Your gastrointestinal (GI) tract is the foundation of your health. If it is working well, your body gets the nutrition and energy it needs, your hormones and neurotransmitters are in balance, and your wellbeing thrives. If it’s not working well, you’re at risk of conditions like food and drug sensitivities and general ill-health. That’s why GI repair is one of the most important steps to good health you can take. So let's explore these and other areas in more detail.
Your gastrointestinal (GI) tract is the foundation of your health. If it is working well, your body gets the nutrition and energy it needs, your hormones and neurotransmitters are in balance, and your wellbeing thrives. If it’s not working well, you’re at risk of conditions like food and drug sensitivities and general ill-health. That’s why GI repair is one of the most important steps to good health you can take. So let's explore these and other areas in more detail.
Although your GI tract is linked to your entire NeuroEndoMetabolic (NEM) stress response, it is directly involved in your Inflammation Circuit. It’s composed of six circuits of organs and systems that work together, and they are the Hormone, Bioenergetics, Cardionomic, Neuroaffect, Inflammation, and Detoxification Circuits.
In this article, we’ll focus on your Inflammation Circuit as it is the one most involved when it comes to GI repair. We’ll also talk about how GI repair and adrenal fatigue recovery must go hand-in-hand, otherwise, your recovery will not be complete.
Adrenal Fatigue Syndrome (AFS) is a condition characterized by an initial rise in cortisol levels, then an eventual drop when in the more advanced stages. AFS can bring about the following symptoms: fatigue, weight gain, insomnia, brain fog, anxiety, mild depression, food and drug sensitivities, low libido, hair loss, PMS, infertility, dry skin, hypoglycemia, salt and sugar cravings, an inability to handle stress, heart palpitations, unstable blood pressure, and dizziness when standing up from a prone position.
Your adrenal glands are part of your NEM’s Hormone Circuit, but they do play a role when it comes to the gut and inflammation, as we will see.
Your GI tract is one of the biggest interfaces you have with the outside world. It is how your body gets the nutrients and fuel it needs. But it also helps filter out pathogens and toxins. In many traditional medical systems, it is considered the most important player in your overall health. And mainstream medical science is now catching on to this ancient wisdom.
 In your gut, you have your gut microbiome, which is the ecosystem of flora that either helps or harms the way your gut functions. A healthy microbiome is diverse and has enough “good” bacteria to keep the “bad” bacteria in check.
In your gut, you have your gut microbiome, which is the ecosystem of flora that either helps or harms the way your gut functions. A healthy microbiome is diverse and has enough “good” bacteria to keep the “bad” bacteria in check.
Unfortunately, your microbiome can go out of balance from several factors. This is a state called dysbiosis and it can be the result of certain stressors, such as:
Physical and psychological stress have a similar effect on the NEM stress response. They both trigger a stress response. And the first responders to stress are always your adrenal glands. They secrete cortisol, which is your body’s main anti-stress hormone, along with other important anti-stress hormones.
And although one of the functions of cortisol is to neutralize inflammation, if stress is chronic, it will make cortisol levels go consistently outside the normal range, which will create more inflammation.
Dysbiosis and inflammation are directly linked. When your microbiome is out of balance, it can lead to the tight junctions in your gut lining to loosen and create leaks. These leaks can then allow particles and pathogens into your bloodstream that shouldn’t be there. This prompts an immediate immune response, which creates inflammation. And if this issue continues, you can end up with Leaky Gut Syndrome and other GI organ dysfunctions.
These issues make up the three main areas we need to look at when planning GI repair: dysbiosis, leaky gut and other GI organ dysfunctions, and pathogen entry. Each one will have different lab tests and markers, and also a slightly different approach to GI repair.
The problem with this cycle is that for many people, they don’t even know that they’re doing something to cause inflammation and leaky gut. For example, not all allergenic foods cause gastrointestinal symptoms. In many cases, the inflammation that arises from a leaky gut can travel to other areas of the body causing issues there.
Inflammation that reaches the joints can cause joint pain, inflammation that reaches the skin can create inflammatory skin conditions, and inflammation that reaches the brain and nervous system can cause psychiatric and neurological symptoms.
So, when you don’t get direct GI tract symptoms, you are less likely to seek the tests needed and to begin GI repair work. But by reading this article, you will have a better understanding of what you might need to look for and what to do.
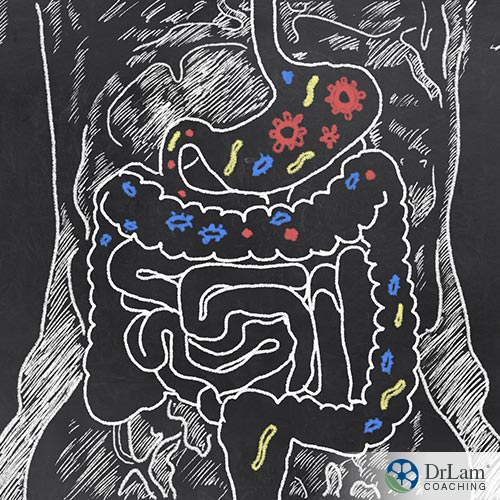 Your Inflammation circuit is composed of your immune system, GI tract, and microbiome. It is activated as a defense against the presence of any harmful stimuli, such as pathogens, toxins, abnormal cells, or injury. The role of inflammation is to get rid of such stimuli, as well as any tissues and cells damaged by them.
Your Inflammation circuit is composed of your immune system, GI tract, and microbiome. It is activated as a defense against the presence of any harmful stimuli, such as pathogens, toxins, abnormal cells, or injury. The role of inflammation is to get rid of such stimuli, as well as any tissues and cells damaged by them.
Although inflammation is a natural and healthy part of your immunity, if it becomes chronic, it can be the cause of a lot of damage. Chronic inflammation is a root cause of many chronic diseases, including those of the GI tract, such as inflammatory bowel disease (IBD), irritable bowel syndrome (IBS), and food sensitivities.
Other symptoms of chronic inflammation include candida, recurring infections, autoimmunity, the presence of stealth viruses, slowed healing, and difficulty recovering from Lyme disease.
Dysbiosis is often the first event in the chain of GI dysfunction, and you can check for it through the following lab markers:
If your SCFAs are low, you’ll need to increase your fiber intake. Especially insoluble fiber. Prebiotic supplements can also help. More specifically, a butyrate supplement might be quite useful here. The most common type is sodium butyrate.
Butyrate, which is also sometimes called butyric acid, is one of the three most common SCFA found in your gut. It’s made by your gut bacteria, but if you have dysbiosis, then that may mean your gut bacteria is not making enough. So a supplement could help until your microbiome rebalances. You can also try to eat butyrate-rich foods, like butter and ghee, but the amount you’d be getting is nowhere near enough for GI repair.
Sauerkraut, which is fermented cabbage, is another source of butyric acid. Other fermented foods include kimchi, yogurt, and kefir, and they can be just as good for your microbiome.
 But one thing we’d advise you to keep in mind when considering fermented foods is that some of them, especially kimchi, can be quite high in sodium. This is not a big problem for AFS since AFS can cause an imbalance of the potassium-sodium mineral ratio. We sometimes even encourage our clients to add a dash of salt in their drinking water to try to rebalance these minerals and to reduce potassium-rich foods for that purpose as well. But too much sodium and you might overshoot in the other direction. And any mineral imbalance can aggravate AFS.
But one thing we’d advise you to keep in mind when considering fermented foods is that some of them, especially kimchi, can be quite high in sodium. This is not a big problem for AFS since AFS can cause an imbalance of the potassium-sodium mineral ratio. We sometimes even encourage our clients to add a dash of salt in their drinking water to try to rebalance these minerals and to reduce potassium-rich foods for that purpose as well. But too much sodium and you might overshoot in the other direction. And any mineral imbalance can aggravate AFS.
As for polyphenols, if your levels are low, then you need to add more fruits and vegetables to your diet. But, again, if you have AFS, you’ll need to stick with the adrenal fatigue guidelines on fruit and vegetable intake. First of all, you’ll want to limit or avoid eating fruits that are high in sugar and high in potassium. Generally, we recommend that vegetables make up 30% to 40% of your diet (partially raw, half-cooked) and fruits make up 10% to 15% of your diet.
And if the commensal bacteria in your microbiome are not enough, you might have to reinforce with a probiotic. Unfortunately, most probiotic supplements are not very effective at diversifying your microbiome. That’s because most of them come from two strains: Lactobacillus and Bifidobacterium lactis.
But spores, such as Bacillus subtilis, are more useful for the diversification of your gut bacteria. They can also help tighten the junctions in your gut lining. Which brings us to the second important area of GI repair.
Dysbiosis leads to leaky gut. But other GI organ dysfunctions can also arise. These include low stomach acid production, low bile production, low digestive enzyme production, and issues with motility and absorption.
Some lab markers that can help determine whether you have some of these issues include the following.
Also, a total protein test can help check for different conditions that affect your protein levels, including GI tract problems.
 Take a look at the above list of stressors that contribute to dysbiosis. You might want to keep a food and medication journal for two weeks to help you. Are there things on that list that you’re doing consistently? Taking an NSAID painkiller once every few months for a random headache shouldn’t be a problem. But if you’re taking them regularly, that might be something to consider.
Take a look at the above list of stressors that contribute to dysbiosis. You might want to keep a food and medication journal for two weeks to help you. Are there things on that list that you’re doing consistently? Taking an NSAID painkiller once every few months for a random headache shouldn’t be a problem. But if you’re taking them regularly, that might be something to consider.
Antibiotics, on the other hand, can create some degree of dysbiosis from just one course, and it can take months to recover from. Eating an unhealthy diet is usually a lifestyle and not a one-time thing, so that would also be something to keep in mind.
Once you have a clear picture of what the causal issues are, you can take the necessary steps to fix them. Most likely, you will find that there are several causal issues you need to address. And generally speaking, changing your diet will help you address them at the same time.
What’s good about this approach is that it can also help with adrenal fatigue and NEM dysregulation. All of the above stressors don’t only cause issues with your microbiome. They also trigger adrenal fatigue, Inflammation circuit dysfunction, and overall NEM disturbance. And changing your diet is the biggest and most important step of adrenal fatigue recovery and NEM rebalancing.
There are three main ways to address digestive issues and leaky gut. The first is, of course, changing your diet. You have already started the process in GI Repair Step 1, and if you have AFS, the adrenal fatigue diet is the foundation of GI repair as well as adrenal fatigue recovery. You may have also added some fermented foods to boost your microbiome. That would be enough, but you can now also consider adding bone broth to speed up the sealing of the gut lining leaks.
The second way is to change the way you eat, not just what you eat. For starters, chewing your food properly will go a long way. Also, consider the setting in which you eat. Are you eating mindfully, in a calm environment, taking your time to taste and enjoy your meal? Or are you rushing through while working at your desk or watching a TV show?
The third way is to address the specific issues that you tested with the above lab markers using supplements. For low stomach acid, an HCL supplement would help. For low levels of digestive enzymes, you might consider taking a digestive enzymes supplement. These issues are common to occur with adrenal fatigue as the gut utilizes a lot of energy to keep things going, the energy that your adrenal glands help to create.
Several types of pathogens can infect your gut:
All of these issues can cause inflammation in your gut and are also big stressors on your entire system. Stealth and recurring infections can cause AFS and NEM dysfunction, and you will not be able to fully recover from your adrenal fatigue if they continue. So it is of utmost importance to address them.
 Many mainstream doctors will prescribe you a regular antibiotic for these gut pathogens, but we don’t recommend them as a first choice. That’s because, once again, they can lead to dysbiosis. Dysbiosis can then cause more leaks, which can then allow more pathogens in. And the cycle would continue.
Many mainstream doctors will prescribe you a regular antibiotic for these gut pathogens, but we don’t recommend them as a first choice. That’s because, once again, they can lead to dysbiosis. Dysbiosis can then cause more leaks, which can then allow more pathogens in. And the cycle would continue.
Herbal antimicrobials would be a much better option to start with. And they can be quite effective if you also change your diet and lifestyle.
But you should not, under any circumstances, take this step, or any of the other steps in GI repair, without proper supervision. We mentioned many dietary changes and supplements in this article, but if you have AFS, you are very susceptible to paradoxical reactions and even adrenal crashes. So you need the guidance of an experienced professional to avoid such problems. Antimicrobials can be quite potent. If not taken under proper supervision, they can lead to a crash and worsen the situation.
Your gut is your body’s fortress. It's what breaks down food into nutrients and glucose for energy, allows them in while it prevents harmful substances from entering your bloodstream. If there is any dysfunction, it can create a lot of inflammation and lead to adrenal fatigue.
So you must make GI repair your top health priority. And you can do so by looking at three main areas: your microbiome (for dysbiosis), your GI tract organs (for leaks or dysfunction), and any pathogens (parasites, yeast, fungi, dysbiotic bacteria) that may have entered.
Changing your diet, taking certain supplements, and addressing the stressors that created these issues in the first place is what you will focus on. But you shouldn’t do any of these steps alone, especially if you have AFS. Otherwise, you risk getting paradoxical reactions and adrenal crashes.
If you have questions about GI repair and adrenal fatigue recovery, you can contact the Dr. Lam Coaching team. We can offer you a free** no-obligation phone consultation at +1 (626) 571-1234 where we will privately discuss your symptoms and what your options are. You can also send us a question through our Ask The Doctor system by clicking here.
There are three areas to consider with GI repair, and each one builds on the one before. We’ll show you the lab markers for each area, as well as how to address any issues in that specific area. But if you have adrenal fatigue, then you’ll need to be cautious.