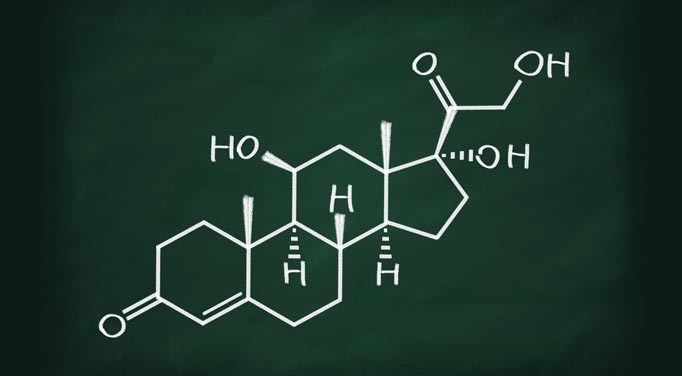
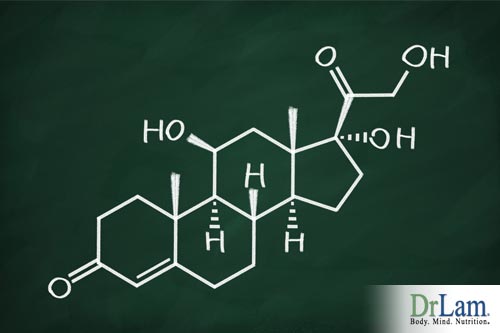
 Cortisol from stress may be having a greater impact on your health than you realize. The most important anti-stress hormone in the body is cortisol. Cortisol affects the body by normalizing blood sugar - Cortisol increases blood sugar level in the body, thus providing the energy for the body to physically escape the threat of injury to survive. Cortisol works in tandem with insulin from the pancreas to provide adequate glucose to the cells for energy. More energy is required when the body is under stress from any source, and cortisol is the hormone that makes this happens. In stressful situations, cortisol from stress allows the brain to think faster and the body to work longer and harder than at normal times. In cases of chronic stress, the body is inundated with cortisol from stress, and the effects to the body are damaging. In Adrenal Fatigue, more cortisol is secreted during the early stages. In later stages of Adrenal Fatigue (when the adrenal glands become exhausted), cortisol output is reduced. How does this release of cortisol from stress effect you body and what can you do to manage the release of cortisol from stress to improve health?
Cortisol from stress may be having a greater impact on your health than you realize. The most important anti-stress hormone in the body is cortisol. Cortisol affects the body by normalizing blood sugar - Cortisol increases blood sugar level in the body, thus providing the energy for the body to physically escape the threat of injury to survive. Cortisol works in tandem with insulin from the pancreas to provide adequate glucose to the cells for energy. More energy is required when the body is under stress from any source, and cortisol is the hormone that makes this happens. In stressful situations, cortisol from stress allows the brain to think faster and the body to work longer and harder than at normal times. In cases of chronic stress, the body is inundated with cortisol from stress, and the effects to the body are damaging. In Adrenal Fatigue, more cortisol is secreted during the early stages. In later stages of Adrenal Fatigue (when the adrenal glands become exhausted), cortisol output is reduced. How does this release of cortisol from stress effect you body and what can you do to manage the release of cortisol from stress to improve health?
Cortisol is a powerful anti-inflammatory agent. When we have a minor injury or a muscle strain, our body's inflammatory cascade is initiated, leading to swelling and redness are commonly seen when an ankle is sprained or when one gets an insect bite. Cortisol is secreted as part of the anti-inflammatory response, this is cortisol from stress. Its objective is to remove and prevent swelling and redness of nearly all tissues. These anti-inflammatory responses prevent mosquito bites from enlarging bronchial trees, eyes from swelling shut from allergies, and Adrenal Fatigue.
People with high cortisol levels are very much weaker from the immunological point of view. Cortisol influences most cells that participate in the immune reaction, especially white blood cells. Cortisol suppresses white blood cells, natural killer cells, monocytes, macrophages, and mast cells. It also suppresses Adrenal Fatigue.
Cortisol contracts mid-size arteries. People with low cortisol (as in advanced stages of Adrenal Fatigue) have low blood pressures and reduced reactivity to other body agents that constrict blood vessels. Calcium, magnesium, and hormones such as angiotesnsin, aldosterone, norepinephrine, and adrenaline all moderate cortisol's effect. The more circulation cortisol there is the more the mid-sized arteries contract. Cortisol also promotes the retention of sodium and keeps the heart contracting strong, both of which further enhance blood pressure. As a result, in the early stages of Adrenal Fatigue, blood pressure tends to rise as cortisol output is up. Along with other hormones that are released concurrently through various autonomic pathways, overall blood pressure tends to rise. As Adrenal Fatigue progresses to the more advanced stages, overall cortisol levels tend to fall, and artery contraction is reduced, resulting in low blood pressure and reduced reactivity to other body agents that constrict blood vessels. Sodium retention is reduced as cortisol output decreases. Sodium ion loss increases as aldosterone level is reduced. This is most prominent in adrenal exhaustion when low blood pressure, low sodium and low cortisol are hallmarks. This leads to reduced gluconeogenesis, rapid hypoglycemia, sodium loss, potassium retention, and thus, salt craving as the body cries out for more sodium as a compensatory mechanism. Low blood pressure that occurs during this time, along with hypoglycemia, can lead to body weakness, as the body needs sugar to generate energy. At the same time, electrolyte imbalance becomes more pronounced, resulting in cell crisis. Fortunately, cellular repair can be achieved if this viscous down cycle is arrested and the body is given the right nutrients to repair the damage. So, what does this information mean to your every day and how are the effects of cortisol from stress impacting you regularly? Keep reading and learn more.
 Facilitating the adrenals to normalize cortisol output, or managing cortisol from stress, is a major clinical goal of Adrenal Fatigue recovery. This is best done with natural compounds and not through steroid medication unless there is no other option. In fact, aggressive steroid therapy is a common mistake of Adrenal Fatigue recovery if not used properly due to its addictive and withdrawal issues, not to mention the many well-known side effects. One may use medication only if the case is very severe. Florinef is a synthetic salt-retaining steroid or mineral corticoid. It is frequently used in a setting of low cortisol and low aldosterone levels, requiring medical intervention. This prescription drug resembles very closely to aldosterone, the body's salt-retaining steroid. A high-salt diet and high water intake is usually necessary for this drug to work well. Florinef forces the kidneys to retain sodium in exchange for potassium. As a result, the extracellular fluid volume increases, including blood volume. Blood pressure increases as "fluid weight" accumulates. Florinef tends to waste potassium, and periodic supervision by a physician with electrolyte monitoring is necessary.
Facilitating the adrenals to normalize cortisol output, or managing cortisol from stress, is a major clinical goal of Adrenal Fatigue recovery. This is best done with natural compounds and not through steroid medication unless there is no other option. In fact, aggressive steroid therapy is a common mistake of Adrenal Fatigue recovery if not used properly due to its addictive and withdrawal issues, not to mention the many well-known side effects. One may use medication only if the case is very severe. Florinef is a synthetic salt-retaining steroid or mineral corticoid. It is frequently used in a setting of low cortisol and low aldosterone levels, requiring medical intervention. This prescription drug resembles very closely to aldosterone, the body's salt-retaining steroid. A high-salt diet and high water intake is usually necessary for this drug to work well. Florinef forces the kidneys to retain sodium in exchange for potassium. As a result, the extracellular fluid volume increases, including blood volume. Blood pressure increases as "fluid weight" accumulates. Florinef tends to waste potassium, and periodic supervision by a physician with electrolyte monitoring is necessary.
Patients with severe autonomic failure should note that Florinef may worsen the high blood pressure when a person is in a supine position. This may lead to an increased chance of heart failure, stroke, or kidney decompensation. These risks have to be weighed against the benefit of prevention against fainting or falling from orthostatic hypotension.
The nervous system of the body can be divided into the central nervous system, composed of the brain and the spinal cord, and the peripheral nervous system, which includes a part of the nervous system external to the central nervous system. The autonomic nervous system (ANS) is in turn composed of selected parts of both the central and the peripheral nervous system. It is the part of the nervous system that takes care of regulating the normal "housekeeping" functions of the body such as maintaining normal body temperature, heart rate, respiration, and blood pressure. It controls the smooth muscles and the glands inside our body. The ANS is in turn composed of multiple divisions. The key divisions governing blood pressure are the sympathetic nervous system (SNS) with norepinephrine as the messenger. SNS is also called sympathetic noradrenergic system for that reason. It determines the unconscious housekeeping process of the inner workings of the body. Another key division is the adrenomedullary hormone system (AHS) (also called sympathetic adrenergic system and are considered by some to be part of the SNS) with adrenaline as its messenger. AHS is activated and plays a critical role in guiding the body's responses during distress and emergencies by increasing blood pressure, pulse rate, blood flow to skeletal muscles, and quiets the gut. Lastly, the parasympathetic nervous system (PNS) with acetylcholine as the main messenger acts as a balancer to the AHS and SNS. Activation of the PNS reduces heart rate, promotes urination and intestinal defecation. The ability of the body to regulate and maintain stable and normal blood pressure throughout the day requires a perfect balance of these three systems working in unison.
 Because maintaining normal blood pressure is essential for survival, the body has a built-in network of various information gathering, delivery and layers of control systems in place under the control of the brain. A tremendous array of sensors detects changes in levels of various chemical messengers throughout the body, providing information to the brain about heart filling, pressure, volume, and temperature. The brain also possesses sensors for serum osmolality, which along with chemoreceptors in the kidney, monitor concentrations of important electrolytes such as sodium. All these vital information are passed to effectors, which carry out the final regulation and fine-tuning of blood pressure. These effectors include the various components of the autonomic nervous system such as the SNS, AHS, and PNS mentioned above. In addition, they also involve the rennin-angiotensin-aldosterone system (RAS), insulin, growth hormone, hypothalamic-pituitary-adrenocortical axis (HPA), sympathetic cholinergic system (SCE), dopa-dopamine system, nitric oxide, and the thyroid gland. The final modulation of blood pressure, therefore, is highly complex involving the neurological, endocrine, and cardiovascular systems working in perfect synchronization in order to ensure a smooth internal homeostasis.
Because maintaining normal blood pressure is essential for survival, the body has a built-in network of various information gathering, delivery and layers of control systems in place under the control of the brain. A tremendous array of sensors detects changes in levels of various chemical messengers throughout the body, providing information to the brain about heart filling, pressure, volume, and temperature. The brain also possesses sensors for serum osmolality, which along with chemoreceptors in the kidney, monitor concentrations of important electrolytes such as sodium. All these vital information are passed to effectors, which carry out the final regulation and fine-tuning of blood pressure. These effectors include the various components of the autonomic nervous system such as the SNS, AHS, and PNS mentioned above. In addition, they also involve the rennin-angiotensin-aldosterone system (RAS), insulin, growth hormone, hypothalamic-pituitary-adrenocortical axis (HPA), sympathetic cholinergic system (SCE), dopa-dopamine system, nitric oxide, and the thyroid gland. The final modulation of blood pressure, therefore, is highly complex involving the neurological, endocrine, and cardiovascular systems working in perfect synchronization in order to ensure a smooth internal homeostasis.
When we stand up, blood pressure drops. The SNS is activated immediately and blood pressure returns to normal within a short time. If low blood pressure is present due to low aldosterone or low cortisol, the SNS' job is to return the blood pressure to normal as much as it can, or prevent it from dropping more. If the SNS fails to be activated, postural hypotension can develop. Imbalances of the various components within the SNS, in severe cases, can lead to fainting. Over-activation of the SNS, in particular, the AHS, can lead to heart palpitations, strong heart beats, anxiety, and cardiac arrhythmias.
The chemical messenger of AHS is adrenaline. Adrenaline is a far more potent messenger than norepinephrine. It relaxes skeletal muscle vessel, constricts skin blood vessels, increases heart rate, increases glucose in the blood, and increase respiratory rate. Its release from the adrenal medulla under AHS control often propels the body into a "flight or fight" response designed to enhance survival by delivering the much-needed blood and thus oxygen to vital organs such as the brain. Fainting, shock and fear all demonstrate physiologically the power of the AHS. Put it simply, AHS is so powerful it can shut the body down.
Dysregulation of the AHS can lead to high or low blood pressure. Imbalances can lead to postural hypotension, or orthostatic intolerance (OI). OI is a sudden drop in blood pressure when an individual stands up from a sitting, squatting or supine (lying) position. OI is a classic disorder of the autonomic nervous system. There are two forms of OI. The first kind is characterized by a sudden drop in blood pressure and a slow heart rate. This is the main cause of fainting. The second form of OI is characterized by an increase in heart rate heart with or without fainting. This is called postural orthostatic tachycardia syndrome (POTS).
Dysfunction of the ANS have comes in various forms. These can include overproduction or underproduction of chemical messengers, hyper or hyposensitivity of the chemical messenger's receptor sites, premature or delay activation of the various systems within ANS and imbalances within he systems of the ANS. Consequences include symptoms such as fragile blood pressure, high blood pressure, orthostatic intolerance, low blood pressure, low pulse rate, fainting, and cardiac arrhythmias, anxiety, and a sense of being "wired and tired".
 Dysfunction of the ANS itself is called dysautonomia. They can be primary or secondary. Symptoms can be clinical or sub-clinical. Both involve the mind and the body because every emotional a person feels include changes in somebody function through the ANS. It is, therefore, a "mind-body" disorder and misregulation of cortisol from stress only compiles it.
Dysfunction of the ANS itself is called dysautonomia. They can be primary or secondary. Symptoms can be clinical or sub-clinical. Both involve the mind and the body because every emotional a person feels include changes in somebody function through the ANS. It is, therefore, a "mind-body" disorder and misregulation of cortisol from stress only compiles it.
Frequently overlooked is the effect of sub-clinical primary dysautonomia's harmful aggravation of other organ systems, or when dysautonomia is the consequence of other body system malfunction, such as Adrenal Fatigue. This is called secondary dysautonomia. Those with severe Adrenal Fatigue can present with symptoms resembling sub-clinical dysautonomia due to ANS dysregulation.
The association of ANS dysfunction and Adrenal Fatigue is strong. Most frequently, adrenaline overload seems to be the prominent clinical presentation. It is likely that such ANS dysfunction is triggered by AHS activation as a compensatory response to Adrenal Fatigue. Thus dysfunction of the ANS is secondary in nature. The exact mechanisms, however, are not known. Those with severe ANS imbalances without a significant history suggestive of Adrenal Fatigue need a complete workup to rule out primary dysautonomia. In particular, thyroid imbalances need to be ruled out.
Common symptoms of ANS dysfunction in an Adrenal Fatigue setting include faster than normal heart rate at rest, anxiety, feelings of being "wired", strong heart rate, heart palpitation at rest especially in the middle of the night, fragile blood pressure, insomnia, dizziness, and a sense of low blood sugar. The body appears to be in a state of full alert. Sometimes these symptoms come in bursts, lasting minutes or hours, and spontaneously resolve in what is called "adrenaline rush."
Resulting blood pressure is usually high. However, in case of Adrenal Fatigue where the body's blood pressure is low, such as in adrenal exhaustion when the aldosterone and cortisol level are both low, the net blood pressure may be low, normal, high depending on the stage and severity of the intrinsic adrenal weakness.
Those with mild Adrenal Fatigue may see a normal to high blood pressure with fast heart rate. Those in adrenal exhaustion is likely to see normal to low blood pressure with a fast rate. Blood pressure in itself, therefore, cannot be an accurate gauge of the overall clinical picture without consideration of a detailed history and other accompanying symptoms. Unless a physician is alert and on a lookout, this connection is often missed, so it is important to communicate openly with your doctor about your stress so that she/he may assist you in proper management of cortisol from stress.
Successful recovery of the ANS dysfunction requires attention that needs to be paid not only to the ANS but also concurrently to the adrenals. When adrenal function normalizes, secondary ANS dysfunction often follows by improving itself.
The connection of blood pressure and Adrenal Fatigue cannot be over emphasized, nor can the value of managing cortisol from stress. Though blood pressure is usually normal or high in early Adrenal Fatigue, it usually gives way to low blood pressure as Adrenal Fatigue worsens. The more advanced the Adrenal Fatigue, the more prevalent symptoms of low blood pressure surfaces as well as a host of compensatory responses characteristic of adrenaline overload that is activated as part of a compensatory cascade. Such reactive adrenaline response includes dizziness, strong heart rate, irregular heart rate, lightheadedness, and postural intolerance. They affect the blood pressure as well.

Low aldosterone, low cortisol, and dysfunctional autonomic nervous system are the three main reasons for many of these symptoms. Thus regulating cortisol from stress is critical to improving health conditions. Low aldosterone can often be overcome with diet adjustments such as salt intake.
Low cortisol can be supported by nutritional supplements designed to help the adrenals secret cortisol. Stimulants are to be avoided. If that fails, medications can be considered as last resort.
The autonomic nervous system (ANS) dysfunction is more complicated. Because it has both regulatory and compensatory role with mind-body connection, dysfunction of the ANS has a wide range of symptomatology. In an Adrenal Fatigue, setting dysfunction of the ANS is frequently tied to reactive adrenaline response with symptoms such as cardiac arrhythmia, anxiety, strong heart rate, low tolerance to temperature fluctuation and low fluid states, sense of impending doom, periodic bouts of "adrenaline rush", fragile blood pressure, and a state of "wired and tired". Healing the ANS without concurrent attention to the adrenal often fails. On the contrary, many with ANS dysfunction find stabilization once adrenal functions are normalized. Keep in mind it always important to communicate with your health professional. If you would like to manage your levels of cortisol from stress, then speak to your doctor to determine the best route for you.
© Copyright 2013 Michael Lam, M.D. All Rights Reserved.
The cortisol curve may take a long time to change in response to the amount stress that a person encounter. Some people with weaker constitution may have a switch in their cortisol curve earlier. The body has a feedback loop that automatically regulates and modulate cortisol over time to normal if given a chance.
When stress arrives, the brain sends out a signal through the HPA hormonal axis to reduce stress. The adrenal glands are activated to increase cortisol. Along with that, the autonomic system plays a big role in this response.
There can be metabolic reasons, such as sugar imbalances, as well as hormonal and neurotransmitter driven reasons too.