain, psoriasis, gastric discomfort, weight gain, vasculitis and muscle ache, the knee-jerk reaction by physicians is to jump to the clinical diagnosis of autoimmune disease. There is no comprehensive look at the body holistically to look out for a hyperactive immune state as the root cause.
 Remember it takes two hands to clap. A hyperactive state combined with pathogens perceived as foreign is the worst possible state. However, even if there is no significant pathogen, a body in a hyperactive immune state can cause damage simply by its hyperactivity.
Remember it takes two hands to clap. A hyperactive state combined with pathogens perceived as foreign is the worst possible state. However, even if there is no significant pathogen, a body in a hyperactive immune state can cause damage simply by its hyperactivity.
Because clinical presentation is similar, little effort is put to trace the symptoms to the root cause – whether it is primarily pathogen-driven, hyperactive immune state driven, or a combination thereof. Patients are often put on steroids and autoimmune medications. Short-term benefit is common, as the hyperactive immune state calms down from anti-inflammatory properties of corticosteroids.
Long-term use of steroids? can be problematic as it can reduce our overall immune response and mask the underlying problem of excessive metabolites within a setting of hyperactive immune state being the true cause. There is a slow but gradual deterioration of the inflammation circuit over time as it becomes dysfunctional. A typical example of this is Hashimoto’s thyroiditis.

The thyroid system is often one of the organs most vulnerable to dysfunction from a hyperactive immune state as the body’s inflammation circuit is put into overdrive. The thyroid glands control the overall metabolic rate and are responsible for our body temperature regulation. Slight changes in thyroid function can result in fatigue, weight gain and feeling cold on the hypothyroid side and anxiety and heart palpitations? on the other extreme.
One of the most frequent complaints that bring patients to their doctors is fatigue and lack of energy. Standard medical workup usually consists of a complete metabolic panel to evaluate thyroid function. In a hyperactive immune state, anti-thyroid autoantibodies (also called anti-thyroid antibodies) that target one or more components of the thyroid may be activated. The most significant one being anti-TPO antibodies. It is present in roughly 90 percent of Hashimoto’s thyroiditis, 10 to 20 percent of nodular goiter or thyroid carcinoma, and 75 percent of Graves’ disease. Clinicians often make the diagnosis of Hashimoto’s thyroiditis based on laboratory test showing anti-TPO antibodies in a clinical setting of fatigue and low energy.
Also, it should be noted that 10 to 15 percent of normal individuals can have a higher level anti-TPO antibody titer. They do not have primary autoimmune disease like those mentioned above. The high titer can be secondary to a hyperactive immune system when our inflammation circuit is on overdrive. These patients can be mistakenly diagnosed as having clinical or subclinical primary Hashimoto’s thyroiditis. Thyroid replacement is often started. Little consideration is given to alternative causes such as inflammation circuit overload.
When symptoms of fatigue improve with thyroid replacement, physicians are misled into thinking they were on the right track, especially if thyroid laboratory studies start to normalize. More often than not, high anti-TPO antibody count may not normalize totally, but fatigue may improve. Doctors are at a loss, but since the patient is feeling better, no further investigation is needed. In other words, normalizing TSH, free T4, and free T3 gives the physician a false sense of compliance.
A persistent high rT3 or anti-TPO titer is disregarded as important in such circumstances. Little attention is placed on investigating whether or not symptoms are caused by a hyperactive immune state trigger by inflammation circuit dysfunction that is clinically accompanied by fatigue that comes from adrenal burnout. Because thyroid replacement tends to help increase energy and normalize laboratory tests, there is little interest or need to further consider other differentials until this approach stops working. The entire focus of therapy is on primary thyroiditis alone as a presumptive diagnosis.
 Without resolving the underlying root cause of a possibly hyperactive immune state and concurrent adrenal fatigue as a secondary cause of symptoms resembling autoimmune disorders, many sufferers will continue to need an ever larger dose of thyroid replacement to keep laboratory numbers normalized and sustain energy over time. This can play out over decades.
Without resolving the underlying root cause of a possibly hyperactive immune state and concurrent adrenal fatigue as a secondary cause of symptoms resembling autoimmune disorders, many sufferers will continue to need an ever larger dose of thyroid replacement to keep laboratory numbers normalized and sustain energy over time. This can play out over decades.
Many who started on T4 replacement eventually have to advance to combination T4/T3 formulas and ultimately to the most potent T3 replacement to maintain the same energy flow. They feel terrible inside, often wired and tired, only to be told all is well.
In other words, thyroid slowdown symptoms are treated as an autoimmune issue based on lab tests and symptoms when in reality, it represents a body in trouble with the inflammation circuit. Thyroid replacement merely covered up the symptoms in such cases. A holistic approach should be deployed to fully comprehend the root cause and effect a comprehensive long-term recovery plan.
The inflammation circuit is part of the NeuroEndoMetabolic (NEM) stress response deployed by the body to overcome stress. Excessive and dysregulated inflammatory response can wreck your body, leading to a host of conditions and undesirable symptoms. Conventional medicine’s approach to this problem is by way of suppression of symptoms. This can worsen the situation over time. Autoimmune diseases and hyperactive immune state are frequent consequences. Understanding the body from a holistic standpoint is needed to fully comprehend the clinical significance because of the systems-wide reunification when a body is overly inflamed.