
 Can what you eat influence chronic pain and illnesses? According to current research, the answer is overwhelmingly yes. We get from our bodies what we put into them. Inflammation plays a major role in your overall health, and what foods you eat can have a big influence on inflammation. There are some inflammatory foods that should be eliminated from your diet altogether, while other foods can have important anti-inflammatory properties. Natural medicine practitioners have known for years what is now seen as the nutritional foundation of chronic illness.
Can what you eat influence chronic pain and illnesses? According to current research, the answer is overwhelmingly yes. We get from our bodies what we put into them. Inflammation plays a major role in your overall health, and what foods you eat can have a big influence on inflammation. There are some inflammatory foods that should be eliminated from your diet altogether, while other foods can have important anti-inflammatory properties. Natural medicine practitioners have known for years what is now seen as the nutritional foundation of chronic illness.
The idea that our bodies can heal themselves if given the right foods has been around since Hippocrates, the father of modern medicine. However, much of the typical medical advice we are given neglects this knowledge.
When considering the relationship between our food choices, pain, and chronic illnesses, it is important to keep in mind the body is made up of interrelated organ systems. These organ systems are affected by each other. What happens in one system also has effects in others.
The NeuroEndoMetabolic (NEM) Stress Response model describes the relationship among organ systems and how the entire body responds to stressors of any kind. Practitioners trained in this comprehensive approach look at the interaction between factors in the environment and all organ systems. This allows for the entire presentation of your symptoms to be considered and approached from a systems viewpoint that helps get to the root cause of the issue.
This holistic approach strives to understand inflammation from its beginnings in the metabolic process through to its effects on other organ systems. If inflammation is allowed to run rampant, its effects can lead to increasingly serious illnesses. The NEM approach allows adequate and effective interventions in multiple organ systems to control inflammation.
Inflammation is the body’s natural response to invasion by foreign substances such as bacteria and viruses. It is part of the complex biological process by which the body fights invaders, carries them out, and repairs whatever damage has been caused. If inflammation were not part of this process, infections and wounds would likely never heal.
 A normal part of inflammation is discomfort at the site of the injury or infection. This type of pain is a by-product of the cascade of molecular and cellular changes that take place when inflammation is at work. The physiological symptoms of pain, redness, swelling, and heat are indicators that inflammation is doing its job.
A normal part of inflammation is discomfort at the site of the injury or infection. This type of pain is a by-product of the cascade of molecular and cellular changes that take place when inflammation is at work. The physiological symptoms of pain, redness, swelling, and heat are indicators that inflammation is doing its job.
In cases of acute inflammation, which is stimulated for a short time to deal with immediate injury or stress, once the healing process is complete, the inflammation subsides. Acute inflammation is tightly controlled by the body. Cortisol, the stress-fighting hormone, is in control of turning off acute inflammation when it is time.
Although the effects of inflammation are uncomfortable, the body can handle them up to a point. Injury leads to an inflammatory response, which deals with and heals the damage from whatever caused the injury, and then cortisol turns off the inflammatory response. This process is a healthy one.
However, there are cases where low-level inflammation endures. It can remain in the body for months or years without an obvious injury or infection ever appearing. This type of inflammation is responsible for much of the damage done to the body, eventually resulting in chronic illnesses and the resulting pain.
Emotional stress is one precipitating factor leading to chronic inflammation. With this kind of stress, your body is subjected to a continuous inflammatory response, leading to imbalance. This leaves you more open to infections, pain, and chronic disease. The longer you have this kind of sub-clinical, chronic inflammation, the more severe the symptoms of any chronic illness will be.
If this chronic inflammation is connected to a specific chronic illness, it will be localized. If the arteries are inflamed, for instance, heart disease will result. If certain areas of the brain are inflamed, Alzheimer’s disease will be most likely. If the pancreas is the target of the inflammation, diabetes results.
Inflammatory foods serve to prolong and worsen this chronic inflammation process. Some foods and environmental toxins tend to cause inflammation in many areas of your body. This kind of inflammation can affect your mental abilities, your overall health, and even how long you live.
Mild allergies to inflammatory foods may have only subtle symptoms, but they can cause long-term inflammation. Diet and lifestyle issues also bring about this kind of inflammation. The modern American diet involves the ingestion of more and more processed foods loaded with sugars and fats, along with a much more sedentary lifestyle, that sets the stage for inflammation. Increasing levels of environmental toxins, especially preservatives in packaged foods, additives in water, and toxic metals have been linked through research to chronic conditions like fibromyalgia.
All of these factors impact your gut microbiota causing dysbiosis, or imbalance, in the flora living there. One of the results of this dysbiosis is leaky gut, a situation in which the cells in the lining of your gut loosen their normally tight junctions and allow hard-to-digest foods, bacteria, viruses, and even fecal material to slip through and enter your bloodstream. This triggers an immune response to this foreign matter, which ultimately results in inflammation.
One of the major factors that leads to chronic inflammation is stress. The daily, unrelenting stress we all feel can lead to increased levels of cortisol and hormonal imbalances, eventually leaving the body unable to deal with inflammation. A common, but overlooked condition that results in chronic inflammation is Adrenal Fatigue Syndrome (AFS).
 Adrenal fatigue is the body’s natural response to long-term or very severe stress. This results in a reduction in the adrenal glands’ ability to secrete cortisol, the stress-fighting hormone. When this happens, an increase in inflammation is one result.
Adrenal fatigue is the body’s natural response to long-term or very severe stress. This results in a reduction in the adrenal glands’ ability to secrete cortisol, the stress-fighting hormone. When this happens, an increase in inflammation is one result.
When you are under stress, regardless of the source, the hypothalamic-pituitary-adrenal (HPA) axis is activated. A cascade of hormones results, with the adrenal glands ultimately secreting cortisol to fight the effects of stress. In normal situations, as soon as the stress is over, the adrenals return to a state of rest.
However, in our stress-filled world, stress often continues. This puts a significant burden on the adrenals to continue secreting cortisol. At some point, adrenal fatigue sets in, and the adrenals no longer have the ability to secrete this necessary hormone. Then, due to several factors, inflammation increases, leading to symptoms that are sometimes vague in the beginning. However, these symptoms accumulate, resulting in serious physical and emotional issues. In stage four AFS, some become bed-ridden due to the severity of symptoms.
Inability to think clearly, depression, anxiety, and weight gain around the middle of the body are some of the common symptoms of AFS.
Recent research has shown a definite connection between inflammation, food, and stress. Numerous studies have detailed the links between food choices and inflammation. The key pathways include oxidative stress, the activation of transcription factor nuclear factor kappa B (NF-kB), and proinflammatory cytokine production. Stress and depression also influence inflammation through these pathways.
 The relationships between diet, stress, depression, and inflammation are complex. The choices you make regarding foods are influenced by stress. You’re more likely to choose inflammatory foods when stressed rather than nutritional foods. These are the so-called “comfort foods” people tend to crave. Also, when you’re under stress, your metabolic response to these unhealthy inflammatory foods becomes more maladaptive. Plus, both mood and proinflammatory responses to stress are affected by your dietary choices.
The relationships between diet, stress, depression, and inflammation are complex. The choices you make regarding foods are influenced by stress. You’re more likely to choose inflammatory foods when stressed rather than nutritional foods. These are the so-called “comfort foods” people tend to crave. Also, when you’re under stress, your metabolic response to these unhealthy inflammatory foods becomes more maladaptive. Plus, both mood and proinflammatory responses to stress are affected by your dietary choices.
And then there is the interplay between vagal nerve stimulation, and the metabolic responses to foods, stress, and depression. Since the vagus nerve is directly involved in the entire process of digestion, absorption, and metabolism of foods, it can significantly affect both inflammation and the metabolic response of your body to food. Abundant documentation shows the negative effects of depression and stress on the vagal nerve, leading to considerable activity between the gut and brain.
This type of interaction is readily shown by the example of Omega-3 fatty acids. An increase in consumption of this beneficial fatty acid causes a boost in mood and activation of the vagus nerve. This serves to decrease NF-kB activation and decreases inflammation due to stress.
 The foods you eat are your body’s medicine. What you consume is what your body has to work and play on. It even makes a significant difference in how well you heal and in how well any medications, even pain medications, work in your body. This is why it is important to avoid inflammatory foods.
The foods you eat are your body’s medicine. What you consume is what your body has to work and play on. It even makes a significant difference in how well you heal and in how well any medications, even pain medications, work in your body. This is why it is important to avoid inflammatory foods.
Good food choices build up your body, give it sufficient nutrients to work with, and hasten the healing process. Good foods will keep your gut microbiome performing its functions properly, absorbing the nutrients in your food more efficiently, and working more effectively to rid your body of toxins.
On the other hand, inflammatory foods will do just the opposite. Research has shown a very strong link between what you eat, inflammation, and the experience of pain. These inflammatory foods will not only increase your pain, but they will also decrease the effectiveness of any medication you take for that pain.
Your choice of foods also has been shown by research to affect your genes. Inflammatory foods can affect the way genes produce proteins that increase or decrease your experience of pain. Eating foods that cause genes to make more proteins that increase pain can affect you for three or four weeks.
If you experience chronic pain, your food choices increase in importance. Choosing the right kinds of foods will help your body heal faster, help you sleep better, and help your pain medications work better. Inflammatory foods will make the opposite happen.
Your gut system contains about 70% of your immune system cells. These cells are in constant, daily contact with the food you eat. Once this immune system is triggered by inflammatory foods, bacteria within foods, or begins treating foods as allergens, inflammation results. The same thing can happen if there is an imbalance of important hormones, such as insulin, in the gut system.
A report from the American Journal of Clinical Nutrition showed consuming processed sugars or other foods containing starches with high glycemic content increased the redness, pain, swelling, and heat of inflammation.
The Standard American Diet (SAD) is a prime example of what not to eat if you want to decrease inflammation. It is mainly composed of inflammatory foods such as refined sugars and starches, saturated fats, and trans fats. It is low in natural antioxidants, Omega-3 fatty acids, and fiber from vegetables, whole grains, and fruits are lacking.
One study showed women who ate this diet had higher CRP, IL-6, E-selectin, sVCAM-1, and sICAM-1. This was compared to a diet higher in fruit, vegetables, legumes, fish, poultry, and whole grains.
This same study supported previous research findings concerning the link between trans fat consumption and increased inflammation. Women in this study who were in the highest quintile of consumption of trans fats showed a CRP level 73% higher than women in the lowest quintile. IL-6 levels were 17% higher for the same group of women.
 Oxidative stress is significantly associated with inflammation. Consumption of higher levels of fruits and vegetables leads to lower levels of both oxidative stress and inflammation. Fruits and vegetables have considerable antioxidant properties that are foundational to their modulation of inflammation when added to your diet. Oxidants produced when food is metabolized, such as superoxide radicals or hydrogen peroxide, tend to activate the NF-kB pathway, leading to increased inflammation. Limiting or even reversing the proinflammatory responses to meals that are high in saturated fats may be possible through adding more antioxidants, fruits, and vegetables to your diet.
Oxidative stress is significantly associated with inflammation. Consumption of higher levels of fruits and vegetables leads to lower levels of both oxidative stress and inflammation. Fruits and vegetables have considerable antioxidant properties that are foundational to their modulation of inflammation when added to your diet. Oxidants produced when food is metabolized, such as superoxide radicals or hydrogen peroxide, tend to activate the NF-kB pathway, leading to increased inflammation. Limiting or even reversing the proinflammatory responses to meals that are high in saturated fats may be possible through adding more antioxidants, fruits, and vegetables to your diet.
Whole grains are important in your diet because the refining process of grains removes the fiber, minerals and vitamins, phytonutrients, and essential fatty acids. You’re left with refined carbohydrates, or inflammatory foods. These refined carbs quickly raise blood glucose and insulin levels. The resulting hyperglycemic condition adds to the production of free radicals and proinflammatory cytokines.
It’s easy to see how the choice of these inflammatory foods leads to significant health risk. In addition, there is accumulating evidence that diet also affects your mental health. Inflammation has been shown to be involved in the development of depression, for example. This suggests your dietary choices are important to your mental health through the mechanism of inflammation because diet affects inflammation, which can have a significant influence on the development of, and experience of, depression.
The links between inflammation, stress, and depression are well documented. Clinical and research evidence shows these links very well.
Both stress and depression add to the risk of infection, as well as longer duration of infections and slower wound healing. All of these can increase the production of proinflammatory cytokines as well. Even without physical injury or infection, stress and depression can lead to the production of these proinflammatory cytokines. There is also some evidence that both clinical depression and subclinical depression symptoms can sensitize your body to inflammation, leading to a higher cytokine response when stress is present.
 In addition, both stress and depression cause changes in health behaviors related to inflammation. Both conditions tend to decrease sleep, which tends to increase IL-6 production. Depression and stress also stimulate increased production of proinflammatory cytokines. Thus, both directly and indirectly, stress and depression stimulate the production of proinflammatory cytokines.
In addition, both stress and depression cause changes in health behaviors related to inflammation. Both conditions tend to decrease sleep, which tends to increase IL-6 production. Depression and stress also stimulate increased production of proinflammatory cytokines. Thus, both directly and indirectly, stress and depression stimulate the production of proinflammatory cytokines.
One of the major mechanisms for the production of stress-related proinflammatory cytokines is NF-kB. NF-kB has an activating effect on the genes that control the expression of the proinflammatory cytokines. One study showed a 341% rise in NF-kB activity within ten minutes of a stressor in the laboratory. When stress increases, so does the level of norepinephrine in your body. This increases activation of NF-kB, showing a direct pathway from your endocrine system to inflammation.
Under conditions of chronic stress, long-term changes in proinflammatory cytokine production can also occur. This appears to happen through increased oxidative stress that activates the NF-kB pathway. One longitudinal study comparing the average annual increase in serum levels of IL-6 found a fourfold increase in a group of men and women who were chronically stressed due to caring for spouses with dementia compared to a similar group without the caregiving responsibilities. Another study of mothers caring for a chronically ill child compared with mothers of healthy children showed higher oxidative stress in the first group as measured by levels of F2-isoprostanes. These studies, and others, strongly suggest stress and depression increase oxidative stress, add to NF-kB activation, lead to more sympathetic hyperactivity, and increase production of proinflammatory cytokines.
 Both Omega-3 and Omega-6 fish oils are important in your diet, as long as they are balanced appropriately. Lower Omega-6 to Omega-3 ratios lead to lower proinflammatory cytokine production. This is because they both compete for the same metabolic pathways. Eicosanoids derived from the arachidonic acid in Omega-6 lead to increases in proinflammatory cytokines, IL-1, IL-6, and TNF-a. These cytokines that come primarily from corn, sunflower, and safflower oils are precursors of the proinflammatory eicosanoids of the prostaglandin-2 series. On the other hand, polyunsaturated fatty acids from Omega-3 can reduce the production of these eicosanoids. Omega-3 fatty acids come from sources such as fish oil, flax seeds, and walnuts.
Both Omega-3 and Omega-6 fish oils are important in your diet, as long as they are balanced appropriately. Lower Omega-6 to Omega-3 ratios lead to lower proinflammatory cytokine production. This is because they both compete for the same metabolic pathways. Eicosanoids derived from the arachidonic acid in Omega-6 lead to increases in proinflammatory cytokines, IL-1, IL-6, and TNF-a. These cytokines that come primarily from corn, sunflower, and safflower oils are precursors of the proinflammatory eicosanoids of the prostaglandin-2 series. On the other hand, polyunsaturated fatty acids from Omega-3 can reduce the production of these eicosanoids. Omega-3 fatty acids come from sources such as fish oil, flax seeds, and walnuts.
The influence of stress on your metabolic response to foods has also been well documented. Those familiar with AFS understand how this relationship works. Stress increases post-meal spikes in symptoms and slows the clearance rate of those same effects. Some of the specifics regarding how stress affects metabolism are significant.
When you eat a meal high in saturated fat, within an hour triglycerides increase in your bloodstream and stay high for up to eight hours. This can lead to increased risk for type 2 diabetes, metabolic syndrome, obesity, and cardiovascular disorders. These high-fat meals also substantially increase levels of IL-6 and CRP. They also increase oxidative stress and sympathetic hyperactivity.
 There are a multitude of inflammatory foods that should be avoided. The list would be lengthy if it were produced, and some of the most common foods would be included.
There are a multitude of inflammatory foods that should be avoided. The list would be lengthy if it were produced, and some of the most common foods would be included.
For starters, the “3 Ps” should be avoided: processed, packaged, and prepared foods. All of these are inflammatory foods because of the additives, oils, sugars, and artificial sweeteners in them. Fast foods top the list.
Many baked goods contain hydrogenated oils and trans fats. These include margarine, shortening, and lard. Margarine is especially bad; it is essentially a poison developed many years ago to alleviate a shortage of butter.
Meat and poultry also increase inflammation. Wild-caught fish are the exception. Small portions of meat and poultry should be alright, but make sure your meals have larger portions of vegetables.
Plant based meals decrease inflammation. If you’re a meat eater and must have meat, try to find grass-fed beef, chicken, turkey, and eggs, or at least those without hormones.
Some people may experience increased pain levels for up to three weeks with even a taste of wheat, sugar, potatoes, juice, or soda. Others will feel more pain for up to four months after eating hydrogenated or partially hydrogenated oils.
Some go so far as to class margarine and aspartame, marketed as NutraSweet, as poisons for your body. The hydrogenated fat in margarine has been associated with many chronic illnesses. Aspartame undergoes conversion in the body into formaldehyde and methanol. Formaldehyde, besides being embalming fluid, has strong links to cancers. Methanol can cause brain damage and increases pain sensations. The amount of methanol in two diet sodas per week is more than your body can detoxify. This allows it to accumulate in your body and cause damage. You may require two months to detox satisfactorily once you stop ingesting aspartame.
White flour and sugar are two of the most common inflammatory foods. White flour actually changes into sugar in the presence of the digestive enzymes found in your mouth. A lot of sugar in your diet leads to an increase in advanced glycation end-products (AGEs), or proteins bound to glucose molecules. When your body works to break this bond, proinflammatory cytokines are produced. And you’ve already seen what these cytokines lead to.
Some inflammatory foods cause allergic reactions in your body. Some allergies throw your blood sugar into imbalance, which then can lead to increased inflammation. This then causes your pancreas to release more insulin, which can lead to more cortisol being secreted by the adrenals. Cortisol causes you to retain belly fat instead of burning for energy. High amounts of belly fat are an indicator of chronic inflammation.
It’s important for you to keep in mind the hidden sugars in many foods as well. For example, many brands of catsup contain significant amounts of sugar. And these simple carbohydrates can be hidden in unexpected places. For example, a nine-ounce bag of potato chips contains 32 teaspoons of sugar. If you drink a soda with chips, you’re adding another 16 teaspoons of sugar – or more! A small size Dairy Queen Blizzard contains the equivalent of 21 teaspoons of sugar.
The American Journal of Cancer Nutrition reported a study that supported the findings that sugar increases inflammation. The study found a large amount of sugar in foods raised the CRP serum level in those who consumed those foods.
Three cups of cooked pasta is equal to 25 teaspoons of sugar in your body. And, of course, this means a greater level of inflammation.
 Food additives create more inflammatory foods. These additives include artificial colors, preservatives, flavor enhancers, and stabilizers. These substances include benzoates, sulfites, and most food colors. Many of the foods directed at children contain these inflammatory food additives.
Food additives create more inflammatory foods. These additives include artificial colors, preservatives, flavor enhancers, and stabilizers. These substances include benzoates, sulfites, and most food colors. Many of the foods directed at children contain these inflammatory food additives.
Many dairy products contain hormones and antibiotics given to the animals they come from. These products include yogurt, butter, ice cream, cottage cheese, and cheese, among others.
Wheat is present in many forms in the grocery store. It is readily acid-forming and significantly increases inflammation in your body. It contains gluten, as do many other grains, which is also very proinflammatory.
Alcohol in its many drinkable forms also converts quickly to sugar in the body and increases inflammation readily. It’s best to leave it alone or at least use it in moderation.

Now that you know which inflammatory foods to avoid, you’ll need to know what foods can reduce or eliminate inflammation. Many of these foods act as natural inflammation remedies.
All meats are not bad. Be sure to choose the right kinds and keep the amount you consume in moderation. Free range, grass fed, and organically raised animals yield better meat as far as inflammation is concerned. The nutritional value of these meats is much greater than meat from industrially farm-raised animals. Pasture raised animals’ meat is higher in Omega-3s and lower in Omega-6s. This leads to lower levels of inflammation in your body.
Cold water fish should be eaten three times a week by adults. This gives you increased Omega-3s with all their health benefits, including decreased inflammation. These kinds of fish include salmon, herring, anchovies, and sardines.
Vegetables like garlic, leeks, artichokes, and asparagus are high in fructooligosaccharides. These complex sugars are hard to digest by your body, causing you to absorb fewer calories and avoid spikes in blood sugar. They feed the good bacteria in your gut system, helping you keep a healthy gut microbiome.
Brightly colored fruits and vegetables are among the best anti-inflammatory foods. The phytochemicals that help fight inflammation also give these fruits and vegetables their bright colors. These include carotenoids that give carrots and squash their orange coloring, as well as lycopene that gives tomatoes and red bell peppers their distinctive red colors.
Grapes and berries contain resveratrol, the phytochemical recently found to fight heart disease. It also aids in reducing inflammation.
Olive oil is another beneficial food choice. High in polyphenols, extra virgin olive oil heated to less than 140 degrees Celsius is the most beneficial in cooking. Olive oil is also a great source of oleic acid, which is a powerful anti-inflammatory.
Nuts and seeds should be added to your diet as anti-inflammatory foods. They contain a number of excellent nutrients, including Omega-3s, and they can keep blood sugar at appropriate levels when used as snacks throughout the day. Walnuts especially are full of phytonutrients not found elsewhere.
Avocados are also packed with nutrients. Phytosterols, carotenoids, and alpha-linoleic acids, along with mono- and polyunsaturated fats are present in avocados. Numerous studies have shown avocado consumption to be linked to reduced inflammation, reduced cholesterol, and balanced blood sugar levels. This versatile food can be used as a garnish, a main dish, or as a substitute for butter and margarine.
Cruciferous vegetables like broccoli, kale, Brussels sprouts, and cauliflower are high in indole 3-carbinol and should be added to your inflammation-lowering food choices. This vegetable family is also high in sulfur which helps detox your liver.
Don’t avoid all fats. Fats give you the building blocks with which your body builds new cells and cell membranes. It’s these cell membranes that allow good things into your cells and expel bad things from the cells. It is very important to have strong cell membranes. Remember this: When you eat hydrogenated fat, every cell you make that day has this hydrogenated fat in it.
As you reduce and eliminate the inflammatory foods from your diet, you may want to consider adding supplements and herbs to increase your body’s ability to fight inflammation.
Omega-3 fatty acids. The benefits of these essential fatty acids have been covered elsewhere in this article. They come from fish and flax seed, but can also be found in supplement form. Side effects of Omega-3s include a fishy aftertaste, burping, slight nausea, and bloating. These typically are mild, but if they persist you should consult your healthcare professional. An increase in bleeding or bruising are unusual side effects but may occur. Severe side effects are rare.
Ginger. Since the 1970s, research has been accumulating that supports the anti-inflammatory properties of ginger, which have been known in other parts of the world for centuries. It inhibits prostaglandin synthesis and leukotriene biosynthesis, both part of the inflammatory response. Because of this effect, ginger can have an action similar to nonsteroidal anti-inflammatory medications. Some mild side effects of ginger include heartburn, diarrhea, and stomach discomfort. It may increase the risk of bleeding. If you’re pregnant or nursing, consult with your healthcare provider before taking ginger.
Turmeric. Shown to be a good anti-inflammatory agent, turmeric can also be used as a flavor enhancer for foods. Typically, there are few, if any, side effects of turmeric. However, some people report stomach upset, nausea, diarrhea, and dizziness. If you’re pregnant, medicinal amounts of turmeric should be avoided. If you have gallbladder or bleeding problems, avoid using turmeric. For people with diabetes, turmeric may lower blood sugar. People with GERD should avoid turmeric because of the potential for increased stomach problems.
 Cinnamon. Also a good anti-inflammatory, the food uses of cinnamon are well known. In general, cinnamon has few, if any, side effects. It should not be taken in large amounts by mouth for a long period of time. Those with diabetes should pay close attention to blood sugar levels when taking cinnamon. If you are planning surgery, you should stop taking cinnamon two weeks prior to the surgery. If you have liver disease, avoid medicinal levels of cinnamon.
Cinnamon. Also a good anti-inflammatory, the food uses of cinnamon are well known. In general, cinnamon has few, if any, side effects. It should not be taken in large amounts by mouth for a long period of time. Those with diabetes should pay close attention to blood sugar levels when taking cinnamon. If you are planning surgery, you should stop taking cinnamon two weeks prior to the surgery. If you have liver disease, avoid medicinal levels of cinnamon.
Probiotics. The benefits of probiotics are many. They improve gut health and are very good anti-inflammatory agents. The most common side effects of probiotics include bloating and stomach discomfort. Large doses may lead to gas. It’s important to keep in mind the type of biologics in the supplement you are taking.
Glutathione. There are many health benefits to glutathione in addition to being an anti-inflammatory. It appears to be effective in dealing with chronic illness conditions that result from weakened defense systems in your body. Generally, glutathione is safe for use. However, due to a lack of information about its effects during pregnancy and breastfeeding, it’s best to avoid its use.
Vitamin E. This supplement is primarily used in dealing with heart-related conditions and diabetes. It is a beneficial anti-inflammatory as well. It is generally safe for use with no side effects for most people at the recommended dosage of 15mg. In high doses, it is likely unsafe. Some research has suggested vitamin E may increase the risk of hemorrhagic stroke. On the other hand, it may decrease the risk of ischemic stroke.
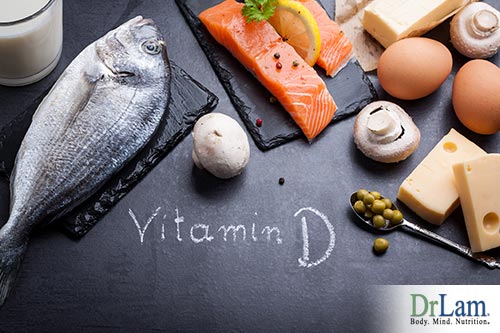 Vitamin D. Everyone is familiar with the ‘sunshine’ vitamin and its health effects on bone growth and strength. Research has shown a lack of this vitamin also increased the risk of diabetes and other chronic health conditions. It is a good anti-inflammatory agent. Vitamin D is generally safe for use in recommended dosages. Taking higher doses for longer periods of time should be done with under a health professional’s supervision due to the possibility of increased calcium in the blood.
Vitamin D. Everyone is familiar with the ‘sunshine’ vitamin and its health effects on bone growth and strength. Research has shown a lack of this vitamin also increased the risk of diabetes and other chronic health conditions. It is a good anti-inflammatory agent. Vitamin D is generally safe for use in recommended dosages. Taking higher doses for longer periods of time should be done with under a health professional’s supervision due to the possibility of increased calcium in the blood.
Quercetin. This supplement is a flavonoid in fruits and vegetables that may have both antioxidant and anti-inflammatory properties. It has been used for conditions of the heart and blood vessels. Care should be taken when using this as a supplement due to lack of information regarding long-term effects. It is probably safe for short-term use, or you could focus on getting it from foods and teas instead. If you’re pregnant or breastfeeding, it’s probably best to avoid using it.
Bromelain. It has been used to reduce inflammation in nose and sinus surgery. However, in general, there isn’t a lot of good information regarding bromelain and its effects. Some mild side effects, such as diarrhea and stomach discomfort, have been reported. Allergic reactions may be possible, especially if you have other allergies. Your healthcare professional should be consulted before using this supplement if you do have allergies.
Most people are not aware of the potential long-term effects of consuming inflammatory foods. These foods can increase the level of chronic pain you feel in the short-term and the risk of developing chronic illnesses in the long-term. Learning the types of foods that are considered inflammatory and avoiding them should greatly improve your quality of life and may lengthen your life as well.
Eating inflammatory foods greatly increases your risk of developing chronic inflammation. Many studies have shown chronic inflammation to be the foundation of increased pain in the body, as well as of developing chronic health conditions that may become worse as you age.