
 Neurotransmitters (NTs) are chemicals in the brain that act as messengers, transmitting signals between the neurons, allowing communication to take place with the multitude of organ systems functioning within the body. These are potent neurochemicals that regulate nearly every function in the body including, physical and cognitive performance, weight, the perception and response to pain, sleep patterns and our emotional and mental state of being. A chemical imbalance in these will be felt everywhere in the body.
Neurotransmitters (NTs) are chemicals in the brain that act as messengers, transmitting signals between the neurons, allowing communication to take place with the multitude of organ systems functioning within the body. These are potent neurochemicals that regulate nearly every function in the body including, physical and cognitive performance, weight, the perception and response to pain, sleep patterns and our emotional and mental state of being. A chemical imbalance in these will be felt everywhere in the body.
Scientific research reveals that malfunctions in neurotransmission, such as a chemical imbalance, deficiency, or disruption is very common these days and are the root cause of many commonly found health conditions. When our neurotransmitters experience a chemical imbalance or are not working at optimum levels our mind and body cannot communicate clearly and effectively. It is estimated that about 80 percent of people have some form of chemical imbalance in their neurotransmitters. Fortunately, only a small number are clinically symptomatic and debilitating.
Brain function will be affected whenever there is a chemical imbalance or a dysfunction of poorly functioning NTs or malfunctioning hormonal axis that are the ultimate conduit upon which NTs exert their effect, such as the hormonal hypothalamic-pituitary-adrenal axis (HPA). This paper will examine both defects in a setting of Adrenal Fatigue Syndrome.
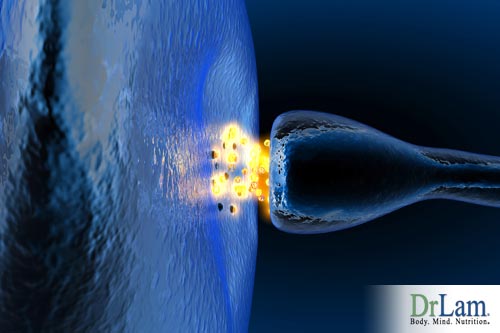
Before we can fully comprehend the effect neurotransmitter problems can have on us, we first need to understand how they communicate with each other. We can compare our nervous system to the electrical system in our homes. Nerve cells communicate with each other via tiny circuits called neuronal pathways. What’s different is that our nerve cells don’t touch each other, they come close but there is a gap between them called a synaptic cleft. The neuron sending the message is the presynaptic cell or axon, and the neuron receiving the message is the postsynaptic cell, or dendrite.
The direction of communication is one-way and to assist the message to make it across the synapse from the presynaptic cell to the postsynaptic cell, chemicals called neurotransmitters are used. For example, a typical synaptic transmission using the neurotransmitter serotonin would involve a presynaptic cell producing serotonin from tryptophan (an amino acid), accumulating the serotonin into small vesicles, which are in the terminals at the end. When your brain sends a signal (an action potential) it goes down the presynaptic cell and arrives at the end terminals. Upon arrival, serotonin is released and fills the synaptic cleft, crosses, and binds with its serotonin receptors located on the surface of the postsynaptic cell. When there is adequate serotonin binding to its receptors, a certain minimum threshold level is attained, and the signal (action potential) will arrive in the cell and continue to be propagated by moving on to the next cell. The goal is for the signal to reach its intended target, like skeletal muscle fibers in order to cause movement.
 To avoid having the nerve in a constant state of being on, the excess serotonin molecules in the synaptic cleft are eliminated by monoamine oxidase (MAO) enzymes plus a process called catechol-O-methyl transferase (COMT). Some of the remaining serotonin does return to the presynaptic cell in a process of absorption called reuptake. As the serotonin level reduces, the nerve signal is turned off and the system resets to baseline. The communication system is now ready to receive another signal or action potential. The classes of antidepressants that block the reuptake process, leading to increased serotonin, are called SSRIs or selective serotonin reuptake inhibitors. They include drugs called Lexapro, Prozac, Paxil, and Zoloft.
To avoid having the nerve in a constant state of being on, the excess serotonin molecules in the synaptic cleft are eliminated by monoamine oxidase (MAO) enzymes plus a process called catechol-O-methyl transferase (COMT). Some of the remaining serotonin does return to the presynaptic cell in a process of absorption called reuptake. As the serotonin level reduces, the nerve signal is turned off and the system resets to baseline. The communication system is now ready to receive another signal or action potential. The classes of antidepressants that block the reuptake process, leading to increased serotonin, are called SSRIs or selective serotonin reuptake inhibitors. They include drugs called Lexapro, Prozac, Paxil, and Zoloft.
The body’s main neurotransmitters are:
We now study each of these in more detail, starting with a group called catecholamines. Catecholamines are a grouping of NTs, which are very often referred to as the stress hormones. They are all derived from tyrosine, an amino acid. These neurotransmitters have the ability to act faster than cortisol, a hormone that responds to stress. The key catecholamines are dopamine, norepinephrine, and adrenaline.
Dopamine is a vital neurotransmitter as well as a precursor to norepinephrine. Dopamine released in the brain acts as a natural reward for pleasurable experiences like when having sex or dining on a delicious meal. It can also be released in response to neutral stimuli and as a result, pleasure becomes associated with those stimuli.
When dopamine is released in excess amounts in the brain, the effects can be anxiety, hyperactivity, and paranoia.
When dopamine levels are low, the effects can be addiction, cravings, compulsive behavior, depression, and inability to concentrate or focus.
Norepinephrine (NE) is an important neurotransmitter that helps to regulate attention and arousal, and plays a part in the fight-or-flight response. It acts both as a neurotransmitter and a hormone. In the brain, it functions as an excitatory NT, putting the body in a state of mental alert. It is produced and acts in the brain to prepare the individual to deal with a perceived threat. It also travels outside the brain. Once outside, it acts as a hormone and plays an important role in increasing heart rate and blood pressure, dilating eye pupils, dilating air passages in lungs, and narrowing blood vessels. It is the main controller that facilitates the actions required for day-to-day stress that we take for granted, such as standing up quickly without feeling dizzy from a reclining position.
If someone is living under ongoing stressful conditions, a long-term excess of norepinephrine in the brain can result. Such is the case of Adrenal Fatigue Syndrome, especially in the moderate to advanced stages. Chronic excess of norepinephrine is called sympathetic overtone. It can cause cellular and tissue inflammation, higher blood pressure, symptoms of hyperthyroidism, and panic attacks.
 On the other side of the spectrum, if there is a deficiency of norepinephrine over a long period it may cause behavioral problems, immunological chemical imbalance, impaired cognitive functioning, or secondary hypothyroidism.
On the other side of the spectrum, if there is a deficiency of norepinephrine over a long period it may cause behavioral problems, immunological chemical imbalance, impaired cognitive functioning, or secondary hypothyroidism.
Adrenaline (A), also called epinephrine, plays the key role in the urgent fight-or-flight reaction that takes place physiologically in the body in response to an immediate threat when survival is perceived to be at risk. It is the chemical daughter of norepinephrine. Their actions are similar, but adrenaline is much more potent. This hormone is secreted in the adrenal glands under the direction of the HPA axis and produces a rapid rise in blood pressure, rapid heartbeat, and stimulates the release of glucose in the liver. This is the hormone of last resort as far as the body is concern when it is under imminent danger. The more danger the body is perceived to be in, the more adrenaline will be released. Those who are in very advanced stages of AFS are invariably flooded with adrenaline internally. Symptoms include heart palpitations, dizziness on standing, and panic attacks.
Acetylcholine (ACh) is a major neurotransmitter for the parasympathetic nervous system (PNS) and helps the body carry out the day to day housekeeping functions for stimulation of rest-and-digest or feed-an-breed activities that occur when the body is at rest, especially after eating, including urination, sexual arousal, bowel movements, and digestion.
Serotonin is a monoamine neurotransmitter synthesized in specific neurons in the brain, central nervous system and in enterochromaffin cells located in the gastrointestinal tract. It is also called the feel good NT. Inside the brain, the pineal gland is the center for serotonin production. Throughout the entire central nervous system, serotonin has a vital role as an effective neurotransmitter in modulating a number of different areas:
Serotonin is also a precursor to melatonin. Once they have completed their task a reuptake or reabsorption of the hormone takes place. Serotonin is effective in making us feel calm and basically good naturally. It helps the mind to relax so that we can easily fall asleep and stay soundly asleep.
Serotonin and melatonin are produced in the body from tryptophan, an amino acid. As we have already discussed, a person who doesn’t have any serotonin cannot produce abundant amounts of melatonin. The ability to convert from one type to another depends on a variety of nutritional cofactors and coenzymes.
For a person to feel well, the overall serotonin level cannot be too high or too low. There should be no chemical imbalance. Chronic excess of serotonin over a long period of time may result in:
A long-term depletion or deficiency in serotonin can cause:
 The compounds utilized in the manufacturing of neurotransmitters are called precursors. Anything affecting the precursors will in turn affect the resulting NTs and influence how the nervous system functions in the end. If a precursor has a deficiency in a certain aspect, then that can cause a bottleneck or delay in the creation of a particular NT and affect its ultimate functionality. It is also true that if there is an excess of a certain precursor that can cause the resulting NT to have excessively high levels.
The compounds utilized in the manufacturing of neurotransmitters are called precursors. Anything affecting the precursors will in turn affect the resulting NTs and influence how the nervous system functions in the end. If a precursor has a deficiency in a certain aspect, then that can cause a bottleneck or delay in the creation of a particular NT and affect its ultimate functionality. It is also true that if there is an excess of a certain precursor that can cause the resulting NT to have excessively high levels.
There are a number of different neuroactive substances working to promote the proper functioning of the neurotransmitter. The following are some and their contributions:
Neurotransmitter precursors and modulators serve important functions. They are generally less potent and thus available as over the counter nutritional supplements. Their gentle character lends well when used in cases where medications such as NT repletion tools are not indicated or well tolerated, for example. They are also less addictive because they tend to be weaker in action.
NTs generally fall into two groups when classified by their actions:
For the body to be in optimum health, NTs of opposing actions need to be perfectly balanced.
L-Glutamate (glutamic acid) is the most vital excitatory neurotransmitter functioning in the brain. It performs a significant role in brain chemistry. It is released by a variety of neurons and acts to stimulate other neurons during synapses. The more glutamate, the higher the levels of excitation will be.  If the excitatory neurotransmitters reach excessively high levels, a state of excitotoxicity exists. This is when the neuronal activation has reached such a high level that the stimulated firing of neurons has become neurologically damaging. Many of the illicit or prescription drugs that abusers take affect either one or both neurotransmitters and cause stimulating or tranquilizing effects on the brain.
If the excitatory neurotransmitters reach excessively high levels, a state of excitotoxicity exists. This is when the neuronal activation has reached such a high level that the stimulated firing of neurons has become neurologically damaging. Many of the illicit or prescription drugs that abusers take affect either one or both neurotransmitters and cause stimulating or tranquilizing effects on the brain.
On the other end of the spectrum, molecules such as GABA and taurine are part of the inhibitory NTs. GABA is derived from glutamine and synthesized when the active form of vitamin B6 (P5P) is present. Inhibitory NTs inhibit or prevent the firing of neurons. It plays a critical role in the regulation of neuronal excitability throughout the entire nervous system so that the body does not operate in a continuous state of high or excitment. They reduce anxiety and promote calmness.
 Have you ever wondered about neurotransmitters and how the are affecting your life? We don't learn much about neurotransmitters growing up, however, they play a prominent role in nearly everything that we do? It is important to know the facts about neurotransmitters and the manifestation of an imbalance. There may be over sixty different mental and physical illnesses associated with a deficiency in neurotransmitters, including:
Have you ever wondered about neurotransmitters and how the are affecting your life? We don't learn much about neurotransmitters growing up, however, they play a prominent role in nearly everything that we do? It is important to know the facts about neurotransmitters and the manifestation of an imbalance. There may be over sixty different mental and physical illnesses associated with a deficiency in neurotransmitters, including:
In particular, neuroscience research has proven strong association between low levels of serotonin and/or norepinephrine with the following conditions:
Keep reading below to learn more about neurotransmitters and how they may impact your life negatively and positively as well as what you can do to better manage their effects.
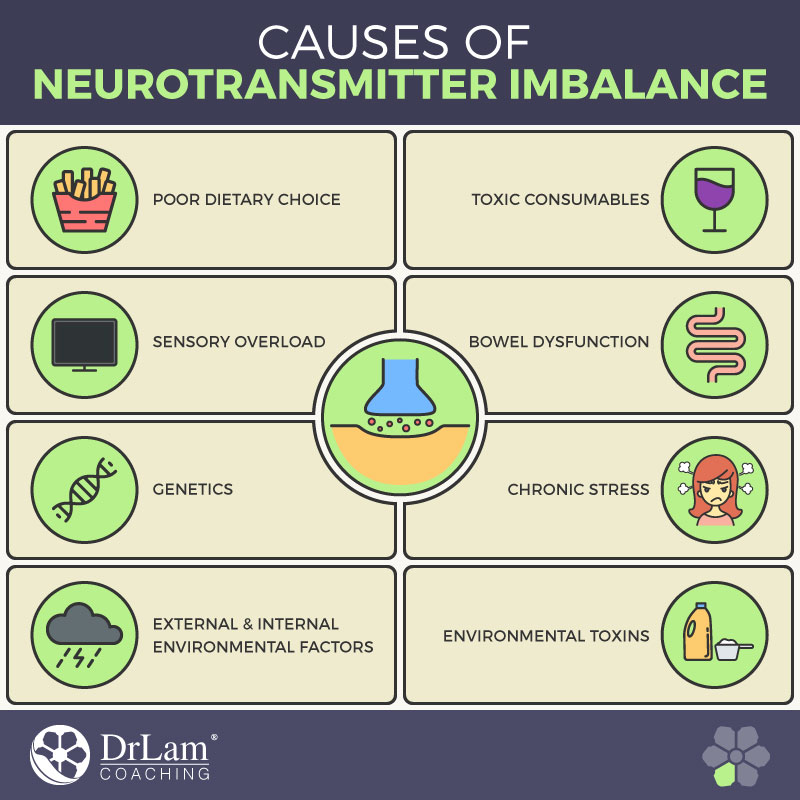
When learning about neurotransmitters one must evaluate the components having an impact on them. There are a number of different reasons why people have imbalanced levels of NTs in their system:
 Environmental Toxins. Most everyone is exposed to toxins in the environment and even inside our homes, every single day. We use cleaning products, laundry soap and fabric softeners, air fresheners, perfume and cologne, nail polish, and other personal care products. We are exposed to pesticides and herbicides in our garden and construction products if our home is undergoing a remodel. Our indoor and outdoor carpeting contains chemicals and so does our clothing. All of these things contain toxic chemicals that can seriously affect our neurotransmitters. These toxins can directly affect the receptors and even inhibit our natural production.
Environmental Toxins. Most everyone is exposed to toxins in the environment and even inside our homes, every single day. We use cleaning products, laundry soap and fabric softeners, air fresheners, perfume and cologne, nail polish, and other personal care products. We are exposed to pesticides and herbicides in our garden and construction products if our home is undergoing a remodel. Our indoor and outdoor carpeting contains chemicals and so does our clothing. All of these things contain toxic chemicals that can seriously affect our neurotransmitters. These toxins can directly affect the receptors and even inhibit our natural production.Considering all of the above, you may be wondering what you can do about neurotransmitters inside of your body and how to not only determinine their imbalance but manage them in an effort to help create a healthier version of yourself.
Urine neurotransmitter testing serves as a versatile diagnostic tool in achieving neurotransmitter balance by assessing levels of several neurotransmitters or their metabolites. These include serotonin, crucial for mood regulation; gamma-aminobutyric acid (GABA), vital for controlling brain activity; glutamate, the primary excitatory neurotransmitter; dopamine, linked with pleasure and reward; norepinephrine and epinephrine, essential for the body’s stress response; and phenylethylamine (PEA), a mood-elevating stimulant. Evaluating these neurotransmitters, the test can offer valuable insights into an individual’s neurochemical balance, identifying potential imbalances or dysregulations that may contribute to various health issues. This highlights the importance of urine neurotransmitter testing in crafting personalized and targeted therapeutic interventions for achieving neurotransmitter balance.
As a valuable tool for assessing neurotransmitter balance, urine neurotransmitter testing explores various aspects of an individual's health, especially focusing on the autonomic nervous system, adrenal health, and gut health. The autonomic nervous system, pivotal in regulating involuntary body functions like heart rate and digestion, can be significantly influenced by neurotransmitter imbalances. This test, by analyzing neurotransmitter levels in urine, pinpoints such imbalances, providing insights into potential nervous system dysfunctions. Furthermore, neurotransmitter levels mirror adrenal health, affecting stress response and energy levels. The test is also insightful for gut health, considering the significant neurotransmitter production in the gastrointestinal tract, identifying imbalances indicative of gut dysbiosis or other issues. Hence, urine neurotransmitter testing emerges as a comprehensive tool for understanding intricate bodily systems and functions, paving the way for targeted interventions to achieve optimal neurotransmitter balance and overall health.
 NT deficiencies can be replenished with amino acids, dietary, and lifestyle changes. NT excess can be helped by lifestyle modifications as well as compounds that calm NT release. It all comes down to balancing so that the excitatory NTs are in balance with the inhibitory NTs. Bias in any direction is not desirable. Most NT imbalances reflect underlying pathology. Comprehensive strategies of NT rebalance needs to also correct the underlying root cause.
NT deficiencies can be replenished with amino acids, dietary, and lifestyle changes. NT excess can be helped by lifestyle modifications as well as compounds that calm NT release. It all comes down to balancing so that the excitatory NTs are in balance with the inhibitory NTs. Bias in any direction is not desirable. Most NT imbalances reflect underlying pathology. Comprehensive strategies of NT rebalance needs to also correct the underlying root cause.
To correct specific NT imbalances, what is needed is to first identify the defective pathway. Clinicians experienced in NT physiology find that a detailed history usually provides the best information to commence NT repletion when needed. Expansive testing may not be needed provided the patient is closely tracked and monitored by an experienced clinician. NT imbalance usually presents in a set of clinical behaviors with general recognizable patterns. Experienced clinicians will be able to ascertain this.
Clinical rebalancing trials can commence by stimulating one or more of the specific conversion pathways that may not be working properly or if sufficiently based on history and then observe the results. The key is to first be able to recognize the symptoms pattern when presented. For example:
To replete what is deficient, nutritional supplements such as amino acids, vitamins and minerals are used to form a nutritional cocktail that can be taken orally. Adaptogenic herbs such as maca, rhodiola, and ashwagandha as well as glandulars can play a supporting role when indicated. Other supportive modalities or therapies include electromagnetic therapies that work on the body's qi (energy) as well as brain wave entrainment technologies, bio-feedback, mitochondrial fortification, liver decongestion, extracellular matrix cleanse, and various detoxification techniques designed to enhance the body’s self-healing ability and rebalance power when these are deployed properly. Along with nutritional repletion, here are eight lifestyle changes that can help NT imbalance.
So, now that you have more information, what will you do about neurotransmitters and their effect on your health today?
 Most popular antidepressants are classified as SSRIs, which refers to the selective serotonin re-uptake inhibitors mentioned earlier. SSRIs cause short-term flooding in the brain of serotonin, and along with this, there is a quick degrading process of serotonin while it remains in the synaptic cleft. The result is that more and more serotonin is eventually needed since the receptors for serotonin become desensitized to the constant fluctuation of neurotransmitters, however the body is producing less and less serotonin naturally since it has started to depend on the medication which provides an external source of serotonin. When the brain does release naturally produced serotonin, it gets degraded way too quickly since the enzymes left in the synaptic cleft are now trained to quickly break down any serotonin. This may lead to a chemical imbalance.
Most popular antidepressants are classified as SSRIs, which refers to the selective serotonin re-uptake inhibitors mentioned earlier. SSRIs cause short-term flooding in the brain of serotonin, and along with this, there is a quick degrading process of serotonin while it remains in the synaptic cleft. The result is that more and more serotonin is eventually needed since the receptors for serotonin become desensitized to the constant fluctuation of neurotransmitters, however the body is producing less and less serotonin naturally since it has started to depend on the medication which provides an external source of serotonin. When the brain does release naturally produced serotonin, it gets degraded way too quickly since the enzymes left in the synaptic cleft are now trained to quickly break down any serotonin. This may lead to a chemical imbalance.
Many taking antidepressants will need constant dosage increases. In doing so, the body is depleting a fair amount of the receptors in the brain for serotonin. Furthermore, the receptors for serotonin in your colon, kidneys and liver can be damaged. This can affect the sensitive balance between your gut and your brain, which regulates appetite, creating a vicious cycle.
Those who are already on SSRIs should not stop abruptly as that can cause unpleasant withdrawal symptoms.
It has been shown that small amounts of caffeine can enhance mental performance and guard against the onset of Alzheimer’s so it need not be avoided entirely except for people who are at risk for or suffering from Adrenal Fatigue Syndrome. Caffeine can affect the brain in a similar manner as antidepressants or other central nervous system stimulants such as ephedra or ephedrine. They can overwhelm the brain with excitation which can create a resistance and/or long term damage to neurotransmitter receptors. Chronic use of caffeine may lead to a chemical imbalance.
If you really must drink coffee, you should limit yourself to just one eight to ten ounce cup of black coffee a day. One week every two months you should switch to decaf coffee. People who rely on coffee, tea, energy drinks or even soda change their brain chemistry and certain physical characteristics over time. Coffee is water and fat-soluble and easily crosses the blood-brain barrier, so as you drink more and more coffee, the caffeine causes your brain cells to produce more neurotransmitter receptors for adenosine. What adenosine does is bring about a feeling of being tired. The structure of caffeine resembles that of adenosine very closely, which means that caffeine can readily fit into the receptors in your brain cells for adenosine. With caffeine always plugging the receptors for adenosine, then adenosine can’t bind to its own receptors any longer and bring about the feeling of tiredness. The problem is that the body will respond by creating more adenosine receptors which means you will need to increase your intake of caffeine in order to not feel tired, which causes you to build a tolerance over time.
You can avoid this and kick your caffeine habit by hitting your reset button regarding your adenosine receptors. You only need to survive seven to twelve days without caffeine and this is why the recommendation is to take a break from coffee and other stimulants for a week every few months.
Other metabolically stimulating compounds including but not limited to thyroid replacement hormones, DHEA, pregnenolone, testosterone, pituitary glandular, adrenal cortex, green tea, maca, rhodiola, ginseng, zinc, copper, selenium, iodine, kelp, should be carefully scrutinized for their need.
 The building blocks of many neurotransmitters are amino acids, vitamin Bs, and various minerals. If you are deficient in any of these critical components, you can be left without the building blocks you need for healthy and balanced neurotransmitters.
The building blocks of many neurotransmitters are amino acids, vitamin Bs, and various minerals. If you are deficient in any of these critical components, you can be left without the building blocks you need for healthy and balanced neurotransmitters.
Some of the best sources of high quality amino acids are almonds and almond butter, free-range eggs, grass-fed beef, quinoa, raw organic dairy products, spirulina or sources of chlorella, and wild salmon. Healthy people with problems sleeping or with motivation that are linked to issues having to do with their neurotransmitters can often, but not always, benefit from using essential amino acids.
For the nervous system to function properly to synthesize and circulate the neurotransmitters being produced by the precursors to amino acids, you should be taking in adequate amounts of B complex vitamins, vitamin B6, B12, and folate from food sources. These are extremely important in the metabolic processes in nerves. Good sources of vitamin B6 can be found in bell peppers, spinach, and turnip greens. Good sources of folate can be found in asparagus, beets, broccoli, calf’s liver, lentils, mustard greens, parsley, romaine lettuce, and spinach. Good sources of vitamin B12 are found in calf’s liver and snapper. External supplementation is acceptable for those who are healthy if you are concerned about whether you have enough. Because of their excitatory nature, those who are weak or sensitive need to be very careful not to take too much.

Environmental toxins can detrimentally affect the production of NTs and cause you to be overly sensitive to NTs, which can lead to brain fog, fuzzy thinking and brain damage. These toxins can be found in the mycotoxins existing in moldy coffee, fragrances in perfumes and colognes, and/or the air freshener you spray around your home or have hanging in your car. In addition to damaging NTs, toxins also place excessive stress on the liver, causing congestion. The extracellular matrix becomes polluted as well. Both are not conducive to optimal health.
To avoid toxins here are a few tips:
Because our body has an intrinsic system of toxin removal, you will start to feel better gradually as you take the steps to avoid further insult. Unfortunately, once you adapt to these changes you’ll find that you will be very sensitive when you find your neurotransmitters being under attack, like when strolling through the perfume section of a department store. You will notice the effect it has on you immediately. Avoiding toxins should therefore be a lifelong endeavor.
In the 21st century we are constantly bombarded by rapid visual images, sounds, auditory input from television, computer games, movies, and electronic monitors that flicker so fast the eyes can hardly detect what’s in front of them. There are radio and EMF waves, LED and fluorescent lighting, and a hectic lifestyle to contend with. All of this stimulation requires a brain to modulate the constant sensory bombardment at a level that would have never been imagined by our ancestors.
The brain must find a way to calm itself down and only use its delicate supply of serotonin and GABA, the calming, inhibitory neurotransmitters. All of this overstimulation impacts neurotransmitters and their receptors significantly so think about the following activities you may be doing:
 Your gut is only second to your brain in influencing bodily functions. Your gut actively uses over thirty different neurotransmitters as it contains your enteric nervous system. The truth is that 95 percent of your body’s supply of serotonin exists in your gut. Consider that in the distance from your esophagus to your anus there are approximately one hundred million neurons. This is more than in your spinal cord or your peripheral nervous system.
Your gut is only second to your brain in influencing bodily functions. Your gut actively uses over thirty different neurotransmitters as it contains your enteric nervous system. The truth is that 95 percent of your body’s supply of serotonin exists in your gut. Consider that in the distance from your esophagus to your anus there are approximately one hundred million neurons. This is more than in your spinal cord or your peripheral nervous system.
The lining of your gut produces neurotransmitters and the bacteria in your gut, numbering in the billions, are also creating neurotransmitters. What this means is that if the lining of your gut is damaged in any way, or the flora is not in balance, then you are certainly at risk for a chemical imbalance in your neurotransmitters or even at risk for deficiencies. The reason why so many people suffer from irritable bowel syndrome at one time or another is too much serotonin in their gut, which means they have a chemical imbalance of the neurotransmitters there. This explains why taking antidepressants can cause such serious gut problems. Maintaining healthy flora with probiotics is therefore an important part of a comprehensive NT balancing program as long as it does not trigger constipation.
Your NTs are only as good as their ability to help in the transmission of signals. This is largely the function of the myelin sheath. Myelin sheaths wrap around your nerves, and in order to have a healthy nervous system you should take in certain nutrients that help support the production of these protective myelin sheaths, and also support your nervous system in general.
A good quantity of omega-3 fatty acids, specifically docosahexaenoic acid (DHA) can be helpful. DHA is extremely important in forming the structure of myelin sheaths and in the prevention of the breakdown and degradation of nerve cells. Excellent sources of omega-3 fatty acids can be found in flax seeds, kale, collard greens, walnuts, and winter squash. However, the quantity of DHA that the body absorbs from plants, nuts and seeds is really quite low.
There are better sources of omega-3 fatty acids and DHA that are more readily available, which include cloves, cod, halibut, grass-fed beef, salmon, shrimp, sardines, and tuna. For vegetarians or vegans algae-based DHA supplements are recommended, such as the ones from marine phytoplankton. Other sources of food that support the formation and health of neuronal membranes and myelin sheaths because of the high concentration of oleic acids include almonds, avocados, macadamia nuts, olive oil and pecans.
 Mindfulness is the act of being more aware and conscious of the present moment, non-judgmentally. Or, in other words, making a conscious choice to be aware and experience the present moment to the fullest without judgment, in all your activities, without dwelling in the past or the future. The frequent use of mindfulness is one of the most effective ways for stress reduction, managing chronic pain, alleviating depression and anxiety, easing a chemical imbalance due to chronic stress, coping with life, overcoming addictions, and to top it off, it is a great avenue for spiritual development, self-actualization, and creativity.
Mindfulness is the act of being more aware and conscious of the present moment, non-judgmentally. Or, in other words, making a conscious choice to be aware and experience the present moment to the fullest without judgment, in all your activities, without dwelling in the past or the future. The frequent use of mindfulness is one of the most effective ways for stress reduction, managing chronic pain, alleviating depression and anxiety, easing a chemical imbalance due to chronic stress, coping with life, overcoming addictions, and to top it off, it is a great avenue for spiritual development, self-actualization, and creativity.
Mindfulness helps boost and balance our feel good neurotransmitters like dopamine, serotonin and endorphins and at the same time reduces excessive norepinephrine, the neurotransmitter responsible for chronic stress. Mindfulness and mindfulness based techniques, such as Yoga and Tai Chi, help the Nervous System rejuvenate and may aid in recovery from a chemical imbalance.
The Adrenal Breathing Exercise is an excellent clinically proven tool that brings mindfulness to calm the overactive autonomic nervous system when under stress. NTs responsible for breathing rhythm include GABA, glutamine, and glycine. Proper breathing not only re-balances NTs (healing chemical imbalance), but also prevents over excitation of the sympathetic nervous system that leads to excess release of norepinephrine and adrenaline. Adrenal Breathing Exercise is specific in accomplishing both and is invaluable. It should be an integral part of the NT balancing program and its power should not be underestimated.
Research has shown that practicing yoga may elevate brain GABA levels, the brain's primary inhibitory neurotransmitter. This suggests that the practice of yoga be explored as a possible treatment for depression and anxiety disorders associated with low GABA levels. Yoga has shown promise in improving symptoms associated with depression, anxiety, chemical imbalance, and epilepsy. The Adrenal Yoga Exercise series is designed specifically to calm the autonomic nervous system and re-balance neurotransmitters without excitation of the sympathetic nervous system.
 The two main classes of NT repletion medications designed to overcome depression and anxieties are SSRIs and SNRIs, each having their own antidepressants side effects. SSRIs include drugs such as Citalopram (Celexa), Escitalopram (Lexapro), Fluoxetine (Prozac), Paroxetine (Paxil and Pexeva), and Sertraline (Zoloft). SNRIs include desvenlafaxine (Pristiq), duloxetine (Cymbalta), and venlafaxine (Effexor and Effexor XR).
The two main classes of NT repletion medications designed to overcome depression and anxieties are SSRIs and SNRIs, each having their own antidepressants side effects. SSRIs include drugs such as Citalopram (Celexa), Escitalopram (Lexapro), Fluoxetine (Prozac), Paroxetine (Paxil and Pexeva), and Sertraline (Zoloft). SNRIs include desvenlafaxine (Pristiq), duloxetine (Cymbalta), and venlafaxine (Effexor and Effexor XR).
SSRIs work by inhibiting the reabsorption of serotonin. By causing the body to feel good, they ease symptoms of moderate to severe depression and anxiety disorders common in Adrenal Fatigue. SNRIs work by inhibiting the reabsorption of not one but two important brain chemicals: serotonin and norepinephrine, which is why these drugs are sometimes called dual reuptake inhibitors, or dual-acting antidepressants, and tend to be a bit stronger. Because SNRIs affect two neurotransmitters, they may be an effective form of treatment for those who have failed to respond to single-acting antidepressants, such as SSRIs. Some research suggests that patients with severe depression may respond better to an SNRI.
Possible side effects for both SSRIs and SNRIs include nausea, muscle weakness, tremor, heart palpitation, increased blood pressure and heart rate, headache, dry mouth, fatigue, excessive sweating, constipation, and fluid retention. Women who are nursing or pregnant should avoid taking SNRIs, as they are passed into breast milk. Certain SSRIs may be better options for pregnant or nursing mothers. People with liver problems or high blood pressure will need liver function monitoring periodically via blood tests. Those on aspirin, non-steroidal anti-inflammatory drugs (NSAIDs) such as ibuprofen, and blood-thinning medications such as warfarin (Coumadin) should use SNRIs with caution as SNRIs may inhibit blood clotting, thus increasing the risk of severe bleeding from a cut or scrape.
 One of the major problems associated with both SSRIs and SNRIs over time is dependency as well as worsening NT depletion, the very problem it is supposed to solve. More and more medication is required with greater and greater depletion leading to a vicious cycle of progressively more medication needed with less and less effect. Typically, there is a short honeymoon with lesser depression within a few weeks. Six to nine months later, however, the crude awakening begins. The patient literally wakes up to returned depression. The patient tries to quit the SSRI, such as Zoloft and finds that they feel worse than ever. The SSRI never solved the underlying problem of NT deficiency but simply temporarily increased the level of NT by blocking its metabolism at the synapses. As more SSRI comes on board with daily intake, the MAO system increases the breakdown of serotonin with no additional nutritional intake of serotonin precursors for replenishment. The overall intersynaptic levels of NT gradually decline, when they fall below the threshold needed to keep the patient disease-free, the depression returns with vengeance.
One of the major problems associated with both SSRIs and SNRIs over time is dependency as well as worsening NT depletion, the very problem it is supposed to solve. More and more medication is required with greater and greater depletion leading to a vicious cycle of progressively more medication needed with less and less effect. Typically, there is a short honeymoon with lesser depression within a few weeks. Six to nine months later, however, the crude awakening begins. The patient literally wakes up to returned depression. The patient tries to quit the SSRI, such as Zoloft and finds that they feel worse than ever. The SSRI never solved the underlying problem of NT deficiency but simply temporarily increased the level of NT by blocking its metabolism at the synapses. As more SSRI comes on board with daily intake, the MAO system increases the breakdown of serotonin with no additional nutritional intake of serotonin precursors for replenishment. The overall intersynaptic levels of NT gradually decline, when they fall below the threshold needed to keep the patient disease-free, the depression returns with vengeance.
This problem can be resolved with prescribing the proper amino acids and nutrients—the building blocks of NTs, and the benefits of the medications will resume within one to two weeks. Sad to say this is seldom the path taken by conventional medicine. Instead, a larger dose or more potent medication is prescribed, again masking the underlying root problem of NT depletion. Over time, sufferers become over medicated and sedated, but depression continues.
 Those who are currently on SSRIs and SNRIs should not abruptly stop their treatment to avoid withdrawal symptoms and antidepressants side effects that can be very hard to bear. Take a step back and look at the big picture. A comprehensive plan is needed to replenish deficiency and rebalance NTs to prevent depression from worsening and other antidepressants side effects. Underlying chronic problems commonly associated with NT imbalance, such as chronic fatigue, infection, or Adrenal Fatigue Syndrome, should be addressed so the root cause is dealt with properly. Natural compounds can be administered but titrated to match the body’s state of function each step along the way. Medications can be tapered off slowly as the body returns to optimal function and root problems resolve. Timing is key, and premature cessation can bring on withdrawal and other negative side effects. Remember that an NT imbalance is more often than not secondary to some other underlying disease, which is why most NT self-corrects once the underlying condition is resolved.
Those who are currently on SSRIs and SNRIs should not abruptly stop their treatment to avoid withdrawal symptoms and antidepressants side effects that can be very hard to bear. Take a step back and look at the big picture. A comprehensive plan is needed to replenish deficiency and rebalance NTs to prevent depression from worsening and other antidepressants side effects. Underlying chronic problems commonly associated with NT imbalance, such as chronic fatigue, infection, or Adrenal Fatigue Syndrome, should be addressed so the root cause is dealt with properly. Natural compounds can be administered but titrated to match the body’s state of function each step along the way. Medications can be tapered off slowly as the body returns to optimal function and root problems resolve. Timing is key, and premature cessation can bring on withdrawal and other negative side effects. Remember that an NT imbalance is more often than not secondary to some other underlying disease, which is why most NT self-corrects once the underlying condition is resolved.
 NT repletion can be satisfied with the use of natural compounds and brain boosting supplements for those low on specific NTs. This can be accomplished by way of nutritional brain boosting supplements, in particular amino acids, that are the foundation precursor or modulators of NTs. Athletes wishing peak performance heading into an intense workout or competition requiring extreme focus sometimes take five to ten grams of amino acid powder to fortify themselves for that reason. Amino acid supplementation, however, can cause over-stimulation and trigger crashes if the body is weak. They can lead to insomnia and panic attacks. Amino acid brain boosting supplements are the most commonly deployed to accomplish this goal. Brain boosting supplements include 5-HTP, DLPA, DPA, GABA, glutamine, L-theanine, tryptophan, or tyrosine.
NT repletion can be satisfied with the use of natural compounds and brain boosting supplements for those low on specific NTs. This can be accomplished by way of nutritional brain boosting supplements, in particular amino acids, that are the foundation precursor or modulators of NTs. Athletes wishing peak performance heading into an intense workout or competition requiring extreme focus sometimes take five to ten grams of amino acid powder to fortify themselves for that reason. Amino acid supplementation, however, can cause over-stimulation and trigger crashes if the body is weak. They can lead to insomnia and panic attacks. Amino acid brain boosting supplements are the most commonly deployed to accomplish this goal. Brain boosting supplements include 5-HTP, DLPA, DPA, GABA, glutamine, L-theanine, tryptophan, or tyrosine.
There are many ways to replete brain boosting supplements, as the following examples will show:
Amino acid repletion is usually taken in conjunction with a variety of other vitamins and minerals and brain boosting supplements because they work together and need one another to support good brain function. For example, pyridoxal-5-phosphate is needed for the conversion of tryptophan to serotonin.
Repletion therapy must be carried out carefully and no one should take matters into their own hands without the proper guidance. Most failures occur under inexperienced hands. For example, if you take 5-HTP and no other supplement(s), or if you take improperly balanced 5-HTP, you can easily deplete the dopamine in your system. If you take L-DOPA alone, or improperly balanced L-DOPA, you can easily deplete the serotonin in your system, as well as the L-tryptophan, sulfur-based amino acids, and tyrosine. One must always be aware of the balances of brain boosting supplements and always seek advice from one's primary medical physician.
 1. B Vitamins. For those that need assistance in the methylation processes of melatonin and of the catecholamines, the amino acid S-Adenosyl methionine (SAMe) can help or you can try methionine and vitamin B12. An active form of vitamin B12 can be found in Methyl-B12, so that could be useful as well.
1. B Vitamins. For those that need assistance in the methylation processes of melatonin and of the catecholamines, the amino acid S-Adenosyl methionine (SAMe) can help or you can try methionine and vitamin B12. An active form of vitamin B12 can be found in Methyl-B12, so that could be useful as well.
Active forms of B vitamins are more potent since they are more useable than non-active forms and can be part of the brain boosting supplements family. The active forms don’t need to be converted into the form that the body actually uses. They can be utilized by the body as they are, or with fewer steps. This is a benefit for those who are strong and healthy. They may be too excitatory for those with weak adrenals. B vitamins therefore have to be carefully chosen to match the body’s need to be successful.
NT repletion supplements can be found in the following B vitamins:
Active vitamin B6 —pyridoxal-5’-phosphate (P5P)
Active vitamin B9 —5-methyltetrahydrofolate (5-MTHF)
Active vitamin B2 —flavin mononucleotide (FMN)
Active vitamin B3 —nicotinamide adenine dinucleotide (NAD or NADH)
Active vitamin B5 —pantothenic acid or pantethine
Alert: Too much vitamin B can cause crashes. Those who are weak and sensitive have to be extra careful. Side effects include anxiety, heart palpitations, and insomnia.
2. 5-HTP. Because serotonin does not cross the blood-brain barrier, it cannot pass into its specified pathways in the central nervous system when taken orally. However, the amino acid tryptophan, along with its metabolite 5-HTP or 5-hydroxytryptophan, which serotonin is derived from, does have the ability to cross the blood-brain barrier.
It is not usually advised that tryptophan be taken as a supplement, but 5-HTP is recommended widely as an effective serotonergic agent and is safe for the most part when taken in small doses. It is helpful to take 5-HTP before bedtime in order to help you relax before going to sleep. It can give you enough serotonin so that the melatonin you need can be produced. For some, it is also helpful to take small doses of 5-HTP throughout the day to help in the production of serotonin and to keep you relaxed.
Recommended dosage: When starting out with 5-HTP it is very important to begin with a very low dose and gradually work your way up. The dosage between individuals can vary from 50 to 200 mg per dose, depending on the person’s needs and what they can safely tolerate.
Alert: High dosages of 5-HTP (e.g., 200 mg or higher) may also cause nausea and stomach cramps. This is why some prefer to take slow release 5-HTP brain boosting supplements at bedtime. These symptoms may only occur at certain points in the day, e.g., at bedtime and not during the day, during the night or in the early hours of the morning if more is taken then. When taken in extremely high doses 5-HTP can cause serotonin toxicity or serotonin syndrome, and this can literally be fatal.
3. Melatonin. Melatonin is a hormone made from serotonin yet 5-HTP is a precursor to serotonin and thus can increase melatonin levels. In order to produce melatonin and the required coenzymes and co-factors, the body requires a certain amount of serotonin as a primer. A certain level of serotonin in the body is needed by many for them to relax enough to go to sleep and when melatonin is produced internally after sleep has initiated, it helps you to stay asleep. A deficient production of melatonin can result in anxiety and mood disorders, lowered basal body temperature, insomnia, elevated estrogen/progesterone ratio, and immune suppression associated with cancer. Excess melatonin is associated with seasonal affective disorder (SAD), lowered estrogen/progesterone ratio, low thyroid and adrenal function, and hypotension.
 Melatonin is widely used as a sleep aid. The sleep promoting effects of melatonin are most apparent only if a person's melatonin levels are low. In other words, taking melatonin is not like taking a sleeping pill or even 5-HTP. It will only produce a sedative effect when melatonin levels are low. By enhancing sleep quality, melatonin enhances NT stability and balance.
Melatonin is widely used as a sleep aid. The sleep promoting effects of melatonin are most apparent only if a person's melatonin levels are low. In other words, taking melatonin is not like taking a sleeping pill or even 5-HTP. It will only produce a sedative effect when melatonin levels are low. By enhancing sleep quality, melatonin enhances NT stability and balance.
Alert: When taking melatonin, you have to be very careful regarding the dosage. Some people are able to absorb and assimilate melatonin quite easily and thus only need a fraction of a milligram. Other people need as much as 50 mg to get the desired effect. In other words, the effect is not linear in response. Some trial and error is required in the hands of an experienced clinician. Those who experience a hangover in the morning with melatonin should take it two hours before sleep rather than at bedtime.
4. GABA, Glutamate, Glutamine. The neurotransmitters in the brain doing most of the work are glutamate (also called glutamic acid) and GABA. Over 50 percent of the synapses in the brain release glutamate, while 30 percent to 40 percent release GABA. GABA is an inhibitor and thus calming. Glutamate is excitatory and stimulatory. In healthy individuals, GABA and glutamate will be in balance in the brain with regard to their absolute concentrations and their relative ratios. Problems arise if the ratio is imbalanced. For example, if GABA production is reduced, a higher glutamate to GABA ratio in the brain will increase, leading to a sense of being wired. A GABA deficiency over a long period of time is linked to the following excitatory or stimulatory effects:
If GABA is deficient in the body it can be supplemented by using a supplemental form of GABA. Each of us may have different amounts of GABA in the brain that is considered normal. There are no accepted medical tests to determine if we have too much or too little GABA activity. Excessive use of street drugs, alcohol, and prescription drugs are associated with low GABA activity and thus a state of excitation. Caffeine, in particular, inhibits the release of GABA and allows the increase of excitatory neurotransmitters.
GABA, glutamine and glutamate are intimately involved in a cycle that ultimately determines the level of each in the body. Neurons are not able to perform new synthesis of the neurotransmitters glutamate and GABA from glucose. The glutamate-GABA-glutamine cycle is a metabolic pathway that describes the release of glutamate or GABA from neurons, which are then taken up into astrocytes (star shaped glial cells). In return, astrocytes release glutamine to be taken up into neurons for use as a precursor to the synthesis of glutamate or GABA. This cycle, therefore, determines whether more GABA or more glutamate is produced.
Think of glutamic acid, glutamine and GABA as three members of a close-knit family with three very different personalities. Glutamic acid is a non-essential amino acid (the body can manufacture it when things are working right) that is also an excitatory neurotransmitter. Its cousin GABA has an opposite personality—it calms our nerves and relaxes us. Glutamine is the source for both of them—the body can make either glutamic acid or GABA from glutamine, depending on what is needed. Glutamine, therefore, is the gatekeeper chemical that determines the amount of GABA and glutamate levels to be produced to keep them in balance.
 If you are in a state of anxiety caused by sympathetic overtone (as commonly seen in advanced AFS) or a severe inflammatory state, glutamine’s focus will be shifted automatically to make more GABA to calm the body in theory, which will in turn lower your glutamate level, and help calm you down. Unfortunately, this pathway can be disrupted because an inflammatory state can cause dysregulation of the cycle itself, leading to excess production of glutamate levels instead. This is why it is very hard to predict the overall net effect of glutamine and it is not unusual for a variety of outcomes when taken by seemingly homogeneous populations. This happens most frequently in a body with chronic weakness, such as that of AFS. This may explain why some people do well with GABA brain boosting supplements, but others can have paradoxical reactions. Similarly, glutamine is also a support for GI health, but it may increase glutamate and cause anxiety as well.
If you are in a state of anxiety caused by sympathetic overtone (as commonly seen in advanced AFS) or a severe inflammatory state, glutamine’s focus will be shifted automatically to make more GABA to calm the body in theory, which will in turn lower your glutamate level, and help calm you down. Unfortunately, this pathway can be disrupted because an inflammatory state can cause dysregulation of the cycle itself, leading to excess production of glutamate levels instead. This is why it is very hard to predict the overall net effect of glutamine and it is not unusual for a variety of outcomes when taken by seemingly homogeneous populations. This happens most frequently in a body with chronic weakness, such as that of AFS. This may explain why some people do well with GABA brain boosting supplements, but others can have paradoxical reactions. Similarly, glutamine is also a support for GI health, but it may increase glutamate and cause anxiety as well.
Generally speaking, if you keep the total amount of glutamate in your body under control, you can prevent excitation responses. For example, excessive glutamate in Chinese food prepared with flavoring enhancer monosodium glutamate (MSG), dubbed the Chinese restaurant syndrome can cause nervousness, headaches, numbness, facial pressure, and anxiety.
Excessive GABA can result in a number of detrimental effects including:
Recommended dosage: Take 100 to 1000 mg in divided doses. GABA is commonly elevated in sufferers with advanced AFS. It is not clear why. Supplementing with GABA may not seem wise, but many have clinically reported benefit under these situations, especially for daytime anxiety control. Taking L-theanine is a lot more helpful in this situation and probably safer than other brain boosting supplements. It’s just weaker all around as it needs to be converted into GABA and serotonin. It is not recommended that GABA be taken in high doses (500 mg or more) at bedtime as it can cause an alert state and possibly stimulate the production of other neurotransmitters that may prevent falling asleep.
5. L-Theanine. L-theanine is another amino acid and a precursor to serotonin. It also helps in the production of GABA and dopamine. Theanine is related to another non-essential amino acid, glutamine. It is considered to be psychoactive since it has the ability to penetrate the blood-brain barrier.
As an alternative to GABA or L-glutamine to support a calming of the brain, one can take the amino acid L-theanine. L-theanine is converted to several useful calming and mood-elevating substances in the brain, including GABA. Therefore, one can use theanine as a kind of bank shot to bypass the blood brain barrier issue with respect to GABA.
Because L-theanine is known for helping to relieve stress and provide relaxation it is used in some sleep remedies in conjunction with low dose 5-HTP, GABA, melatonin, and calming herbs like passionflower and valerian root.
Recommended dosage: Take 200 to 400 mg once or twice daily. Those with advanced AFS need to be on alert for paradoxical reactions. Stop supplementation if this occurs.
 6. Taurine. Taurine is an amino acid that calms the nervous system by facilitating the production of the neurotransmitter GABA. By helping to raise GABA levels, taurine allows the body to manage anxiety so that your thoughts don't go spiraling out of control and you don't experience the associated cortisol and adrenaline spikes seen in Adrenal Fatigue Syndrome.
6. Taurine. Taurine is an amino acid that calms the nervous system by facilitating the production of the neurotransmitter GABA. By helping to raise GABA levels, taurine allows the body to manage anxiety so that your thoughts don't go spiraling out of control and you don't experience the associated cortisol and adrenaline spikes seen in Adrenal Fatigue Syndrome.
Take taurine for better sleep, but make sure you are getting a magnesium supplement that your body can absorb as well. Together these nutrients are the answer to abolish stress, calm the nervous system, and help you sleep better. You'll also have an overall improved mood. People who are deficient in either magnesium or taurine are at greater risk for depression and poor motivation.
Magnesium is well known to calm the nervous system, while countering fatigue. Similarly, taurine raises GABA levels, calming the nervous system and lowering anxiety and stress hormones that hinder rest.
Recommended dosage: A 500 to 2000 mg dosage range has shown efficacy, although the upper limit for toxicity is placed at a much greater level and high doses are well tolerated. The upper limit for which one can be relatively assured no side effects will occur over a lifetime has been suggested to be 3 grams a day. Taurine is a natural diuretic and may cause excessive urination and drop in blood pressure in high amounts.
7. Glycine. Glycine is one of the most common amino acids found within human proteins. It is particularly important clinically in supporting healthy digestive and central nervous systems and chronic fatigue. Within the central nervous system glycine works together with taurine and GABA as an inhibitory neurotransmitter. It interferes with the hyperexcitability of the CNS neurons by regulating chloride and potassium balance. It has been shown to be beneficial for disorders such as hyperactivity, anxiety, obsessive-compulsive disorder, schizophrenia, bipolar, and epilepsy. Due to its neuro-inhibitory effect, glycine calms the brain and is thus helpful in treating depression and insomnia as well. Glycine also helps in supplying glucose to the body and thus helps to alleviate fatigue.
Recommended dosage: Take 1 to 3 grams for anxiety or sleep. Up to 100 grams is needed for schizophrenia.
8. L-DOPA / Tyrosine. L-DOPA has the capability of penetrating the blood-brain barrier and is the precursor of dopamine and as we know, dopamine is involved in the production of noradrenaline, which converts into adrenaline. Supplementing with L-DOPA can increase the levels of dopamine in the system, but it won’t necessarily increase the levels of norepinephrine over the levels of adrenaline. Many factors are involved in balancing the equilibrium in the nervous system so it isn’t that straightforward.
Instead of supplementing with L-DOPA, you can supplement with the amino acid tyrosine, which is a precursor of L-DOPA. Tyrosine contains many different proteins but it is not as effective since it must go through an additional step in order to produce L-DOPA. Tyrosine brain boosting supplements may be considered for someone having below normal reference ranges of it and if there are no clinical contraindications.
Recommended dosage: Take 500 to 5000 mg daily in divided doses. Up to 20 grams has been used by researchers to improve cognitive function.
Alert: Overuse of tyrosine can push the body into an over-excitatory state and trigger an adrenal crash, panic attack, and heart palpitations. Don’t take L-tyrosine if you have problems with chronic headaches or bellyaches because the supplement might trigger these conditions. If you have problems with hyperthyroidism, such as with Graves' disease, avoid tyrosine.
 9. Neuromodulators and Precursors. The following are commonly used:
9. Neuromodulators and Precursors. The following are commonly used:
Phosphatidyserine (PS) is derived from soy lecithin a component of cell membranes. PS is helpful in repairing damaged cell membranes as well as repairing the cortisol receptors located in the hypothalamus. When cortisol levels are too high it is believed this elevation damages the receptors, which impairs the hypothalamus’ ability to detect when levels of cortisol are too high and to correct the problem. The stronger the phospholipid layer of the cell, the more efficiently the NTs can be transported. PS can be used successfully to help calm elevated cortisol levels at night and induce sleep. Nonetheless, for reasons that are not well understood paradoxical responses are common.
As simple as it may seem, most self-navigating natural NT repletion programs fail, just as most medications that attempt repletion of NTs also fail over time. Those who are under stress, in particular, are at risk of failure. Sufferers of adrenal fatigue are most vulnerable, especially in advanced stages when their HPA hormonal axis is deranged. It is clear that a body under stress will negatively impact the effectiveness of any NT balancing program and in particular, SSRIs and brain boosting supplements. A comprehensive NT balancing program must take this into account to be successful. Let us study why.
 The hypothalamic-pituitary-adrenal (HPA) hormonal axis connects sensory signals (such as smell) received from the outside world into NTs in the brain that further travel to various organs and trigger the release of over fifty hormones that help the body deal with daily living and stress. Remember that stress can be physical or emotional. Moreover, perceived stress is a more powerful trigger of the HPA axis than actual stress. The HPA axis is put in overdrive and the adrenal glands overburdened if the body is exposed to chronic stress. If the stress is unrelieved, the adrenal glands becomes overburdened from living in a wired state.
The hypothalamic-pituitary-adrenal (HPA) hormonal axis connects sensory signals (such as smell) received from the outside world into NTs in the brain that further travel to various organs and trigger the release of over fifty hormones that help the body deal with daily living and stress. Remember that stress can be physical or emotional. Moreover, perceived stress is a more powerful trigger of the HPA axis than actual stress. The HPA axis is put in overdrive and the adrenal glands overburdened if the body is exposed to chronic stress. If the stress is unrelieved, the adrenal glands becomes overburdened from living in a wired state.
Adrenal Fatigue Syndrome represents the end result of the body’s neuroendocrine response to stress. In early stages of AFS, anti-stress hormone cortisol output from the adrenal cortex rises as the adrenal glands are put in overdrive because of the HPA axis. In advanced stages of AFS, cortisol depletion sets in as the HPA becomes dysregulated and the adrenal glands reach exhaustion. This is when adrenal epinephrine and brain NT norepinephrine output takes center stage as the body enters the flight-or-fight alarm response.
HPA axis dysregulation from chronic stress is associated closely with NT regulation. For one to function properly, the other must be in balance and synchronization. Without proper balance, the overall condition can easily worsen.
For example:
 Many people have negative outcomes when they take 5-HTP and glutamine as well as L-theanine. These are supposed to raise GABA, an inhibitory NT and reduce anxiety commonly experienced by those with advanced AFS. However, these three compounds often cause paradoxical reactions instead. They can trigger adrenal crashes and further over stimulation of the excitatory pathways for reasons not known instead of inhibiting it. This negative chain reaction can make a whole range of symptoms much worse. The reverse can happen. Taking in more GABA when laboratory levels already show high GABA levels may produce clinically positive results of relaxation for reasons not known.
Many people have negative outcomes when they take 5-HTP and glutamine as well as L-theanine. These are supposed to raise GABA, an inhibitory NT and reduce anxiety commonly experienced by those with advanced AFS. However, these three compounds often cause paradoxical reactions instead. They can trigger adrenal crashes and further over stimulation of the excitatory pathways for reasons not known instead of inhibiting it. This negative chain reaction can make a whole range of symptoms much worse. The reverse can happen. Taking in more GABA when laboratory levels already show high GABA levels may produce clinically positive results of relaxation for reasons not known.We are still very much in the infancy of NT research. There is much we do not know. What is clear is that NTs are very much interconnected with each other. While we have some good understanding on the physiology of each NT individually, overall clinical outcomes remain hard to project with accuracy. This is especially true in the advanced AFS setting or for those most at risk due to concurrent chronic conditions in which the body is already on edge in an alarm response. The slightest adjustments of NTs can upset the internal NT balance that is fragile at best. Any additional intrusion into the already fragile internal homeostasis, such as receptor disorders or extracellular matrix congestion, can lead to exaggerated or paradoxical responses. Severe anxiety, a wired state, and fatigue can be triggered as the risk of an adrenal crash increases.
An example of this is with selective serotonin reuptake inhibitors (SSRIs) antidepressant medications, which are very helpful in treating panic attacks. SSRIs cause serotonin levels to rise. Over time, this is not an effective way of treating stress because you’ll develop a tolerance and even with more antidepressant medication, the body just becomes desensitized to the added availability of serotonin during the neurotransmission, and the depression, wired state, and fatigue persists. This negative scenario is frequently seen in people who are put on antidepressants by their private physician while AFS is overlooked, resulting in a worsening of their depression.
When HPA axis dysregulation, NT imbalance and advanced AFS are all present at the same time an autonomic nervous system is in high gear, or a wired state, the clinical picture becomes very convoluted and complex. For example, overemphasis on NT repletion can trigger excitotoxicity and adrenal crashes. Too little NT repletion can retard the overall AFS recovery. Too much adrenal support can trigger NT excitation, and too little adrenal support will lead to increased NT repletion dependency. Regular NT pathways are disrupted in a body that is fragile and sensitive.
A carefully planned and balanced approach after an in depth history is taken is best with focus placed on both NT repletion and helping the body heal from AFS concurrently. The more advanced the AFS, the more focus and priority should be placed on healing the AFS first.
 For example, amino acids and herbal remedies can be detrimental if the adrenals are not stabilized first or if the liver is congested and the extracellular matrix polluted. If you want to decrease your levels of norepinephrine while at the same time increasing serotonin levels, then certain supplements would not be advised. For example, people often try to treat depression by supplementing with St. John’s Wort, but if they have extremely high levels of norepinephrine, it’s not a good idea since this would increase their norepinephrine levels even more by their association with the HPA axis which can be put in overdrive during the process.
For example, amino acids and herbal remedies can be detrimental if the adrenals are not stabilized first or if the liver is congested and the extracellular matrix polluted. If you want to decrease your levels of norepinephrine while at the same time increasing serotonin levels, then certain supplements would not be advised. For example, people often try to treat depression by supplementing with St. John’s Wort, but if they have extremely high levels of norepinephrine, it’s not a good idea since this would increase their norepinephrine levels even more by their association with the HPA axis which can be put in overdrive during the process.
Sometimes people use melatonin to help them sleep. Melatonin begins with the turning on of sympathetic nerve tracks in the brain that secrete the NT norepinephrine which in turn stimulates cells it the pineal gland to produce melatonin. This may not be problematic for some, but for those in advanced AFS where the body is already flooded in a sea of norepinephrine, any excess can make insomnia worse and trigger adrenal crashes.
Therefore, a comprehensive recovery plan needs to have components that address NTs, HPA axis dysregulation, adrenal function, liver congestion, extracellular matrix pollution, dietary concerns, environmental toxins etc., to be effective long term.
One of the classic signs or NT imbalance in a setting of advanced AFS is a state called wired and tired. There are several mechanisms that can lead to this wired state, one of which is NT imbalance.
Advanced AFS sufferers are typically in a state of constant fatigue, but yet unable to fall asleep. Those who are able to fall asleep typically wake up after a few hours and are unable to return to sleep easily. In the morning, they are unrefreshed as a result. Furthermore, many are anxious or in a wired state, during the day, with energy slumps in the afternoon. When it is time to go to sleep, the body is again in a wired state. It may take a long time to fall asleep, only to be awakened in a few hours and once more the cycle repeats itself. This can go on for years. Over time, the body becomes weakened. Sleep medications are often required, and over time, dependency and tolerance issues develop.
In addition to NT imbalance, which is a causative factor of poor sleep, research has shown that much of the wired state, or feeling wired and tired, is the result of a body flooded in stimulatory catecholamines. Other contributing factors to a wired state include liver congestion and extracellular matrix pollution. When the body alarm response is activated because of stress, a state of sympathetic overtone (high norepinephrine typical of early Stage 3C AFS) or reactive sympathetic response (high norepinephrine and adrenaline typical of late Stage 3C AFS) is prevalent. Other symptoms associated with this state include heart palpitations, reactive hypoglycemia, posturalorthostatic hypotension, and dizziness.
 Normalizing a body in this wired state is a very challenging process because the body is often hypersensitive at this stage so that the smaller adjustment in NT can trigger exaggerated responses in some and paradoxical responses in others. Most failure in resolving this state of wired and tired comes from the failure to recognize NT function, dosage error, improper delivery system, and a mentality of trying to fix the sleep or anxiety problems rather than looking at insomnia and anxiety as part of the overall consequence of a body in full state of alarm. Because this alarm state is twenty-four seven, successful resolution involves a twenty-four seven approach.
Normalizing a body in this wired state is a very challenging process because the body is often hypersensitive at this stage so that the smaller adjustment in NT can trigger exaggerated responses in some and paradoxical responses in others. Most failure in resolving this state of wired and tired comes from the failure to recognize NT function, dosage error, improper delivery system, and a mentality of trying to fix the sleep or anxiety problems rather than looking at insomnia and anxiety as part of the overall consequence of a body in full state of alarm. Because this alarm state is twenty-four seven, successful resolution involves a twenty-four seven approach.
A battery of natural compounds, dietary and lifestyle modifications are required to support and ensure smooth NT balance throughout the day.
Nutritional supplementation and hormones focused on NTs need to be different for each phase of the day to match the desired goal. Here are some considerations:
Additional organ specific nutrients to support NT balance can be deployed. They include:
 Adrenal support: vitamin C, mineral ascorbate, ascorbyl palmitate, pantethine (B5), pregnenolone, DHEA
Adrenal support: vitamin C, mineral ascorbate, ascorbyl palmitate, pantethine (B5), pregnenolone, DHEAIt should be clear that NT balancing is a highly technical aspect of nutritional medicine requiring in-depth clinical experience due to its complexity and lack of well correlated scientific clinical markers. The rather simplistic approach of simply replenishment of what appears to be depleted on the surface based on laboratory testing seldom works and in fact can worsen the overall condition over time.
A comprehensive plan is necessarily tedious, time consuming and all encompassing because we are dealing with chemicals that have wide ranging ramifications throughout the body. Most NT imbalances have underlying root causes that need to be addressed to effect long-term healing. This is especially true when NT occurs in a setting of AFS. Fortunately, once NTs are stabilized, the recovery program can be discontinued. The younger the sufferer, the faster is the recovery. Unfortunately, most people tend to underestimate or are unaware of the long-term negative consequences of NT imbalance. Many heath care practitioners are not well educated in this aspect of medicine. Sufferers are put through many trial and error attempts, which can worsen the overall condition.
Neurotransmitter balance is key to vitality and optimum health. Imbalanced NT is a common occurrence in advanced stages of AFS. Balancing NTs requires a thorough knowledge of each specific NT and its interaction with others because all NTs are connected biochemically. Laboratory studies of NTs need clinical correlation to be useful. A detailed history by an experienced physician is far more accurate. The proper use of food, micronutrients, lifestyle, and exercise can help restore proper NT balance. Always remember that NT imbalance is more often than not secondary to an underlying disease, and that is why most NTs self-correct once the underlying condition is resolved.
That is an interesting question. Normal, the body self-adjusts. However, in severe cases, the thyroid function could be permanently affected. In such case, during and even after anorexia is resolved, there are residual problems with thyroid that can remain for a long time.
The cortisol produce by the adrenal glands is anti-inflammatory. When the adrenals are fatigued, cortisol production goes down, and your body becomes more sensitive and sensitivities to food, chemicals will start surfacing.
Modern medicine is controlled by the pharmaceutical companies, where the big bucks are. Using food to improve health does not generate the money.
"I just wanted to say THANK YOU for taking me on as a client"
"
Dear Health Coaches:
First of all, I just wanted to say THANK YOU for taking me on as a client. I can't tell you how comforting it is to actually be able to work with people who are so knowledgeable about this complex condition. It has been such a confusing and scary journey over the past 20 years.
I am very sensitive to any change going on in my body - good or bad - so I always have to go very slow when starting anything new or making any changes From reading all the info in the books and on the site, I can tell you have worked with people like me before (and some who are probably much worse) so it's comforting to know you understand my sensitivity and that I will have to go really slowly. Other doctors in the past have just thought I was being a hypochondriac and not believed me or tried to rush me through protocols and just made my situation much worse.
Thanks so much for your time.