 Stress has been shown time and again to be a major influence on mood, physical health, mental health and behavior. Persistent stress can make you generally more susceptible to physical and psychological problems, and it can be a precursor to many illnesses. Stress induced inflammation is something that everyone should be made aware of so that the prevention of many diseases, as well as recovery from them, can happen at the causal level.
Stress has been shown time and again to be a major influence on mood, physical health, mental health and behavior. Persistent stress can make you generally more susceptible to physical and psychological problems, and it can be a precursor to many illnesses. Stress induced inflammation is something that everyone should be made aware of so that the prevention of many diseases, as well as recovery from them, can happen at the causal level.
We are all equipped with the ability to neutralize stress through a series of stress responses that are fast and efficient enough to prevent damage to our physical and psychological health. However, when acute stress turns into chronic stress, it increases our health risks significantly.
There are many physical disorders that have been connected to stress, including:
Psychological problems like depression, anxiety, and panic attacks are also very commonly linked to chronic stress.
The interesting thing that not many people are made aware of by their doctors is that the inflammation that is induced by the chronic stress is actually what creates the environment for these problems to develop, including the psychological issues mentioned above.
But, what exactly is stress?
Stress is a force or state of tension, pressure or strain imposed by a stressor. A stressor is the stimulus that creates stress and it can be psychological or physical. All kinds of stress will have a physiological effect on the body in the form of the body’s stress responses.
Not all stress is bad. In fact, some types of stress are healthy and needed, such as stress caused by moderate exercise. For our purposes, we are going to focus on unhealthy and excessive stress.
Physical stressors include:
Psychological stressors include:
All of these stressors can elicit an acute stress response, but if they are not resolved and the stress response is constantly switched on, the stress becomes chronic and opens the body up to many problems, including stress induced inflammation.
One very important factor in health, and even survival, is the ability of the body to maintain homeostasis – the equilibrium between different organs and systems. Stress is a threat to the maintenance of this homeostasis.
Depending on the stressor, different patterns of stress responses are elicited. Also, different people will have different stress responses to the same situation.
For example, some people will have a more averse reaction to a stressful situation, especially if the situation does not allow for an active response like fight or flight to actually be effective. These aversive reactions will typically involve the sympathetic nervous system, an inhibition of movement and the blood shunting from the periphery of the body. This is also called a vigilance response.
On the other hand, some people will have a more active coping mechanism to stress, such as the fight or flight response, which helps them either defend themselves or run away from a threat by increasing hormonal, metabolic and autonomic functions that enhance their muscular capabilities.
 Most stress responses are integrated, and everyone is capable of both types of response. Although the pattern of the stress response that shows up largely depends on the situation itself, there is a certain personal tendency that is determined by genetic, developmental and environmental factors.
Most stress responses are integrated, and everyone is capable of both types of response. Although the pattern of the stress response that shows up largely depends on the situation itself, there is a certain personal tendency that is determined by genetic, developmental and environmental factors.
Studies in rats and dogs have shown that those that were nurtured consistently by their mothers early on have lowered stress responses and less anxiety than those that were not.
The mechanisms of homeostasis are sophisticated enough to help the body deal with acute stress without much damage to the system, especially for younger, healthier people. Those who suffer from illnesses already, are in weak health or are older tend to have a higher health risk when exposed to stress.
This is especially true if the stress becomes more consistent. Even younger, healthier individuals are at risk of disease and psychological issues in that case.
Other elements also play a role in how susceptible an individual becomes to the diseases and stress induced inflammation. Hereditary factors, upbringing, early life experiences, the meanings given to certain situations, constitutional composition, and access to health care (including psychological support) all have a part in how vulnerable an individual is to the harmful effects of stress.
Before diving into these harmful effects, how they affect each other, how they trigger illness, and how to deal with them, we need to have a good understanding of how your body deals with stress.
The body has many different organs and systems that work together to fight stress. They are all part of the NeuroEndoMetabolic (NEM) Stress Response, which is composed of six organ / system circuits that are all affected by chronic stress and stress induced inflammation. We will go through each of these circuits and how each of them respond to stress and their association with inflammation.
The adrenal glands, the thyroid and the gonads (male testes and female ovaries) regulate, through the hypothalamic-pituitary-gonadal (HPG) axis as well as the hypothalamic-pituitary-adrenal (HPA) axis, the hormone response. The hypothalamus and pituitary gland in the brain send signals to these organs to produce or stop producing their hormones.
As we will discuss in more detail below, the adrenals are responsible for secreting the body’s main anti-stress hormone, cortisol. With consistent stress and stress induced inflammation, your adrenals will weaken and become unable to handle the stress, causing a very common yet usually under-diagnosed condition called Adrenal Fatigue Syndrome (AFS).
The metabolism response involves the thyroid, pancreas and liver. The thyroid is responsible for producing thyroid hormones to increase the basal metabolic rate when stress is present so that you can be ready and have the needed energy to deal with whatever threat is present. The pancreas produces insulin to help get your cells the glucose they need to give you a boost of energy when under stress, while the liver clears away excess metabolites generated as a result of metabolism.
Inflammation can affect metabolism and the metabolic response. If the pancreas is chronically inflamed, insulin producing cells may be affected. It will become more difficult as time passes for your body to regulate your blood sugar and reactive hypoglycemia can result. A constantly triggered inflammatory response can also get in the way of thyroid function, which can lower the production of thyroid hormones T3 and T4. At the same time, low T3 and T4 decreases metabolic function and contributes to inflammation.
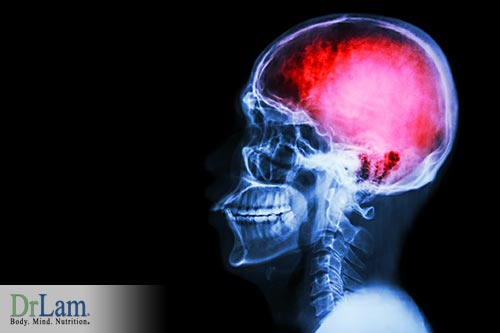
The neuroaffective? circuit consists of the autonomic nervous system (ANS), central nervous system (CNS), and gastrointestinal (GI) system. These systems rely on neurotransmitters to balance your body, mood, and emotions.
Many of these neurotransmitters are actually made in the gut of the GI system, which is why the gut is sometimes called “the second brain.” The gut, brain and ANS form the management team of the neuroaffective? response.
Stress affects the ANS, as well as the brain and gut. For example, when the gut’s health is compromised and there is inflammation present, its production of neurotransmitters is dysregulated and, by connection, the neuroaffective? response. This is one of the reasons why stress induced inflammation and gut health are things to look at if your mood and brain function are not optimal. Inflammation of the brain has also been connected to decreased mood and depression.
Readying the heart, lungs and blood vessels by providing more oxygen-filled blood is part of the fight or flight response. The hormones that turn this response on are cortisol, adrenaline and norepinephrine, which are all produced by the adrenal glands and regulated by the SNS.
When the cardionomic response is triggered, your heart rate goes up, breathing rate is faster and blood pumps through your system more vigorously so that it gives you the best chance at a strong fight or a fast escape. Norepinephrine and epinephrine (also called adrenaline) are the two catecholamines responsible to carry out this responsibility.
Chronic stress and the inflammation induced by it can weaken the adrenal glands and also keep the fight or flight response constantly switched on as the body is flooded with these catecholamines. When this happens, your cardionomic response is on overdrive and you can experience faster resting heart rate, heart palpitations, stronger heartbeats, irritable bowels, anxiety, panic attacks, temperature intolerance, and POTS-like symptoms. In severe cases, this can lead to atrial fibrillation, supraventricular tachycardia, and premature ventricular contractions.
Inflammation is one of the most effective and important defense mechanisms that your body has against injury and harmful intrusions by pathogens (such as bacteria, virus, parasites) or toxins. This mechanism involves the immune system, the microbiome, and the gut. The inflammation response creates a hostile environment for the harmful intruders, and it cleans away tissues and cells already damaged by the pathogens, the immune system’s attack, or from injury.
Just like stress induced inflammation, inflammation also affects your brain’s ability to respond to stress. Studies have shown that consistent low-grade inflammation increases the permeability of the gut lining, allowing toxins to enter the system and cause depression in the CNS.
SSRIs, which are common antidepressants, have anti-inflammatory properties that can help with this. If you suffer from depression, you might want to consider taking up an anti-inflammatory diet alongside your regular therapy. However, you should never discontinue medications in favor of this diet without the consent and supervision of your doctor.
A disruption in your inflammation response can also bring about recurring infections, autoimmunity, candida, GI tract disorders, stealth viruses, musculoskeletal pain, slow healing, and food sensitivities. It also puts a lot of pressure on your body’s detoxification response.
The debris left over from damaged and dead cells, whether from the inflammation response or oxidative stress, as well as any pathogens or toxins that entered the body, need to be cleared out of the system. The detoxification response involves the liver, extracellular matrix, lymphatic system, kidneys and immune system all working together to ensure anything that is not needed gets removed from the body as quickly and efficiently as possible.
 When consistent stress induced inflammation and unrelenting stressors burden your detoxification response, your body’s toxicity levels will inevitably rise as reactive metabolites accumulate. Symptoms of this include intolerance to certain medications, chemicals, foods, and supplements. Paradoxical reactions and brain fog have also been reported.
When consistent stress induced inflammation and unrelenting stressors burden your detoxification response, your body’s toxicity levels will inevitably rise as reactive metabolites accumulate. Symptoms of this include intolerance to certain medications, chemicals, foods, and supplements. Paradoxical reactions and brain fog have also been reported.
While each of the NEM circuits perform a specific function, the body has a built-in activation sequence when stress arrives at the doorstep. Not all circuits are activated at the same intensity. Some circuits are designed for chronic stress, while others are equipped for more acute situations. The first line of defense within the NEM stress response is the all-important HPA hormonal axis. The HPA axis is composed of the two regulatory control centers in the brain: the hypothalamus and pituitary gland, which secrete stimulatory neurotransmitters that signal the adrenal glands to produce cortisol, the body’s main anti-stress hormone.
Cortisol has many important functions, including regulating blood sugar, regulating heart rate, maintaining heart and blood vessel function, suppressing the immune system, and neutralizing inflammation.
With chronic stress and consistent stress induced inflammation, the adrenal glands begin to increase, and that can ultimately lead to dysregulation. At first, they increase their production of cortisol to meet the growing need for stress/inflammation neutralization. This brings on the symptoms of the first stages of AFS such as sugar craving, hypoglycemia, and low exercise tolerance. After some time, the adrenals become exhausted and their cortisol output drops, bringing about the symptoms of more advanced stages of AFS such as heart palpitations?, anxiety, insomnia, and brain fog.
Without proper cortisol’s anti-inflammatory role, inflammation, including that which is induced by stress, can run rampant. Also, all of the other functions that are under cortisol’s regulation are adversely affected, and that is why AFS can have such a wide range of symptoms.
Symptoms of AFS range from mild to severe. They include fatigue, an inability to fall asleep, waking up in the middle of the night, difficulty getting up in the morning, easily gaining weight and difficulty losing it, low libido, reactive hypoglycemia, food sensitivities, drug sensitivities, PMS, fertility issues, anxiety, heart palpitations, mild depression, and frequent colds and flus.

Many of these symptoms are either directly related to inflammation, or can aggravate the state of inflammation in the body.
So far, we have studied the negative effect of uncontrolled inflammation. Let us back up and examine in more detail now exactly what inflammation is and why it is an important part of our well-being.
© Copyright 2018 Michael Lam, M.D. All Rights Reserved.
We’ve known for years that stress can create physical and psychological disorders, but now we understand the main link is that stress induced inflammation is the underlying cause. Understanding this link and knowing what to do about it is key to good health.

