 Your immune system, your gastrointestinal (GI) tract, and your gut microbiome are the three components of your Inflammation circuit. They are the main modulators of your body’s inflammatory responses. These inflammation responses in the body can either be acute or chronic.
Your immune system, your gastrointestinal (GI) tract, and your gut microbiome are the three components of your Inflammation circuit. They are the main modulators of your body’s inflammatory responses. These inflammation responses in the body can either be acute or chronic.
Acute inflammation is a natural and necessary reaction to harmful stimuli, such as pathogen invasion or injury. Its role is to get rid of the original insult as well as any cells that were killed or damaged by it. And for cleaning out these damaged cells, it also needs an optimally functioning Detoxification Circuit.
Both the Inflammation and Detoxification circuits are part of the NeuroEndoMetabolic (NEM) Stress Response, which is your body’s global response to stress. Stress here would constitute the pathogen or injury that prompted the inflammatory response. The other four NEM circuits are the Hormone, Bioenergetics, Cardionomic, and Neuroaffect circuits. All six circuits work together in the fight against stress. Some are just more involved than others depending on the type of stressor your body is facing.
Your NEM’s main duty is to neutralize the stressor and then return your body to a state of homeostasis as quickly as possible. But, with chronic inflammation, that is a very difficult task. Chronic inflammation is becoming more and more common today, and, unfortunately, it underpins many chronic conditions. It also shaves years off your life.
How chronic inflammation happens has to do with the components of the Inflammation circuit – your immune system, GI tract, and the gut microbiome. And the good news is that these components can all be rebalanced with simple yet powerful steps, which we’ll cover in this article.
Your gut contains around two-thirds of your immune system cells, in what’s called the gut-associated lymphoid tissue. It also helps run your metabolism, produce vitamins, and store neurotransmitters. Its role in the functioning of your body is so central that it has its own nervous system - the enteric nervous system – which contains more neurons than your spinal cord.
Your gut microbiome is another miracle. It contains over 100 trillion microorganisms, which means that your body has 10 times more microbial cells than human cells and 100 times more microbial DNA than human DNA. In total, that’s around four pounds of organisms living inside your body. So it’s important that you are a good host and take care of their well-being and balance so they treat you well too.
Many people, however, neglect the health of their gut. They eat unhealthy diets, rely too much on certain medications (such as NSAIDs and antibiotics), drink too much alcohol, eat too much sugar, lead a sedentary lifestyle, get exposed to toxins, eat foods they’re sensitive to, let stress run their lives, and don’t get enough sleep.
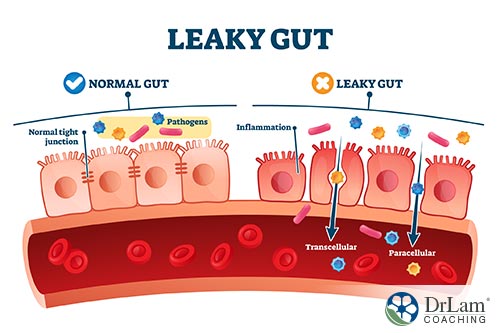
All of these factors, among others, can affect the balance of your gut microbiome. And when your gut microbiome is out of balance – a state called dysbiosis – your gut’s lining can begin to create leaks.
It’s important to note that genetics also play a role, although your diet and lifestyle choices can overrule genetic vulnerability to gut microbiome imbalance. Your choices do make a difference.
 If these factors above were just a one-off thing, you’d have no problem. But the more likely scenario is that you’re exposed to them consistently, possibly on a daily basis. If your diet is not healthy, and you eat it every day, then your gut has to deal with it on a daily basis. The same is true of stress or inadequate sleep.
If these factors above were just a one-off thing, you’d have no problem. But the more likely scenario is that you’re exposed to them consistently, possibly on a daily basis. If your diet is not healthy, and you eat it every day, then your gut has to deal with it on a daily basis. The same is true of stress or inadequate sleep.
As these things assault your gut microbiome, which then becomes imbalanced, it causes the tight junctions of your gut lining to become wider. These junctions are meant to only allow nutrients broken down from digestion to enter into your bloodstream. But now, they begin to allow other substances in, such as food particles, toxins, and pathogens.
Now, your immune system, which is so heavily present in your gut, is alerted of their presence and mounts an attack. That creates acute inflammation. But, because this keeps happening over and over again, the acute inflammation turns chronic.
Chronic inflammation that starts in the gut doesn’t stay in the gut. It can travel to other parts of your body and wreak havoc there. It can create neurological and psychiatric symptoms if it reaches the brain. Or it can create inflammatory conditions in the GI tract, such as IBD and IBS. It can also cause skin flare-ups and issues with your joints. Sometimes you can get very serious chronic conditions that take years off your life, such as:
So, if you want to live a longer, healthier, happier life, it pays to deal with any inflammation you have and to strengthen your gut microbiome. Let’s now take a closer look at some of the risk factors and how to address them.
Of course, when speaking of the gut and microbiome, diet is at least 50% of the equation. But, because we have discussed the topic of diet in-depth in other articles, such as this one, we’ll now focus on other risk factors.
There are many chemicals and toxins that can cause dysbiosis and impact the health of your gut, such as:
Let’s take glyphosate as an example. You can find traces of it in sugar, soy, corn, and wheat. It inhibits your cytochrome P450 enzymes, key players in detoxification. And when detoxification is slowed, inflammation rises. Glyphosate can also disrupt the synthesis of certain amino acids. This is why we advocate for eating organic whenever possible.
A huge swath of the population leads a sedentary lifestyle. Whether working in an office or remotely at home, too much time is spent sitting in front of a computer. But physical exercise is not just needed for weight loss and increased muscle mass. Its benefits stretch all the way to altering your gut microbiome. It helps diversify it. It also improves the function of your gut barrier and modulates its mucosal immunity.
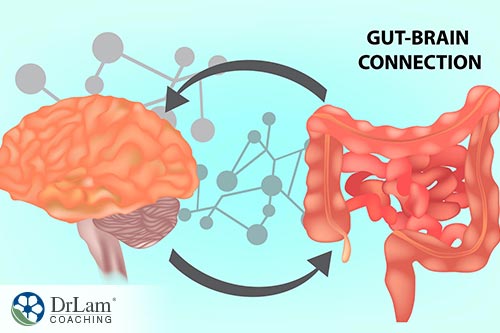 Physical stressors are not the only types of stressors that can affect gut health. Mental/emotional stress can be just as impactful. Indeed, this kind of stress elicits a similar stress response in the body, with the same kinds of stress hormones released to deal with it. Your NEM, of course, is the conduit of your stress response. And its first responder is cortisol.
Physical stressors are not the only types of stressors that can affect gut health. Mental/emotional stress can be just as impactful. Indeed, this kind of stress elicits a similar stress response in the body, with the same kinds of stress hormones released to deal with it. Your NEM, of course, is the conduit of your stress response. And its first responder is cortisol.
Cortisol is your body’s main anti-stress hormone, and it’s released by your adrenal glands. But, if the stress is constant, your adrenals will eventually dysregulate, leading to adrenal fatigue. Symptoms of Adrenal Fatigue Syndrome (AFS) include fatigue, weight gain, sleep issues, brain fog, anxiety, mild depression, PMS, infertility, hypoglycemia, heart palpitations, and lowered immunity, to name a few.
Cortisol affects every part of your body, including your GI tract and microbiome. And although it’s needed to neutralize stress, too much or too little of it negatively impacts your health. It can actually increase inflammation rather than help deal with it.
But the mind-gut connection utilizes other neural, endocrine, and immune pathways to communicate. And, in fact, how healthy your gut microbiome is may play a role in how well you respond to stress. So, in that sense, manipulating the microbiome may create changes in your emotional wellbeing and even in your social behavior.
This is why stress-management is just as important as physical health. You need to find ways to deal with the stresses in your life in a productive way. This can take the form of meditation, therapy, support groups, yoga, journaling, and taking time off.
One of the most overlooked yet effective and important stress reducers is having a good support network. It pays to cultivate meaningful relationships and healthy social bonds. This is why, for example, in all the blue zones (the areas around the world that have relatively higher longevity) you’ll find "community" as one of the top priorities of the citizens. This has also been validated by the Harvard Longevity Study.
Sleep is another overlooked factor when talking about gut health. But if you’re not sleeping enough or you're waking up constantly, you’ll likely have some level of inflammation. Sleep helps regulate your metabolism, burn fat, and keep your gut microbiome in balance.
Interestingly, both too short and too long sleep durations are harmful, and can increase the risk of cardiovascular problems as well as all-cause mortality. Seven hours of uninterrupted sleep is optimal for most people. Although, if you’re recovering from AFS or some other chronic condition, you may need to rest and sleep more than usual.
To increase your chances of getting the best sleep possible, there are a few sleep hygiene practices you should implement:
We’ve covered supplementation extensively in other articles, such as this one. But there are a few supplements worth discussing here in more detail.
There is some debate on the effectiveness of most commercial probiotic supplements. What we recommend is to look for targeted and spore-based probiotics. This means that your healthcare professional needs to assess your gut microbiome first and then select the right strains of bacteria needed for your gut, and they should be spore-based.
 Liposomal colostrum is one of those supplements that has so many actions and potential benefits yet are not very widely promoted. It contains more than 100 bioactive substances. They range from nutritional factors like vitamins, minerals, and energy, to immune factors like immunoglobulins, cytokines, and lysosomes, to growth factors like TGF-A, insulin-like growth factor, and fibroblasts.
Liposomal colostrum is one of those supplements that has so many actions and potential benefits yet are not very widely promoted. It contains more than 100 bioactive substances. They range from nutritional factors like vitamins, minerals, and energy, to immune factors like immunoglobulins, cytokines, and lysosomes, to growth factors like TGF-A, insulin-like growth factor, and fibroblasts.
There is a protein called lactoferrin that is found in both human and cow colostrum. It's one of the substances that can be a potential therapeutic agent for issues such as infections (viral, bacterial, and fungal), certain types of cancers, and endotoxin shock.
Some studies have shown that bovine colostrum can also help seal leaks in the gut of performance athletes, who are at higher risk of leaky gut. It's also been shown to help increase the good bacteria in the gut microbiome and reduce the risks that come with inflammation-associated conditions.
Glutamine is an amino acid that can help heal gut wall issues and even ulcers. More specifically, it can help support your gut's mucosal integrity and provide a source of energy for your healthy gut bacteria as well as your gut immune cells. It can also help address some of the symptoms that can come with digestive problems, such as brain fog and fatigue. In a more indirect fashion, its support of insulin secretion can help those with carbohydrate metabolism issues, which also involves the GI tract and digestion.
Beta-glucans are a type of sugar compound that you can get from oats and barley, although they can also be found in algae, bacteria, fungi, and yeast. They can provide your gut bacteria with soluble fiber, which can help reduce levels of cholesterol and glucose in the blood. This is really good for those with metabolic disturbances, diabetes, or cardiovascular issues.
Beta-glucans also have antioxidant effects, which can help reduce your risk for cancer, neurodegenerative disorders, and many other chronic conditions. Lastly, they have fermentation effects, which can help regulate the GI tract and microbiome, as well as the gut-associated immune tissues.
Certain types of mushrooms, especially those that originate in Asia, can help your microbiome regain or maintain its balance. For example, in the lab, reishi mushrooms have helped obese mice lose weight and become more insulin sensitive thanks to their gut bacteria alterations.
If you have issues with your immunity, which is common for those with gut wall problems, you can combine reishi mushrooms with cordyceps fungus or maitake mushrooms. Cordyceps also has the added benefit of supporting your vascular-system.
Finally, supplements that can help fill in any nutritional gaps left over by your diet or ones that can help give a boost to weakened systems can also indirectly help rebalance your GI tract and microbiome, as well as help strengthen your immune system. They are also a very important part of adrenal fatigue recovery, although you need to be extra careful with supplements if your AFS is more advanced.
The systems in your gut are interconnected, and understanding how can help you look at your health and longevity holistically. There are some key takeaways that you should focus on to help increase your longevity and improve your quality of life:

If you have questions about how to rebalance your gut microbiome, how to increase longevity, or how to recover from adrenal fatigue, you can contact the Dr. Lam Coaching team. We can offer you a free** no-obligation phone consultation at +1 (626) 571-1234 where we will privately discuss your symptoms and what your options are. You can also send us a question through our Ask The Doctor system by clicking here.
Your gut microbiome needs to have a good balance in order for it to be healthy and strong. More “good” bacteria and less “bad” bacteria are key. Sealing any leaks in the gut lining is also important so that you don’t allow chronic inflammation to begin or spread. Here’s how.
