 The term “microbiome” refers to microorganisms (microbiota) and their genomes that exist in and on the human body. This includes millions of bacteria, fungi, viruses, parasites, and protozoa. Each human has roughly 600,000 genes from microbes, compared to only 23,000 from human sources. The gut microbiome has diverse microbial inter-species interactions that can be either beneficial or harmful. One example of an interaction between this is the microbiome and CFS (Chronic Fatigue Syndrome).
The term “microbiome” refers to microorganisms (microbiota) and their genomes that exist in and on the human body. This includes millions of bacteria, fungi, viruses, parasites, and protozoa. Each human has roughly 600,000 genes from microbes, compared to only 23,000 from human sources. The gut microbiome has diverse microbial inter-species interactions that can be either beneficial or harmful. One example of an interaction between this is the microbiome and CFS (Chronic Fatigue Syndrome).
Myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS) is a chronic illness affecting up to 24 million people globally, for which there is currently no specific therapies. Chronic fatigue syndrome (CFS), or myalgic encephalomyelitis, is a long-term condition characterized by unexplained debilitating fatigue or exhaustion, brain fog or cognitive dysfunction, and gastrointestinal disturbances.
Other symptoms of CFS include:
Chronic Fatigue Syndrome (CFS) and Adrenal Fatigue Syndrome (AFS) are interconnected through the NeuroEndoMetabolic (NEM) Stress Response system, a comprehensive framework that describes how different systems of the body interact in response to stress. The NEM stress response encompasses six circuits—neuroaffective, metabolic, hormonal, cardionomic, inflammation, and detoxification—each involving various organs and pathways. Both CFS and AFS can be viewed as manifestations of an overwhelmed or dysregulated NEM stress response.
In the case of AFS, the hormonal circuit, which includes the adrenal glands, becomes imbalanced. Stress hormones like cortisol may be produced in suboptimal levels, affecting the body's ability to handle stress and contributing to persistent fatigue. Similarly, CFS, although not fully understood, may be related to abnormalities in the neuroaffective and metabolic circuits of the NEM stress response system. Both conditions might involve multiple circuits, including the inflammation and detoxification circuits, thereby explaining their wide range of symptoms, including unrefreshing sleep, cognitive difficulties, and exercise intolerance.
The exact cause of Chronic Fatigue Syndrome remains a mystery, although it has been associated with viral infections. However, research indicates that in individuals with ME/CFS, there can be significant rewiring of the bacterial networks in the microbiome.
New studies suggest that there is a link between the human microbiome and CFS. Based on the findings of a recent study, there might be a link between the degree of health-promoting gut bacteria and the severity of fatigue symptoms. A study published in the journal Cell Host & Microbe suggests that the health-promoting gut bacterium Faecalibacterium prausnitzii may significantly reduce exhaustion in persons who experience CFS (Guo).
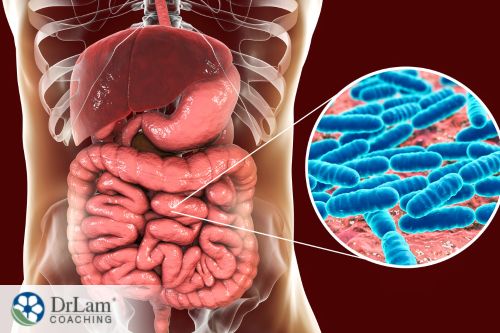
Researchers measured the level of a specific bacteria in fecal samples taken from 106 CFS patients. The results were compared to 91 healthy subjects to see how gut microbiomes differ between the two. Subsequently, findings revealed that levels of the gut bacteria F. prausnitzii and Eubacterium rectale were decreased in CFS subjects. These two can be categorized as “good” bacteria. Furthermore, they play a critical role in the production of butyrate.
Butyrate, which is a gut microbial metabolite, plays a key role in the health of the gut microbiome and is linked to mucosal immune regulation. Specifically, it’s a fatty acid in the gastrointestinal microbiome that helps to break down fiber. Microbiome diversity can be altered in CFS patients, and microbes that produce butyrate can be reduced.
Reduced butyrate levels in persons with CFS could lead to inflammation in the gut and a weakened gut barrier. This combination could trigger an inflammatory response that extends from the gut to the brain. Additionally, decreased level of butyrate is linked to several diseases, including colon cancer, inflammatory bowel disease (IBS), and insulin resistance.
Furthermore, lower levels of the bacteria F. prausnitzii are also associated with the severity of fatigue CFS symptoms. Still, it is unknown whether a decrease in F. prausnitzii is a cause or consequence of CFS.
A different 2023 study in Cell Host & Microbe analyzed gut microbiome-host interactions in short- and long-term chronic fatigue syndrome patients (Xiong). Findings revealed that:
As such, these findings indicate that the immune system becomes disrupted in patients with CFS. Furthermore, they point to the possibility that microbiome abnormalities may lead to an abnormal immune response over time.
This study suggested that the mechanism of the problem may be because:
The exact cause of low butyrate-producing bacteria in CFS is unclear. However, low levels of physical activity could play a role in this problem. Recent studies suggest that physical exercise stimulates butyrate-producing bacteria that are low in CFS. One study found an association between reduced butyrate levels and fatigue, which suggests that the lower activity levels of more fatigued individuals with CFS may contribute to lower butyrate levels.
Still, there are several possibilities including, reduced gut motility, blood flows to the gut, as well as reduced circulation of bile acids. Furthermore, low butyrate levels are found in a variety of conditions, such as inflammatory bowel disease (IBD), IBS, celiac disease, colorectal cancer, and obesity. As such, it may be safe to say that low activity levels are not responsible alone for all the gut issues in individuals with CFS.
The connection between the microbiome and CFS appears to be multifaceted, and when irritable bowel syndrome (IBS) is thrown into the mix, it becomes even more complex.
IBS is a common, but not a universal comorbid condition present in persons with CFS. It’s characterized by symptoms such as abdominal pain, bloating, or cramping typically associated with a bowel movement or changes in the appearance of stool (e.g. hard-packed or diarrhea), and frequency of bowel movement.
When looking and the microbiome and CFS, studies indicate that having IBS with CFS can make a significant difference in the diversity of your gut microbiome. Specifically, whether CFS patients had or didn’t have IBS showed in the alpha diversity of the gut bacteria. In this case, alpha diversity refers to the diversity of the complex ecosystems of the gut. In fact, the higher the species alpha diversity of the bacteria in your gut, the greater its health, resiliency, and productivity should be. However, research findings suggest that some CFS patients’ gut ecosystems are not as diverse and resilient as others.
 The body’s microbiome plays a significant role in your overall health. Early research findings suggest that a person’s microbiota has a direct effect on several diseases, such as asthma, celiac disease, cancer, diabetes, inflammatory bowel disease, and heart disease. A dysfunction between the microbiome and the host is connected to these diseases.
The body’s microbiome plays a significant role in your overall health. Early research findings suggest that a person’s microbiota has a direct effect on several diseases, such as asthma, celiac disease, cancer, diabetes, inflammatory bowel disease, and heart disease. A dysfunction between the microbiome and the host is connected to these diseases.
As such, there seem to be potential mechanisms whereby your microbiome can impact your immune system. The highest levels of microbes and lymphoid tissue that support immune responses are found in your GI tract. Here, the immune system and the microbiota have a harmonious relationship.
According to an article published in the Journal of Clinical & Cellular Immunology, your body’s immune system benefits from the microbiome because it helps the body resist the colonization of pathogens. However, it’s also possible for the microbiome to alter the body’s response to a particular pathogen and limit the efficiency of prescription drugs and how well your immune system functions.
As such, the relationship between the immune system, the microbiome and CFS is a complex one and requires more research before much can be said about what may cause observed changes.
One thing can be said for certain though: that CFS is not just in your head. Research findings point to biological markers for CFS in gut bacteria and inflammatory microbial agents in the blood. A study published in the journal Microbiome describes researchers correctly identifying CFS in 83 percent of patients through stool samples and blood work. This gave the researchers the opportunity to provide a noninvasive examination and some level of understanding regarding the cause of CFS.
Researchers made two significant findings:
Thus, CFS is not merely in your imagination. It is characteristic of significant gastrointestinal and inflammatory changes. Signs of a biological abnormality provide evidence against the notion that the disease is only psychological in nature. There are significant physiological differences between individuals with CFS and those who do not suffer from the condition.
To date, there is no specific therapies or known ways to remove CFS. However, different remedies and lifestyle changes have been used to ameliorate and manage CFS symptoms.
Some options that are usually recommended include:
A different set of therapies for CFS may be implicated by the relationship between the microbiome and CFS. One bacterium in particular, Faecalibacterium prausnitzii, is implicated in the health of the microbiome and CFS. Supporting these bacteria may thus help symptoms.
An adequate intake of pectins seem to stimulate the growth of various beneficial bacteria, including Bifidobacterium, Lactobacillus species, Faecalibacterium prausnitzii, and Eubacterium rectale. Pectins are complex, plant-derived carbohydrates that cannot be digested by human enzymes. However, they can be easily broken down by certain commensal bacteria in your gut.
Inulin is another prebiotic that can be used to increase the level of F. prausnitzii in the intestinal microbiota.
 Probiotics are “friendly” microorganisms, usually bacteria or yeasts, that reside in the gastrointestinal tract or on other mucosal surfaces. They exert beneficial effects on your health. Some significant probiotic benefits for your microbiome and CFS include:
Probiotics are “friendly” microorganisms, usually bacteria or yeasts, that reside in the gastrointestinal tract or on other mucosal surfaces. They exert beneficial effects on your health. Some significant probiotic benefits for your microbiome and CFS include:
There are many different strains that can be beneficial in reducing inflammation, supporting the immune system, and preventing the growth of bad bacteria. These include:
However, it is essential that you talk to your healthcare provider before taking any of these supplements. Discuss with your healthcare provider the possible benefits and harms of any remedy, such as medicines and other therapies.
These Dr Lam supplements may help support gut health and your microbiome through CFS. However, don't take any new supplements without talking to a doctor first.
Adrezyme is a proprietary formulation that’s packed with a variety of enzymes. These enzymes help with the breakdown of fat, carbohydrates, proteins, dairy, grains, and indigestible fibers.
Glutelyze is a digestive enzyme formula that supports the digestive process, by digesting gluten and carbohydrates. It breaks down difficult-to-digest proline-containing peptides, found in dairy products and cereal grains.
Stomazyme is a proprietary blend containing a combination of enzymes, as well as betaine hydrochloride and ox bile extract. It helps to support healthy digestion and has the potential to aid with the production of stomach acid, greater bile production, and the breakdown of carbs, fat, and proteins.
Pro-B is a potent probiotic formula that contains Lactobacillus acidophilus, which helps with digestion and supports healthy skin and the health of your immune system. Also, it’s beneficial in maintaining the "good bacteria" in your gut that support proper digestion and absorption of nutrients from food. Additionally, it can help you to maintain healthy intestinal flora and help support a balanced mycobiome.
Pro-Y contains Saccharomyces boulardii, which is a strain of yeast with probiotics benefits. It may support a healthy gut flora balance, as well as the health and balance of the intestinal tract against environmental and internal stressors.
The human microbiome and CFS are connected, in that changes in the microbiome are correlated to the condition. As such, it’s essential that the microbiome's health be maintained and the growth of good bacteria is supported. If you think you may have CFS and are unsure about your symptoms, Dr. Lam's Adrenal Fatigue Recovery Program can help you! In this program, you'll learn how to use supplements, which foods to eat, which exercises are best for you, and about your stage of adrenal fatigue. This course focuses on helping you make informed choices and avoid the pitfalls Dr. Lam faced in his recovery journey.
Adrezyme: Boosting Your Energy and Balancing Your Microbiome!
Cornell University. (2016, June 27). Chronic fatigue syndrome is in your gut, not your head. ScienceDaily. Retrieved June 2, 2023 from www.sciencedaily.com/releases/2016/06/160627160939.htm
Groeger, D., O'Mahony, L., Murphy, E. F., Bourke, J. F., Dinan, T. G., Kiely, B., Shanahan, F., & Quigley, E. M. (2013). Bifidobacterium infantis 35624 modulates host inflammatory processes beyond the gut. Gut microbes, 4(4), 325–339. https://doi.org/10.4161/gmic.25487
Giloteaux, L., Goodrich, J.K., Walters, W.A. et al. Reduced diversity and altered composition of the gut microbiome in individuals with myalgic encephalomyelitis/chronic fatigue syndrome. Microbiome 4, 30 (2016). https://doi.org/10.1186/s40168-016-0171-4
Guo, C., Che, X., Briese, T., Ranjan, A., Allicock, O., Yates, R. A., Cheng, A., March, D., Hornig, M., Komaroff, A. L., Levine, S., Bateman, L., Vernon, S. D., Klimas, N. G., Montoya, J. G., Peterson, D. L., Lipkin, W. I., & Williams, B. L. (2023). Deficient butyrate-producing capacity in the gut microbiome is associated with bacterial network disturbances and fatigue symptoms in ME/CFS. Cell Host & Microbe, 31(2), 288-304.e8. https://doi.org/10.1016/j.chom.2023.01.004
Rivera-Amill V. (2014). The Human Microbiome and the Immune System: An Ever Evolving Understanding. Journal of clinical & cellular immunology, 5(6), e114. https://doi.org/10.4172/2155-9899.1000e114
Roman, P., Carrillo-Trabalón, F., Sánchez-Labraca, N., Cañadas, F., Estévez, A. F., & Cardona, D. (2018). Are probiotic treatments useful on fibromyalgia syndrome or chronic fatigue syndrome patients? A systematic review. Beneficial microbes, 9(4), 603–611. https://doi.org/10.3920/BM2017.0125
Xiong, R., Gunter, C., Fleming, E., Vernon, S. D., Bateman, L., Unutmaz, D., & Oh, J. (2023). Multi-'omics of gut microbiome-host interactions in short- and long-term myalgic encephalomyelitis/chronic fatigue syndrome patients. Cell host & microbe, 31(2), 273–287.e5. https://doi.org/10.1016/j.chom.2023.01.001
Yao, S., Zhao, Z., Wang, W., & Liu, X. (2020). Bifidobacterium Longum: Protection against Inflammatory Bowel Disease. Journal of Immunology Research, 2021. https://doi.org/10.1155/2021/8030297
The connection between the microbiome and CFS is not fully understood. However, research suggests that an altered microbiome with low levels of butyrate triggers inflammation. Furthermore, levels of the gut bacteria F. prausnitzii and Eubacterium rectale seem to decrease in CFS subjects.