Stress enters our sphere through a small area of the brain stem called the locus coeruleus (LC) (also spelled locus caeruleus). Discovered in the Eighteenth century, this area of the brainstem deals with physiological responses to stress and panic.
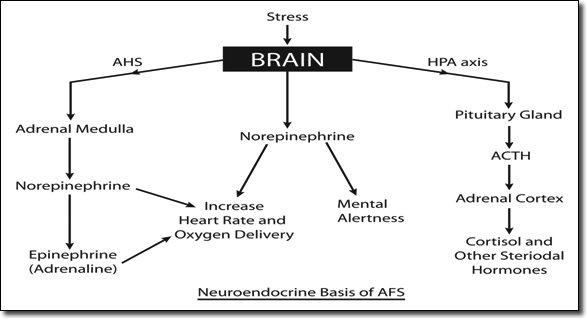
As an important homeostatic control center of the body, the LC receives input signals from a variety of sources, including the hypothalamus, amygdala, cerebellum, and prefrontal cortex. Emotional pain and stressors from the outside enters our inner world through these pathways. Once arrived, excitatory signals trigger production and release of norepinephrine from the LC. Norepinephrine has dual functions. In the brain, it acts as a neurotransmitter and keeps us aroused. It also acts as a hormone when outside the central nervous system (CNS), exerting its excitatory effects directly on the target organ concerned, such as the heart. As a result, both the force of the heartbeat as well as heart rate goes up. This is illustrated in the diagram below:
Aside from being the principal production site of brain norepinephrine, LC is also connected to many other parts of the (CNS) on the output side, including the spinal cord, the brain stem, cerebellum, hypothalamus, amygdale, and the cerebral cortex. Collectively, the LC and the areas of the CNS affected by the norepinephrine it produces are described as the locus coeruleus-noradrenergic system, or LC-NA system. Distribution is ubiquitous and consistent with a prominent role for norepinephrine (also called noradrenaline or NA) in a variety of CNS functions and behaviors that include locomotor control, cognition, motivation, and attention.
Once activated by stress, LC responds by increasing norepinephrine secretion, which in turn activates the HPA axis. Norepinephrine released from LC also increases the sympathetic discharge/inhibit parasympathetic tone in the peripheral nervous system. The body goes on alert and prepares for impending danger. Activation of the LC-NA system may be responsible for much of the psychological effect we see in Adrenal Fatigue Syndrome including fear, anxiety, alertness, memory changes, and REM sleep dysregulation. Psychiatric research has documented that the role LC plays in cognitive function in relation to stress is complex and multimodal.
The hypothalamus is an area of the brain located below the thalamus, just above the brain stem. By its various influences, the hypothalamus plays a key role in controlling hunger, sleep, thirst, circadian cycles, and body temperature. It is the beginning of the hypothalamus-pituitary (HPA) hormonal axis. About the size of an almond, it produces and secretes certain neurohormones, one of which we call the corticotrophin-releasing hormone (CRH). CRH is released when the hypothalamus is stimulated by norepinephrine from the LC. CRH travels to the pituitary gland and serves as a bridge to link the CNS to the endocrine system. The pituitary gland is an endocrine gland about the size of a pea and is a protrusion off the bottom of the hypothalamus at the base of the brain. It secretes nine hormones that keep the body in homeostasis. Upon arrival to the anterior pituitary gland, CRH triggers and induces the formation and release of adrenocorticotropic hormone (ACTH). ACTH travels to the adrenal cortex, and is responsible for orchestrating the synthesis of a family of steroids including cortisol, the master anti-stress hormone.
The HPA axis works concurrently and alongside the LC-NA system. The HPA axis goes into action when the LC-NA system is activated. While the LC-NA system's effect tends to localize to the CNS, the HPA axis effect, more diffused, affects the entire body, mediated by cortisol.
Therefore, the body has three well designed anti-stress mechanisms in place to protect us: brain norepinephrine keeps us alert in the CNS, systemic norepinephrine keeps our cardiovascular system ready to take action physically by way of the sympathetic nervous system (SNS), and a family of steroids from the adrenal cortex helps generate energy and reduce inflammation. Activating any or all of these three systems in varying degrees is enough to help us deal with unwelcomed stress under most normal circumstances.
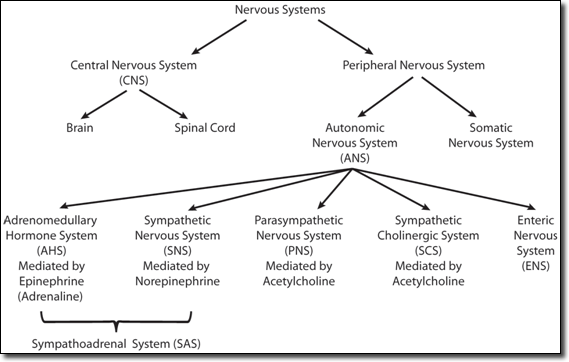
The SNS is part of the autonomic nervous system (ANS), which has 5 branches. Working together in unison, these 5 branches regulate the internal housekeeping functions of the body at rest and in emergency. The other 4 branches are: the parasympathetic nervous system (PNS), and the adrenomedullary hormonal system (AHS), the enteric nervous system (ENS), and the sympatheic cholenlergic system (SCS). Normal bodily housekeeping function of daily living is regulated by a perfect balance primarily by the PNS (and it chemical messenger acetylcholine) and SNS (and its chemical messenger norepinephrine). It is absolutely necessary for the SNS to be involved in regulating even small stressors such as standing up or exercise in order for daily living to be smooth. The widespread believe that the SNS is primarily activated and useful only in time of extremely stressful situations has been proven false. It is the AHS that is mainly responsible for the fight or flight response associated with extreme stress.
Thanks to the SNS, LC-NA system, and the HPA axis working together each time stressors arrive, individuals in early stages of AFS may experience stress, but seldom notice any significant clinical dysfunction. Working behind the scenes, they help us deal with stress without us knowing about it.
When stress becomes extreme, the adrenomedullary hormonal system (AHS), also known as the sympathetic adrenergic system, is activated. What makes the AHS physiologically unique is the way their synaptic pathways are structured. Synapses occur between pre- and post-ganglionic neurons of the AHS occur within the adrenal medulla instead of outside the adrenal glands, because the adrenal medulla develops in tandem with the SNS, and, therefore, acts as a modified sympathetic ganglion. The nerve fibers come directly from cell bodies in the spinal cord. The fibers pass through the para-vetebral ganglia and innervate by way of splanchnic nerves without relaying their signals via cells in the ganglia. This is a "direct link" highway. The speed of transmission is extraordinary fast as a result. Furthermore, the post- ganglionic neurons do not leave the medulla, as happens with regular SNS pathways. Instead, they directly release epinephrine and a proportionally small amount of norepinephrine into the bloodstream. Epinephrine, the most potent catecholamine, serves as an emergency hormone largely responsible for executing the fight or flight response, with norepinephrine as a helper. Upon release, epinephrine is carried to the cardiovascular system and other parts of the body. It increases blood glucose levels, increases pulse rate and blood pressure, quiets the gut, stimulates metabolism, and dilates blood vessels in skeletal muscle. At the heart, we see the rate and force of contraction increased. Key organs responsible for getting us out of physical danger, such as the heart, receives excitatory stimuli from norepinephrine directly transmitted through the SNS as well, in addition to that secreted from the adrenal medulla through the AHS. This double protection maximizes our chances of survival in times of danger.
From a neuroendocrine perspective, we have four anti-stress systems well in place within the body. They are the LC-NA system, HPA axis, SNS, and AHS. In varying degrees, all four systems work constantly around the clock and they balance each other to ensure homeostasis and help us with stress. Multiple feedback loops are in place to help accomplish this mission.
There is a clear and logical pattern of the activation sequence that defines how the body decides which system to activate, to what degree, and under what circumstances. Perceived stress, for example, may be handled differently hormonally than actual stress. Therefore, this gang of four serves an ongoing function to protect and serve our survival needs.
Any one of these systems can be overtaxed and dysregulated. The causes range from toxins, chronic stress, medications, and hereditary factors, just to name a few. Out of these, chronic stress is perhaps the biggest culprit. Overtaxed systems invariably lead to dysregulation and breakdown as a function of time. Symptoms of AFS are merely reflections of such activation burden, dysregulation, breakdown, compensatory effect, and ultimately collapse of this process over time. For example, we see classic signs of hypoglycemia and low blood pressure, both reflective of HPA axis dysregulation in early Adrenal Exhaustion. Dysregulation of the AHS with epinephrine overload tends to occur later on.
When stress enters the body, the immediate central command of the stress response lies in the brain. Controlled by the LC, mediated through the LC-NA system by the brain neurotransmitter norepinephrine, the body is aroused and put on alert when stress arrives at its doorstep. This action is immediate and localized to the CNS. The HPA axis is also activated and serves as the messenger chain that ultimately controls the field command center located in the adrenal cortex, where various hormones are produced, including cortisol. These hormones have a diffusive effect throughout the body, increasing energy and glucose, and reducing inflammation.
In addition, the SNS is also put on alert as part of the readiness drill. Norepinphrine output rises.
The sum of all three systems form a complex structure and are likely to be involved early on with AFS, though the degree in which each of the systems participate is highly variable and not known. Great overlap is expected, and that points to a well designed system with multiple control points. Successful deployment of the three systems of stress control in early stages of AFS returns the body to a normal state. Thus no symptoms are reported by those suffering from early AFS.

If stress is unrelenting, the HPA axis workload may be taxed to a point where dysregulation occurs. Cortisol output is compromised at the adrenal glands. Independently, excessive norepinephrine peripherally may overwhelm the SNS. The LC-NA system may be over-stimulated if stress is unresolved with constant brain arousal, giving a sense of being "wired" perhaps. All such dysfunctions lead to unpleasant symptoms. This point is likely reached when we enter Adrenal Exhaustion, where we see onset of signs of HPA axis dysregulation, including hypoglycemia and low blood pressure. Anxiety, brain fog, and a cognitive toll also increases as the LC-NA system stretches to the limit.
If left unresolved, further deterioration of the HPA axis dysregulation may arise, triggering other downstream hormonal axis dysregulation. The dysfunction of one organ system such as the adrenal gland can trigger a domino effect, leading to dysfunction of other organ systems. An example of this is the ovarian adrenal thyroid (OAT) axis imbalance in women and the adrenal thyroid (AT) axis imbalance in men that arise as Adrenal Exhaustion progresses. Three glands are involved. Started from cortisol dysregulation when the HPA axis is dysregulated, concurrent low cortisol, high estrogen, and low thyroid can appear as the condition worsens.
With the HPA dysregulated and OAT axis imbalanced, the sympathetic nervous system (SNS), already well on alert in earlier phases but not fully activated, is put in overdrive. Norepinephrine, the key hormone of the SNS, builds up. This can lead to heart palpitation, increased fatigue, and panic attacks. This hormone, normally playing a low-keyed homeostatic function, now goes in to be part of the emergency anti-stress team. It is now also responsible for some of the fight-or-flight responses to get the body ready for impending doom and for priming the body for action.
If stress is still unresolved after the above three systems are well deployed, the body, in its final attempt to overcome stress, activates the adrenomedullary hormonal system (AHS). Again, it is likely that this system is already on alert and may now be activated from earlier phases, perhaps less intense. As the body enters advanced phases of Adrenal Exhaustion, the AHS goes on full throttle. A larger amount of epinephrine and a smaller amount of norepinephrine are released from the adrenal medulla directly into the blood stream, flooding the body. This ensures that the vital organs, such as the brain and the heart, get the necessary blood flow and thus oxygen for survival. Other less important systems for survival sacrifice temporarily, such as reproduction and the gastric system. The AHS is designed to be a temporary anti-stress measure. Long term stimulation without adequate rest of the AHS may lead to dysfunction, putting the body into a state of disequilibrium. This frequently appears in sufferers who take metabolic stimulants to keep up their energy when faced with fatigue, not knowing that this strategy can be harmful to the AHS.
If not reversed on a timely basis, the overall anti-stress hormonal supply continues to deteriorate. Cortisol and other hormones become grossly dysregulated and severely depleted. This generally occurs in advanced phases of Adrenal Exhaustion. In its last ditch attempt to increase production, undesirable positive feedback loops may be activated. They are inherently unstable. Crashes are common. If not reversed, the body is inevitably down-regulated and draws nearer to failure with time, as it runs out of necessary basic reserve to prime the hormonal pump for basic function. To conserve energy, the body surrenders and turns to activating the remaining survival mode. This is accomplished by down-regulation of bodily functions. This effectively reduces energy output to a level close to a vegetative state as the final preparation for impending collapse. It comes as no surprise that those with advanced AFS are invariably incapacitated and bedridden.
From a neuroendocrinological perspective, it is clear that the body's multiple ant-stress pathways offer redundancy systems to handle stress in the vast majority of the time. It has ensured survival of our species for quite some time. What is confusing clinically in AFS is that these pathways can be activated a few at a time, or all at once, quickly or slowly, as the body sees appropriate for that moment in time. The body is truly in control, despite what appears to be total confusion from a conventional medical logic perspective.
To fully appreciate the body's heroic effort to rescue us from stress, it is important to understand first that our brain is in control of our body. What one person perceives as stressful may not be for another. Based on the perceived level of stress by the mind, the body automatically activates any or all of the anti-stress mechanisms in place.
In order for us to fully grasp the big picture, clinicians and sufferers alike need to take a step back, because it is easy to be confused from a closer or subjective perspective. The picture from afar is crystal-clear-that of a body in trouble, unable to maintain homeostasis and trying all its ways and means to recover on its own with the only method it knows-activating the anti-stress mechanisms in place. It is totally logical and systematic. Symptoms are simply the messages or signs the body sends us as warning of impending danger thereby alerting us to take appropriate action. Despite a losing battle, the mind is ultimately in charge through the body's various hormonal and anti-stress pathways. Successful recovery from AFS invariably needs to factor in the requirements of the mind as well as the body. A total body approach to recovery is crucial.
© 2007 Michael Lam, M.D. All Rights Reserved.