 You probably already know that what you eat can affect your gut health. But new research is showing that what you eat, and even where you live, can have a huge effect on your microbiome, and consequently, your health. According to a recent study, there may be a close correlation between immigration and gut microbiome health, and this could help explain some of the origins of the obesity epidemic. This study focused on specific populations and detailed the findings per group. Besides an increased rate of metabolic conditions, the study found that obesity amongst these specific populations also increased.
You probably already know that what you eat can affect your gut health. But new research is showing that what you eat, and even where you live, can have a huge effect on your microbiome, and consequently, your health. According to a recent study, there may be a close correlation between immigration and gut microbiome health, and this could help explain some of the origins of the obesity epidemic. This study focused on specific populations and detailed the findings per group. Besides an increased rate of metabolic conditions, the study found that obesity amongst these specific populations also increased.
One study on how immigrating to the United States changed gut microbial compositions gave numerous insights into how the microbiome could be influenced by its environment.
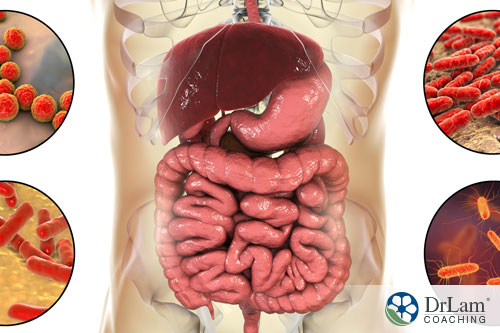
With regards to immigration and gut microbiome, it was found that these immigrants immediately started losing many of their native microbes once arriving on United States soil, with many new microbes replacing them. The new microbes, however, were not as diverse as those found in the immigrants’ places of origin and seem to have ties with obesity.
People from developing countries tend to have a much greater diversity in their gut microbiome than those living in the United States or other Western countries. This study, however, indicates the astonishing degree that this biodiversity is lost as soon as the American diet and lifestyle are introduced.
The research into immigration and gut microbiome targeted two groups of Southeast Asia immigrants and refugees. These are the Karen and Hmong people. These two ethnic minorities have large communities in Thailand. Their origins, however, are in China and Burma. These two groups were specifically chosen because of their large communities in Minnesota. This made drawing comparisons between the immigrants and their counterparts in Asia an easier undertaking.
 Researchers compared the discrepancies in immigration and gut microbiome of five groups. The first group was Hmong and Karen people who were living in Thailand. The second group consisted of those who had already immigrated to the United States. The third group was the children of the Karen and Hmong people who had already immigrated. The fourth was a Caucasian control group. The fifth and last group consisted out of 19 Karen refugees who were in the relocation process. The last group was included so that the changes with regards to immigration and gut microbiome could be tracked during their first six to nine months in the United States. For this group, the change in gut microbiota was astounding. Western bacteria speedily began displacing non-Western bacterial strains.
Researchers compared the discrepancies in immigration and gut microbiome of five groups. The first group was Hmong and Karen people who were living in Thailand. The second group consisted of those who had already immigrated to the United States. The third group was the children of the Karen and Hmong people who had already immigrated. The fourth was a Caucasian control group. The fifth and last group consisted out of 19 Karen refugees who were in the relocation process. The last group was included so that the changes with regards to immigration and gut microbiome could be tracked during their first six to nine months in the United States. For this group, the change in gut microbiota was astounding. Western bacteria speedily began displacing non-Western bacterial strains.
Beyond this initial displacement, however, the westernization of the gut tended to continue for at least the first ten years of an immigrant’s advent into the US, with their gut microbe diversity steadily declining. While diet seemed to play an important role in this change, it could not, however, account for all the changes noticed in the study. Many immigrants still ate a very different diet than that of the typical Caucasian. Besides a change in gut microbiome, obesity and diabetes were also more pronounced in those who had immigrated to the USA than their counterparts who had stayed in Thailand.
For second-generation immigrant children born in the U.S.A., the changes tended to be more pronounced than in their parents. The research could not ascertain whether this continued change in gut microbiome was due to environmental factors or whether it is due to these children being exposed to a diet that is more typical of the US. What could be ascertained, however, was that the loss of gut microbiome diversity is not only limited to first-generation immigrants but spans generations.
The research does indicate is that immigration and gut microbiome are correlated, resulting in loss of microbiome diversity and an increased risk of developing obesity and diabetes. And in addition to immigration and gut microbiome diversity, enzymes are also affected.
Enzymes are responsible for breaking down food in your digestive tract. When your body is lacking in enzymes, a certain set of symptoms manifest. Amongst these are bloating, fat gain, and even brain fog, to name but a few. Usually, the enzymes we carry affect the food we are able to digest. An enzyme production discrepancy is usually the result of inflammation. This could be the result of food intolerances, irritable bowel syndrome (IBS), or low stomach acid. Inflammatory conditions within your gut could also affect your pancreatic function, and thus influence your chances of developing diabetes.
Interestingly, one of the microbial strains looked at in the study was Prevotella. This microbial strain is particularly useful in the digestion of coconut, palm, and tamarind, foods the immigrants ate while living in Asia. Of course, if you do not eat any of these foods, these microbes would no longer be found in your digestive tract. But while your diet may play a role in your gut microbiome composition, the changes seen with regards to these immigration and gut microbiome diversity outstripped the rate at which the diets of the immigrants became Westernized. This would suggest something else is also involved, such as medication or environmental factors, for instance.
One thing, however, is for certain. American gut microbiomes are not as diverse as that of people living in a developing country. And when it comes to immigration and gut microbiome, exposure to a Westernized diet plays a large role in reducing the diversity of microbial compositions.
Stress may very well be the single largest influence on your digestive health. And this stress is not only the result of strain from work or a relationship. It may also be the result of physical or environmental factors. Stress, in fact, typically puts your body into a state of alertness, or fight or flight mode, where those processes needed to combat a threat are put into higher gear, and processes such as digestion that are not deemed important for your immediate survival are put on hold or slowed down.
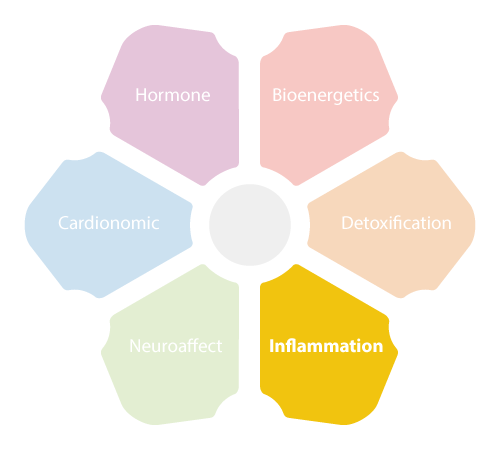 Your body’s response to stress is known as the NeuroEndoMetabolic (NEM) Stress Response and is governed by your hypothalamic-pituitary-adrenal (HPA) axis. The many, diverse chemical reactions that compose your stress response result in your body producing higher levels of cortisol. When stress is chronic, your cortisol production in the adrenals stays at higher levels, but the possible end results to your body can be devastating.
Your body’s response to stress is known as the NeuroEndoMetabolic (NEM) Stress Response and is governed by your hypothalamic-pituitary-adrenal (HPA) axis. The many, diverse chemical reactions that compose your stress response result in your body producing higher levels of cortisol. When stress is chronic, your cortisol production in the adrenals stays at higher levels, but the possible end results to your body can be devastating.
Your gut’s health is largely determined by its microbiome, or the types of bacteria and the ratio between good and bad bacteria. These bacteria and their enzymes are important for:
Stress of any type may result in inflammation. Stress also results in increased cortisol production that, in turn, acts as an inflammation suppressant. Chronic stress, however, and the corresponding inflammation suppression that may go with it, may serve to negatively impact your body’s immune response. A suppressed immune response may leave you open to all kinds of infections, resulting in increased stress and increased inflammation response. Thus, your body’s inflammation, stress, and immune responses go into a continuing downward spiral, with possible chronic health conditions as a result. You may, for instance, become more susceptible to colds and flu, develop certain food allergies, alternate between loose and hard stools, develop cancer, or experience a number of digestive issues.
When it comes to digestive issues, chronic inflammation may have a debilitating effect on gut health, as your microbiome and digestive enzymes may both be impacted.
Symptoms commonly associated with a compromised gut include, amongst many others:
IBS has its own set of symptoms associated with it. Amongst these we find:
A balanced gut microbiome is thus of the utmost importance when it comes to continued good health, not only for gut health but for that of our entire body.
 We basically have our mothers to thank for our gut microbiome. A fetus, before being born, has a sterile gut. During the process of giving birth, a mother’s vaginal and fecal microbiome are transferred to the baby. The baby receives environmental microbes in the days after his birth.
We basically have our mothers to thank for our gut microbiome. A fetus, before being born, has a sterile gut. During the process of giving birth, a mother’s vaginal and fecal microbiome are transferred to the baby. The baby receives environmental microbes in the days after his birth.
There are, however, numerous factors that may influence the newborn’s gut microbiome health. Breastfeeding, for example, plays a positive role in gut microbiome development.
By the time a child is three years old, their gut microbiome should be stabilized. This does not mean that no further changes and balances could take place throughout their lives. Your body always strives for a state of balance, and your gut microbiome may change depending on conditions.
One of these changing conditions is the aging process, which is often accompanied by increased inflammation due to a decrease in gut microbial diversity.
In the case of immigration and gut microbiome connections, we see different factors come into play. For the Hmong and Karen immigrants mentioned, their microbiome diversity may have changed due to a different diet and lifestyle, although other factors also seemed to be involved. For their children born in the USA, they received microbiomes from their mother during the birthing process. However, as they developed, so too did their gut microbiome according to their environment and diet.
Of course, as was mentioned in the study, many other factors that are, as yet, undetermined may also come into play. One of the factors not mentioned is the effect of stress, whether from environmental or other sources. Of itself, stress may be one of the major factors influencing continued gut health and possibly gut microbiome diversity. However, the loss of some gut bacteria, such as Prevotella, seemed to be caused by diet changes, according to the study.
As seen with the Hmong and Karen immigration and gut microbiome study, your gut microbiome composition plays a large role when it comes to your continued health. But while there are many stressful factors that work to compromise your gut microbiome stability, there are a few measures you can take to help enhance not only your gut microbiome composition but your continued good health.
Diet plays a huge role, with evidence suggesting that probiotics, prebiotics, and fermented foods such as kimchi benefit the gut, helping produce more vitamins, enzymes, and amino acids. Vegetables, whole grains, and fruits are also recommended. On the other hand, one should stay away from refined foods, processed sugar, GMO’s, and artificial sweeteners as these may harm the friendly flora in your gut.
 Exercise may also play a role, as athletes, on the whole, tend to have a richer gut microbiome than their sedentary counterparts. Exercise, of course, may not necessarily mean the high impact kind. Low-impact exercise such as walking or weight training is just as effective, especially in someone whose adrenals may be compromised due to stress.
Exercise may also play a role, as athletes, on the whole, tend to have a richer gut microbiome than their sedentary counterparts. Exercise, of course, may not necessarily mean the high impact kind. Low-impact exercise such as walking or weight training is just as effective, especially in someone whose adrenals may be compromised due to stress.
Sleep is another important aspect of supporting gut health, as this is the time when your body heals. Getting enough good quality sleep is one of the mainstays for good health. Here, an established bedtime routine may be of immense value.
Besides those mentioned, the practice of mindfulness, meditation, and yoga are also often recommended for reducing stress and improving gut health.
At the end of the day, however, it is up to you. Your gut and microbiome play a huge role even in adrenal fatigue recovery, which is why the gut is often addressed first during the recovery process. This does not apply to everyone with adrenal fatigue, however, which is why it is important to seek out an adrenal fatigue specialist who can put you on the right path of recovery specifically for your body. By taking measures to support your gut health, you are supporting all body systems.
© Copyright 2020 Michael Lam, M.D. All Rights Reserved.
According to research, there is a correlation between immigration and gut microbiome issues. This study, on a population of Hmong and Karen immigrants, showed their gut microbiome diversity declined once they moved to the USA. Instances of obesity and diabetes also seemed to increase during this time.
