
 Aging happens to everyone, and so often do the chronic diseases that accompany it. Research shows the chronic diseases that afflict most, if not all, people over the age of 65 to have inflammation at their foundation. Most of these illnesses are handled by medications, but the patients suffer the side effects of those medications. These side effects often are as problematic as the illnesses themselves. Dealing more effectively with the inflammation that is the root cause of these illnesses is the goal. Natural inflammation remedies can help eliminate this root cause without the side effects of traditional medications.
Aging happens to everyone, and so often do the chronic diseases that accompany it. Research shows the chronic diseases that afflict most, if not all, people over the age of 65 to have inflammation at their foundation. Most of these illnesses are handled by medications, but the patients suffer the side effects of those medications. These side effects often are as problematic as the illnesses themselves. Dealing more effectively with the inflammation that is the root cause of these illnesses is the goal. Natural inflammation remedies can help eliminate this root cause without the side effects of traditional medications.
In order to fully grasp the impact of aging and the chronic diseases inflammation can trigger, it is helpful to know some demographics related to aging. The population of the United States is getting older as people live longer due to medical advances.
By the year 2030, the number of people in the U.S. age 50 and above is estimated to be 132 million. Those aged 65 to 74 in 2010 numbered 21.7 million. By 2030, that number is expected to increase to 38.6 million.
In 2030, one in five people will be 65 or older. One in eight will be 75 or older by 2040.
This aging of America will bring at least a 10% increase in the cost of health care. A large part of this increase will be due to chronic diseases. By age 65, most people will have two or more chronic illnesses. In the last 10-15 years of life, people can expect to spend 70% of the health care costs for their lifetime.
And nearly all of these chronic diseases have inflammation at their foundation. A number of factors can bring on inflammation. Among these are inactivity, obesity, and the effects of aging.
The aim of medicine in the care of the aging population must be complete control of inflammation. Natural inflammation remedies thus gain importance over our lifetimes.
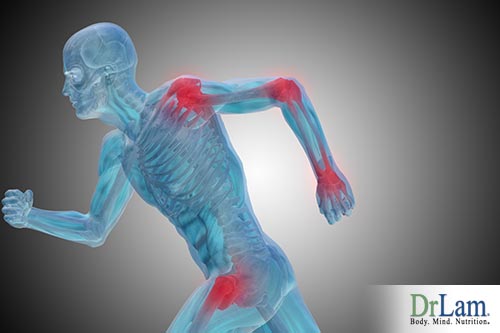
Inflammation serves a purpose in your body. Normally, inflammation arises as a result of an insult to your body. Injury due to accident, illnesses, or surgical procedure can all lead to inflammation. In addition, stress can bring on inflammation.
In the latter case, there is a connection between Adrenal Fatigue Syndrome (AFS) and inflammation. Both are a result of stress of some kind on the body. Each can cause the other.
When a stressful event occurs, the body releases certain biochemical messengers. Among them are lipid mediators, cytokines, and chemokines. These messenger chemicals signal the beginning of a series of events that works to deal with the insult to the body.
The goal of this cascade of bodily mechanisms is to heal. First, blood vessels dilate to increase blood flow. Then, white blood cells stream to the site of the injury, whether it is physical or psychological in nature. With this healing process comes some discomfort. Swelling, redness, warmth, and elevated temperature are the four cardinal signs of inflammation. It is an adaptive response that serves us in dealing with acute attacks on our health.
All of this is associated with acute inflammation. When inflammation is in the acute phase, it’s a self-limiting condition. Once the injury or other insult is over, inflammation naturally ceases. A release of anti-inflammatory messenger chemicals stops the process.
 Recent research has pinpointed two distinct phases of the inflammatory process. These phases must balance in order for inflammation to carry out its naturally protective role.
Recent research has pinpointed two distinct phases of the inflammatory process. These phases must balance in order for inflammation to carry out its naturally protective role.
The initiation phase is the activation of the inflammatory process, as mentioned above.
The resolution phase is the part of the process in which inflammation is neutralized. It releases its own set of chemicals for the body to use. These chemicals are lipid mediators called SPMs, or specialized pro-resolving lipid mediators.
There are four families of SPMs: resolvins, protectins, maresins, and lipoxins.
The SPMs’ job is six-fold:
If these SPMs aren’t present in sufficient quantity or don’t do their job adequately, the stage is then set for chronic inflammation to occur.
Traditional medicine focuses on stopping inflammation once it is already in the initiation phase. This contributes unwittingly to the presence of chronic inflammation. The medications physicians use to combat inflammation only cover up the symptoms. These only give temporary relief from the pain and tenderness that often accompanies inflammation. These medications impede the resolution phase of the inflammatory process. They prevent the equally important cleaning up of residue from the injury or insult that started the inflammation. In addition, medications stop the release of the chemical messengers that signal anti-inflammatory processes to begin.
If the inflammatory process continues beyond the bounds of normal functioning, an ongoing, low-grade process of inflammation begins. Inflammation becomes chronic. This response bombards your system with more and more inflammation-related chemicals. Over time, this chronic inflammation makes itself known physically, through, for example, the swollen joints of arthritis, the diarrhea and bleeding of inflammatory bowel disease, or the restricted breathing of asthma.
With the passage of more time and the advancing of age, a ‘silent’ inflammatory process can lead to more destructive illnesses. These include heart disease, diabetes, macular degeneration, autoimmune diseases, dementia, obesity, and even cancer.
This chronic, low-level inflammation is also known as ‘inflammaging’. Due to its involvement in the development and continuance of these chronic diseases, inflammation is considered a significant risk factor for both morbidity and mortality among the aging population.
Considering this serious risk, the ability to successfully reduce or eliminate the effects of inflammation gain even more importance. Thus, finding natural inflammation remedies assumes a greater importance as well. Natural inflammation remedies often have fewer side effects than medical remedies. This is a major consideration for older people due to quality of life issues and the number of chronic illnesses many people have.
 Exactly how inflaming begins, and its specific role in the development of chronic illness, is not clearly known. It is necessary, therefore, to learn pathways of control for this process across more than one system to understand how inflaming can be remediated in older people. Developing and examining natural inflammation remedies is one important pathway for this understanding. Learning the effectiveness of natural inflammation remedies and how they modulate inflammation is important for the aging population.
Exactly how inflaming begins, and its specific role in the development of chronic illness, is not clearly known. It is necessary, therefore, to learn pathways of control for this process across more than one system to understand how inflaming can be remediated in older people. Developing and examining natural inflammation remedies is one important pathway for this understanding. Learning the effectiveness of natural inflammation remedies and how they modulate inflammation is important for the aging population.
There is significant evidence that this kind of low-grade inflammation, shown by biomarkers such as C-reactive protein and interleukin-6 (IL-6), may also be a means of predicting how people age.
There appear to be several mechanisms by which chronic inflammation works as inflammaging. One mechanism may be through infiltrating leukocytes. These produce reactive molecules whose purpose is to kill pathogens. However, their continued presence may damage the structure and cells of tissues.
Another possible mechanism may be through cytokines produced by active immune cells or damaged nonimmune cells. These cytokines are supposed to increase or modulate the inflammatory response. However, they may alter the phenotypes of other, nearby cells and decrease the normal functioning of tissues. Many tissues in older people may already be in a state of chronic inflammation without overt infection.
Yet another possible mechanism of inflammaging may be anabolic signaling interference. IL-6 and tumor necrosis factor alpha interfere with insulin, insulin-like growth factor-1, and erythropoietin signaling and protein synthesis. This occurs after a meal or after exercise.
Where inflammaging comes from is another area of conjecture. One possible origin could be the buildup of damaged molecules and cells that comes with age. This buildup is typically due to continued production and imperfect elimination of this type of debris. Debris like this and debris left over from insult or injury to your body may signal the immune system to activate because it can mimic bacteria. Inflammation is a product of immune system activation.
Another possible source could be microbes from your oral or gut microbiota that leak into your system and get carried around your body by blood circulation. Your ability to keep these microbes at bay deteriorates with age, resulting in low-grade inflammation.
An alternate explanation may have to do with a change in gut bacteria as we age, resulting in an inflammatory response. Mitochondria have a large role in controlling inflammation and activating the Nlrp3 inflammasome. This inflammasome is made up of multiple proteins. It can activate pro-caspase-1 because of danger to cells and leads to processing and secretion of proinflammatory cytokines IL-1beta and IL-18.
Aging cells tend to build up to high levels in adipose tissue, or fat. This is important because of the increasing incidence of obesity among all ages in the population. Obese individuals have high levels of visceral fat. This fat accumulation typically is rich in inflammatory cytokines. It is, therefore, a reservoir of pro-inflammatory chemical messengers. Obesity increases the likelihood of inflammation.
Many age-related chronic diseases share similar cytokines, molecular pathways, effector cells, and tissue responses with chronic inflammation. IL-6 may be the cytokine most commonly shared between inflammation and age-related diseases. It is a typical biomarker of inflammation status and chronic morbidity. IL-1beta and tumor necrosis factor-1 are two other typical biomarkers shared between inflammation and age-related diseases. Let’s take a look at some of these conditions.
 There is a growing body of research that indicates a relatively strong connection between chronic inflammation and metabolic syndrome. Chronic, low-grade inflammation appears to be a possible triggering event for metabolic syndrome.
There is a growing body of research that indicates a relatively strong connection between chronic inflammation and metabolic syndrome. Chronic, low-grade inflammation appears to be a possible triggering event for metabolic syndrome.
The typical features of metabolic syndrome include abdominal obesity, insulin resistance, high blood pressure, and dyslipidemia (high triglycerides and low HDL cholesterol). This condition may be as prevalent as occurring in one in four Americans. This level of prevalence necessitates finding natural inflammation remedies that significantly reduce it.
Metabolic syndrome appears to be a strong risk factor for the development of atherosclerosis. It is also prognostic of possible cardiac events.
One way chronic inflammation may trigger metabolic syndrome is through the hypersecretion of cytokines due to overeating, sedentary lifestyle, and aging. This leads to insulin resistance and the eventual development of diabetes in individuals predisposed to it. Resistance to insulin, with its anti-inflammatory properties, may result in increased proinflammatory cytokines in circulation, leading to chronic low-grade inflammation.
Another possible explanation for the connection between metabolic syndrome and inflammation has to do with adipose tissue in obese individuals secreting adipose tissue-specific enriched hormones called adipokines. These adipokines may interfere with the balance between anti-inflammatory and proinflammatory factors in the body.
In any case, the proinflammatory state that comes with metabolic syndrome affects both insulin resistance and endothelial dysfunction. This indicates the relationship between inflammation and metabolic syndrome is damaging to vascular functions.
Elevated C-reactive protein levels are implicated in metabolic syndrome and major coronary events. The higher levels of adipose tissue in obese individuals and subsequent release of more cytokines may lead to greater production of C-reactive proteins by the liver.
Adrenal Fatigue Syndrome and inflammation go hand in hand. Each one can be a causative factor for the other, and each one can be caused by stress.
Anytime stress impacts your body, the same process is set in motion. The hypothalamic-pituitary-adrenal (HPA) axis is activated. The adrenal glands respond by secreting cortisol, the stress-fighting hormone. Normally, the cortisol manages the effects of stress and the body returns to a resting state. If stress continues though, pressure is placed on the adrenals to continue secreting cortisol. At some point, adrenal fatigue sets in, and cortisol secretion drops as the adrenals become exhausted.
With adrenal exhaustion, symptoms of low cortisol begin. Once this advanced stage of AFS is reached, symptoms appear like reactive hypoglycemia, chronic inflammation, menstrual problems, thyroid dysfunction, and low blood pressure.
Unrelenting fatigue is a major factor in the condition. You might sleep well all night but wake in the morning feeling as tired as if you didn’t sleep at all. On the other hand, you may suffer from insomnia and genuinely not be able to sleep.
Anxiety and depression also can be part of advanced AFS. The anxiety and fatigue combination leads to a person becoming ‘wired and tired’. At this time, the body has few resources left to deal with inflammation. And the inflammation grows rapidly under the conditions of AFS. Increasing inflammation leads to many different kinds of chronic disease conditions. None of the symptoms experienced in AFS can specifically indicate AFS; it is the collection of symptoms that lead to the assessment of AFS.
Traditionally trained physicians tend to assess and remediate diseases, including AFS, from the standpoint of focusing on individual symptoms and organs. For conditions like AFS, where the symptoms are sometimes non-specific, this is not an effective method. Considering organ systems in interrelationship with each other brings a more comprehensive way of dealing with illness. Using natural inflammation remedies are always considered the first approach.
 The NEM model of stress response is such a comprehensive method. This model, a natural medicine approach using natural inflammation remedies, studies the way several organ systems interact in the presence of AFS symptoms.
The NEM model of stress response is such a comprehensive method. This model, a natural medicine approach using natural inflammation remedies, studies the way several organ systems interact in the presence of AFS symptoms.
Inflammation is one of the six main circuits in how your body deals with stress. The primary organ systems involved with inflammation are the immune system, the gastrointestinal system, and the gut microbiome. An imbalanced gut microbiome may allow leakage of bacteria, which leads to increased inflammation.
Inflammation is a key aspect of the body’s response to stress. It is tied closely to the ability to detox naturally. When our detox ability is decreased, toxins build up, leading to more inflammation. The body’s inability to detox also leads to oxidative stress, which causes cell damage and death, adding to the debris that can’t be eliminated and increasing inflammation.
Using this NEM model allows a healthcare professional to see the entire process of disease and dysfunction across systems in order to restore a healthy balance. It allows the professional to see underlying causes and triggers that operate in the various systems, and it eventually enables discovery of the root cause of the disease condition.
The detrimental health effects of chronic inflammation have been shown repeatedly in research and clinical practice. The importance of reducing or eliminating chronic inflammation can’t be overstated. Natural inflammation remedies frequently appear to be the most appropriate way to alleviate the effects of chronic inflammation.
A naturally produced protein, tristetraprolin (TTP), appears to significantly reduce or eliminate the effects of inflammation, according to research conducted at the National Institutes of Health. Producing elevated levels of TTP in humans may be an effective way to deal with chronic diseases such as rheumatoid arthritis and multiple sclerosis. The beneficial effect of TTP is achieved by binding to messenger molecules that encode cytokines. TTP decreases the level of cytokines, resulting in lowered inflammation.
Other new research has investigated the effect of too little or too much sleep on inflammation. This research found inflammatory markers such as C-reactive protein and IL-6 were present in people who slept too little and too much. This suggests both too little and too much sleep may act as triggers for inflammation. In normal aging and in AFS, sleep disturbances are common. The CDC has labeled insufficient sleep to be a public health epidemic. However, exactly how sleep and inflammation are linked is not known at this time due to variability of research results.
A significant body of research exists looking into how dietary factors affect inflammation markers. A number of clinical trials have shown losing weight to significantly reduce biomarkers such as C-reactive protein and IL-6. Other, more limited studies have suggested other dietary factors reduce these biomarkers of inflammation as well.
 Dietary and weight control factors appear to be the crucial elements in preventing chronic inflammatory conditions. Obesity contributes to the elevation of C-reactive proteins, and weight loss decreases this same biomarker.
Dietary and weight control factors appear to be the crucial elements in preventing chronic inflammatory conditions. Obesity contributes to the elevation of C-reactive proteins, and weight loss decreases this same biomarker.
It appears that reducing saturated and trans fats also reduces inflammation. These fats are proinflammatory. A diet high in monounsaturated fats, such as the Mediterranean diet, may help reduce inflammation.
Low cholesterol diets may also aid in reducing inflammation. One eight-week clinical study showed a diet low in cholesterol and saturated fat was linked to lower inflammation, as evidenced by lower levels of C-reactive proteins.
High blood sugar levels can lead to inflammation as well. The mechanism involved appears to be the production of free radicals and proinflammatory cytokines. Consuming high-glycemic index foods leads to higher and more rapid increases in blood glucose levels. This stimulates the pancreas to secrete more insulin, potentially leading to hypoglycemia.
Especially in obese individuals, consuming a low glycemic index diet leads to significantly lower levels of C-reactive protein. This type of diet also appears to lead to lower levels of proinflammatory cytokines.
 Hippocrates, the father of modern medicine, reportedly said, “Let food be your medicine.” This appears to be very applicable in the case of inflammation and its effects. Nutrition therapy is an emerging area of investigation as a way of dealing with inflammation. It shows that food can be excellent natural inflammation remedies.
Hippocrates, the father of modern medicine, reportedly said, “Let food be your medicine.” This appears to be very applicable in the case of inflammation and its effects. Nutrition therapy is an emerging area of investigation as a way of dealing with inflammation. It shows that food can be excellent natural inflammation remedies.
Evidence strongly suggests eating foods consisting of plants, lean protein, and healthy fats will speed the resolution of inflammation. Consuming supplements also is a good step in helping the effects of inflammation. However, there is no specific combination of supplements suggested for dealing with inflammation. The use of these natural inflammation remedies should be individualized.
Obesity, especially abdominal obesity, has been clearly connected to low-grade inflammation. Many chronic illnesses have also been linked to obesity, the same ones that have inflammation at their foundation.
Adipokines, a form of biologically active molecule, are produced by adipose tissue that is involved in abdominal obesity. These adipokines include hormones, proteins, cytokines, and macrophages. Adipokines have multiple health effects, including regulating food intake, the use of energy, and the metabolism of glucose and fatty acids.
Proinflammatory cytokines TNF-alpha, IL-6, and IL-1beta are secreted due to the influence of the macrophages contained in adipose tissue. These cytokines stimulate the liver to produce increased amounts of C-reactive proteins, leading to increased inflammation.
Since foods have a very significant effect on inflammation, it’s important to know which of these foods have a proinflammatory effect. These foods should be avoided as part of a natural inflammation remediation plan.
Increased caloric intake leads to increased adipose tissue formation. This increases the risk of obesity and the likelihood of developing chronic diseases such as diabetes or metabolic syndrome.
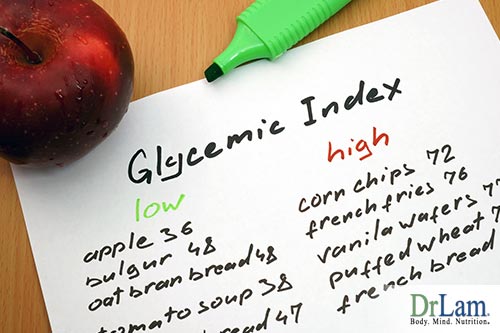 Consuming high levels of carbohydrates also contributes to chronic diseases like obesity, metabolic syndrome, and type 2 diabetes. These carbohydrates are usually from foods low in fiber, high in sugars and starches, and high on the glycemic index.
Consuming high levels of carbohydrates also contributes to chronic diseases like obesity, metabolic syndrome, and type 2 diabetes. These carbohydrates are usually from foods low in fiber, high in sugars and starches, and high on the glycemic index.
Consuming trans fatty acids is a significant risk factor for sudden cardiac arrest. These trans fatty acids lead to an inflammatory response in cardiac tissues because of effects on cell membranes.
Saturated fatty acids have been shown to play a part in inflammation through increased macrophage production, leading to secretion of the pro-inflammatory cytokines TNF-alpha, IL-6, and IL-8. Research has shown that mice fed a diet with 12% saturated fat, which is the average amount of these fats in the typical American diet, resulted in increased body fat and higher levels of proinflammatory cytokines.
Over the last several decades, the amount of omega-6 polyunsaturated oils in the American diet has steadily risen. This increase correlates with an increase in the risk of chronic inflammatory diseases, such as cardiovascular diseases and rheumatoid arthritis. Research suggests the best ratio of omega-6 to omega-3 fatty acids is 4:1. However, the increased consumption of omega-6 fatty acids has changed this ratio to as much as 20:1.
Omega-6 fatty acids are precursors to proinflammatory signaling molecules active in the inflammation process. Through chemical conversion, these molecules tend to increase proinflammatory cytokine production.
Foods that decrease inflammation are also an important aspect of natural inflammation remedies.
Fresh fruits and vegetables that are brightly colored fall into the anti-inflammatory category. They are possibly the most effective anti-inflammatory foods. They contain magnesium and antioxidants, along with carotenoids and lycopene.
Grapes and berries contain resveratrol. This phytochemical appears to fight heart disease. It also helps lower inflammation.
Vegetables like artichokes and garlic contain fructooligosaccharides. These are complex sugars that are not digested by the human gut, decreasing the absorption of calories and leading to fewer spikes in blood sugar levels. They also feed beneficial gut bacteria, promoting and maintaining a healthy gut.
Avocados are a great way to remedy inflammation naturally because of the high level of nutrients they contain. Numerous studies show the consumption of avocados leads to decreased inflammation, balanced blood sugar levels, lowered cholesterol, and reduced arthritis pain.
Nuts and seeds contain protein, fiber, phytonutrients, and omega-3 fatty acids. Snacking on them throughout the day helps keep blood sugar and insulin levels stable and provides energy. Walnuts especially contain a certain phytochemical that is hard to find anywhere else.
Olive oil contains high levels of polyphenols. These are powerful anti-inflammatory compounds and important natural inflammation remedies.
Whole grain foods, such as oatmeal, which are high in fiber, phytochemicals, vitamins, and minerals, may decrease inflammation found in metabolic syndrome, diabetes, and cardiovascular disease.
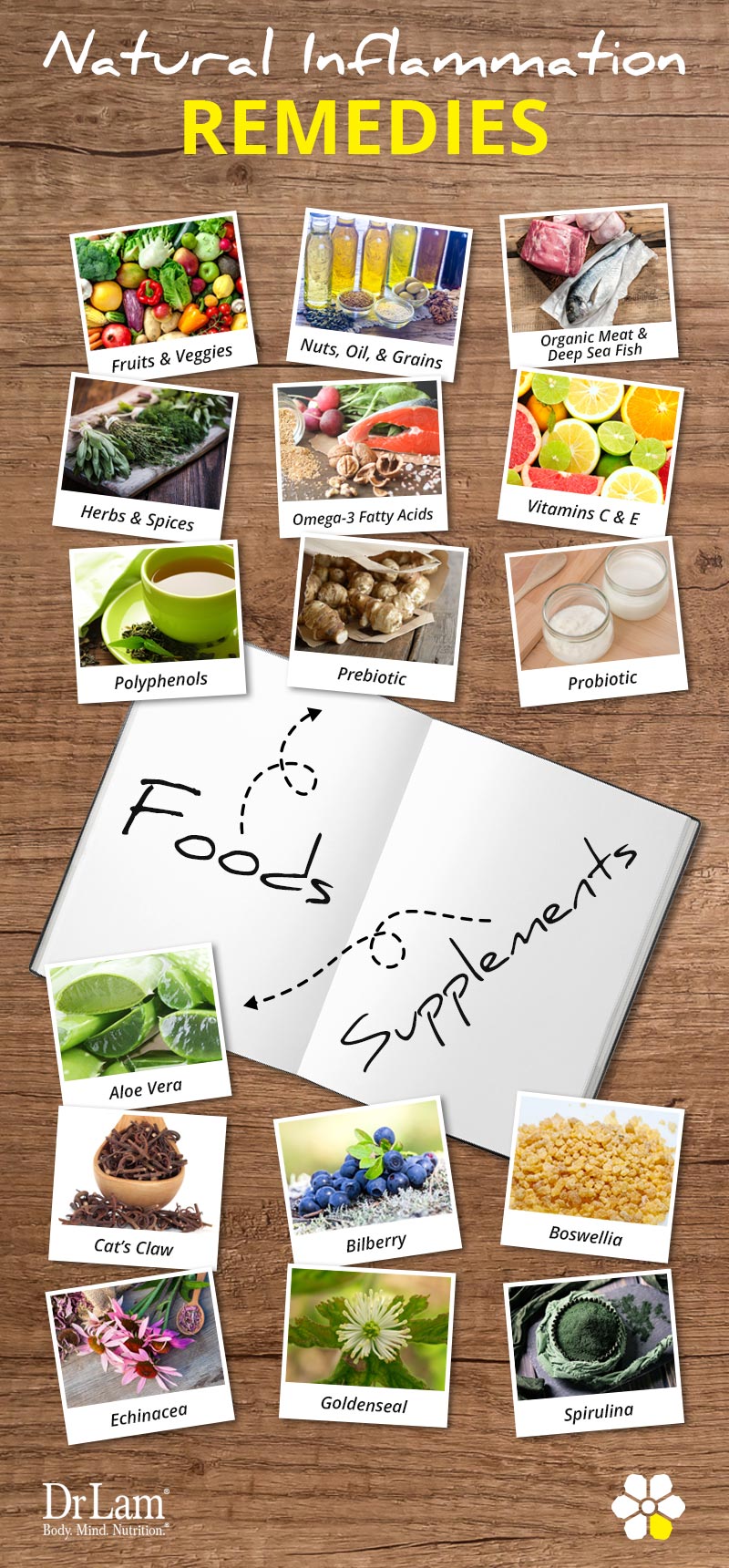
Organic meats are healthier overall than meats from factory farmed animals. Their nutritional values are higher. They also have higher levels of omega-3 fatty acids and lower omega-6 fatty acid levels.
Cold water fish such as salmon, anchovies, and sardines are high in polyunsaturated omega-3 fatty acids. These fatty acids provide a wide range of health benefits, such as alleviating autoimmune conditions and reducing inflammation. These foods are very good natural inflammation remedies.
 A large number of herbs and spices have mixtures of vitamins and phytonutrients that fight inflammation and add to overall health. They are a great source of natural inflammation remedies. Oregano, lavender, rosemary, cinnamon, and turmeric contribute to overall health and decrease inflammation.
A large number of herbs and spices have mixtures of vitamins and phytonutrients that fight inflammation and add to overall health. They are a great source of natural inflammation remedies. Oregano, lavender, rosemary, cinnamon, and turmeric contribute to overall health and decrease inflammation.
Ginger has been used in many cultures because of its anti-inflammatory properties. Only recently has modern medicine caught up with this use of ginger. It has been shown to inhibit prostaglandin synthesis and leukotriene biosynthesis. Both of these compounds are present in the inflammation process.
The spice turmeric is high in curcumin. Studies have shown curcumin to be more effective than cortisol, the anti-stress hormone, in combating inflammation.
It has been suggested that omega-3 fatty acids are beneficial in reducing levels of inflammation. They contain higher levels of alpha-linolenic acid (ALA), eicosapentaenoic acid (EPA), and docosahexaenoic acid (DHA) which may decrease biomarkers of inflammation. EPA and DHA have been shown to decrease the production of proinflammatory eicosanoids and increase the synthesis of anti-inflammatory eicosanoids from arachidonic acid. Omega-3 fatty acids also decrease the production of the proinflammatory cytokines TNF-alpha, IL-1 beta, IL-6, and IL-8. Resolvins are also produced from EPA and DHA. These resolvins inhibit proinflammatory signaling.
In addition to cold water fish, omega-3 fatty acids can also be found in flaxseeds, chia seeds, walnuts, and canola oil. ALA is the fatty acid that is gained from these foods. It has been shown to be somewhat effective in decreasing inflammation, but EPA and DHA are more effective.
Ascorbic acid (vitamin C) from foods is a powerful antioxidant that stimulates the activity of natural killer lymphocytes in the innate immune response. It also reduces tissue damage at inflammation sites.
Vitamin E from foods like seeds, nuts, and vegetable oils is present in the form of gamma-tocopherol. This chemical decreases proinflammatory NF-kB and TNF-alpha activity. Vitamin E in the form of alpha-tocopherol has the ability to scavenge free radicals and prevent lipid oxidation.
Some studies investigating the relationship between vitamin E and measures of inflammation have yielded mixed results. It’s possible this occurred due to these studies instead examining alpha-tocopherol, which decreases the levels of gamma-tocopherol and reduces its anti-inflammatory properties. These alpha-tocopherols were also from supplements and not food-based.
Polyphenols are found in foods like fruits, vegetables, grains, chocolate, coffee, and tea. These substances have powerful anti-inflammatory properties and are good natural inflammation remedies. Research and clinical studies suggest polyphenols prevent free radical formation, decrease proinflammatory cytokine production, and block proinflammatory signaling systems. However, the true effects of dietary polyphenols on inflammation require further study due to wide variations in the polyphenol content in food.
 Prebiotics are nondigestible and nonabsorbable substances that ferment in the gut of humans. This fermentation promotes the growth of beneficial microflora in the gut, leading to improved gut health. Foods like chicory, Jerusalem artichokes, and onions contain prebiotics. These foods are good natural inflammation remedies.
Prebiotics are nondigestible and nonabsorbable substances that ferment in the gut of humans. This fermentation promotes the growth of beneficial microflora in the gut, leading to improved gut health. Foods like chicory, Jerusalem artichokes, and onions contain prebiotics. These foods are good natural inflammation remedies.
Probiotics, another food source of natural inflammation remedies, are bacteria. These bacteria are a normal part of your gut flora and ferment lactose. Cultured dairy foods like yogurt and kefir contain probiotics.
Both prebiotics and probiotics lower the activity of proinflammatory cytokines and NF-kB while increasing anti-inflammatory TGF-beta in the gut mucosa. However, mixed results have been found in research studies regarding their effects on inflammation in Crohn’s disease and ulcerative colitis.
Several supplements can also be beneficial in reducing or avoiding inflammation.
Aloe vera has been used for many purposes, and its effects on inflammation are noteworthy. Two substances, campesterol and bradykinin, are the active substances in aloe that fight inflammation. Campesterol has been shown to lower cholesterol and actively decrease inflammation. It also helps generate new cells to repair the damage done by inflammation. Bradykinin helps increase blood flow by dilating blood vessels.
However, some cautions are in order regarding aloe supplements. If you’re pregnant or breastfeeding, avoid taking aloe by mouth. Aloe supplements may lower blood sugar, so hypoglycemia is a possibility. Consult with your healthcare professional before taking it if you have diabetes. Aloe latex is a bowel irritant. Don’t take it if you have Crohn’s disease or any other GI illness. High doses of aloe latex have been linked to kidney failure.
The flavonoids found in bilberry have been shown to be effective natural inflammation remedies. Studies conducted in Finland show consuming bilberries (similar to blueberries) significantly reduced the biomarkers associated with metabolic syndrome. The mechanism for this reduction appears to be the polyphenols, especially anthocyanins, contained in bilberries.
Be certain to discuss the use of bilberries with your healthcare professional if you know you are allergic to any part of bilberry. Some medications interact with bilberries. If you’re planning to become pregnant, are pregnant, or are breastfeeding, be sure to consult with your healthcare professional before using them. Also, a consultation is needed if you’re taking any medications, herbal preparations, or dietary supplements. If you’re diabetic, this consultation is a necessity.
Boswellia is said to have a beneficial effect on inflammation. This supplement has only recently been researched as a natural remedy for inflammation, but it has a long history of use throughout the world to reduce the effects of arthritis. Used in combination with turmeric, it appears to have a beneficial effect on the inflammatory aspects of arthritis. Very few side effects have been reported with Boswellia.
Cat’s claw has been reported effective for reducing inflammation and boosting your immune system. It has been used for many years in South America as a way of dealing with ulcers, inflammation, dysentery, and fevers. It may stimulate the immune system and has antioxidant properties.
Cat’s claw appears to have few side effects other than transitory GI issues that go away with continued use. However, cat’s claw should be avoided by women who are pregnant or breastfeeding and by people with autoimmune diseases, TB, or who have had transplants. If you have low blood pressure or leukemia, avoid cat’s claw. If you have kidney or liver disease, consult with your healthcare professional before taking cat’s claw.
 Echinacea has been reported to have anti-inflammatory properties, as well as immune stimulatory effects. Laboratory and animal studies suggest that echinacea has properties that boost immune function and fight inflammation.
Echinacea has been reported to have anti-inflammatory properties, as well as immune stimulatory effects. Laboratory and animal studies suggest that echinacea has properties that boost immune function and fight inflammation.
Side effects include a wide range of possible allergic reactions. If you have asthma and allergies, you’re at an increased risk of developing an allergic reaction. Upset stomach, nausea, and dizziness have been reported. If you’re taking any prescription medications, be sure to consult with your healthcare professional before taking echinacea.
Goldenseal has been said to reduce inflammation. It stimulates bile flow and digestive enzymes regulating liver and spleen functions. It contains numerous vitamins, minerals, and other nutrients. Goldenseal has antibacterial properties, likely due to berberine. This substance allows it to decrease inflammation.
If you are pregnant, likely to become pregnant, or breastfeeding, avoid taking goldenseal.
Spirulina, a ‘superfood’ in the blue-green microalgae family, has proven anti-inflammatory properties. Its antioxidant and anti-inflammatory properties have been investigated in several research projects. Gamma-linolenic acid (GLA) is very high in this food. GLA is a precursor to prostaglandins, leukotrienes, and thromboxanes, all of which are chemicals that modulate inflammatory and immune reactions.
A low-grade fever may come with this supplement, along with dizziness and nausea. Taking spirulina may lead to thirst and constipation. For this reason, be sure to drink plenty of water when taking this supplement. Stomach ache may also be experienced.
It is evident from research and clinical experience that inflammation is a serious health issue. With inflammation, aging increases in both rate and severity. The importance of this comes to the fore when the number of people over 65 years of age in the U.S. is considered, along with the rising cost of healthcare for this population. Taking measures to reduce or eliminate inflammation can have a big impact on long-term quality of life. Natural inflammation remedies may be the best way to attack this problem.