
 Energy: it’s what we need to live. Some of the body’s processes, like respiration and digestion, revolve around getting and producing energy for the other processes of life. Every single thing we do, voluntarily or involuntarily, takes energy. If we improve gut microbiome, our energy development increases as well.
Energy: it’s what we need to live. Some of the body’s processes, like respiration and digestion, revolve around getting and producing energy for the other processes of life. Every single thing we do, voluntarily or involuntarily, takes energy. If we improve gut microbiome, our energy development increases as well.
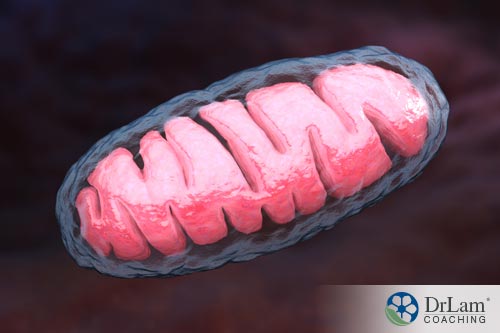
Much of the body’s energy – over 90 percent – comes from the mitochondria in cells. So it is vital that they are functioning at optimal levels if you want to have an active, healthy day-to-day life.
One way to ensure high functioning mitochondria is to improve gut microbiome health. Another is to address any weakening in the mitochondria directly, and yet another is to address any medical conditions that may be affecting mitochondrial health.
It’s very important to support the mitochondria’s energy production with diet, lifestyle and special supplementation when needed. Otherwise, the lack of energy will not just affect your activity level; it will affect every single physical and chemical process, from heart function to brain function.
Consider the cardiovascular system at its most basic level. If you have an average heart rate of 72 beats per minute, this adds up to 103,680 beats per day. This much work needs a significant amount of mitochondrial function and energy.
Another example: even though one of the functions of sleep is to conserve energy, many of your bodily processes are still functioning and need energy. Energy conservation only happens during non-REM sleep; the brain wave activity that occurs in REM sleep is actually just as high, or even higher, as brain wave activity during waking hours.
So it goes without saying that energy conservation is not enough to contribute significantly to your body’s energy requirements, and mitochondrial energy production has to perform at a high level even if you do get enough rest or sleep.
The word mitochondrion, which is singular for mitochondria, comes from the Greek words “mitos” – meaning threads – and “chondrion” – meaning granule.
Mitochondria are one type of organelle (specialized structures that have a specific function within cells) found in eukaryotic cells. Eukaryotic cells are cells that have a nucleus, and other cytoplasmic organelles bound by membranes that separate them from the rest of the cellular space. They also have a cytoskeleton.
Prokaryotic cells on the other hand are cells that do not contain a nucleus and other membrane-bound organelles. They were the only form of life on earth until evolutionary processes brought about eukaryotic cells millions of years later. Bacteria are a type of prokaryote.
What makes mitochondria unique in comparison to other cellular organelles is that they have their own DNA separate from that of the cell itself (which is contained in the nucleus). This is thought to have happened due to the process of endosymbiosis – the evolution of the symbiotic relationship of bacteria living within larger cells. The mitochondrial genome has a striking similarity to bacterial genomes.
Further studies have confirmed this might be the case because the mitochondria and a specific type of bacteria called Rickettsia prowazekii seem to share a similar genetic origin, and both of them are incapable of reproduction outside of eukaryotic cells.
This one reason is why, as we will discuss later, mitochondria within the human cells and microbiota, or gut flora, in the gastrointestinal (GI) tract are able to interact and communicate, and why we must improve gut microbiome to support mitochondria.
The GI tract contains 100 trillion microbes and the human body has upwards of 10 times more microbes than cells. The human microbiome, which is the collection of microorganisms, is estimated to have at least 100-fold more genes than the human genome.
There is a lesser accepted theory on the origin of mitochondria which states that they came about by splitting off part of the cell’s DNA from the nucleus and developed membranes around this portion. This is called the autogenous hypothesis.
A mitochondrion has two membranes – an inner membrane and an outer membrane that are separated by what is called an intermembrane space. This space has folds, called cristae, which go all the way into the interior part of the mitochondrion, the matrix. The matrix is where the mitochondrion’s genetic system is located.
 Mitochondria have many functions, including energy production, maintaining cell cycle and growth, apoptosis (cell death), regulation of cellular metabolism, steroid synthesis, calcium storage and signaling, signaling through reactive oxygen species, and hormonal signaling.
Mitochondria have many functions, including energy production, maintaining cell cycle and growth, apoptosis (cell death), regulation of cellular metabolism, steroid synthesis, calcium storage and signaling, signaling through reactive oxygen species, and hormonal signaling.
The most important function they perform is the production of metabolic energy in eukaryotic cells. They break down carbohydrates and fatty acids through the process of oxidative phosphorylation in order to produce adenosine triphosphate (ATP), the energy currency of life. Much of this process takes place in a mitochondrion’s inner membrane.
More specifically, the process of cellular respiration is where energy is derived from glucose. ATP is the body’s currency for energy. The first step in the process of energy production therefore is changing glucose to pyruvate to produce ATP. With aerobic respiration, which is the type of cellular respiration that occurs in human cells, oxygen is present and the pyruvate then produces more ATP. If there is no oxygen and respiration is anaerobic, no extra ATP is created.
So what happens if the mitochondria are not functioning properly? ATP production is reduced – meaning the energy needed for all of the body’s processes is reduced. That can become quite a challenging situation for health and wellness.
This reduction in mitochondrial energy production sometimes results in, or is termed as, mitochondrial disease – a set of different diseases that fall under that umbrella term, including conditions like Alzheimer’s, Parkinson’s, Lou Gehrig’s disease, autism, muscular dystrophy and chronic fatigue.
In fact, mitochondrial dysfunction, or the subclinical state of mitochondrial weakness, has been associated with many seemingly unrelated conditions such as diabetes, cancer, autoimmune disorders, thyroid problems, extracellular matrix congestion, cognitive issues, liver sluggishness, and adrenal fatigue. The reason is simple. All cellular function requires energy. Poor energy production equals poor energy state, a common denominator in practically all chronic diseases – including those mentioned above.
Here’s the question that comes next: if the tissue of the organs affected by a certain condition is given specialized therapy, will that therapy also support the mitochondria within the cells of that tissue?
Or do we need to support the mitochondria throughout the entire system so that tissue responds better to therapy?
The answer is yes to both questions. It seems to be that supporting overall mitochondrial function will have an impact on whatever condition you’re dealing with, and by addressing whatever condition you’re dealing with, you will also support mitochondrial function.
It can be a little difficult to differentiate between all these different conditions and mitochondrial dysfunction in order to take the right steps. However, there is one thing that you can count on that will have an effect in all cases – the state of the gut’s microbiome. If you improve gut microbiome health and function, you will improve all of these issues, including problems on the mitochondrial level.
That is because if the microbiome is not in an optimal state, you’re not absorbing the nutrients that you need for mitochondrial ATP production, meaning you don’t have the fuel for your tissues to be healthy and strong. Also, there will be an imbalance of gut metabolites and inflammatory substances that negatively impact the mitochondria.
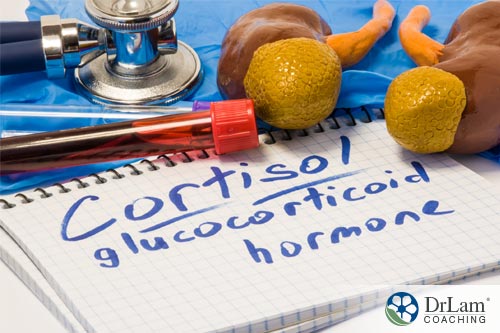
Now let’s talk about another important mitochondrial function: steroid synthesis and hormonal signaling. If these are affected, they can trigger a number of conditions, including adrenal fatigue.
 The inner membrane of the mitochondrion contains the enzyme cytochrome P450. One subset of this enzyme is responsible for the synthesis of steroid hormones by the adrenal glands, the gonads (male testes and female ovaries) and peripheral tissue.
The inner membrane of the mitochondrion contains the enzyme cytochrome P450. One subset of this enzyme is responsible for the synthesis of steroid hormones by the adrenal glands, the gonads (male testes and female ovaries) and peripheral tissue.
This subset of cytochrome P450 acts on the hormonal cascade that synthesizes the adrenal hormones – starting with cholesterol that is converted into pregnenolone, which is then converted into DHEA, estrogen, progesterone, testosterone and cortisol.
Cortisol is the body’s main anti-stress hormone. Along with 50 other types of hormones, it is produced by the adrenal glands, which are two organs found on top of the kidneys that are part of the body’s endocrine system.
The adrenals are the last link in the body’s hypothalamic-pituitary-adrenal (HPA) axis, which is part of the hormonal circuit of the body’s global stress-response system – the NeuroEndoMetabolic (NEM) Stress Response.
Cortisol has many important functions, including regulating blood pressure and blood sugar levels, maintaining heart and blood vessel function, suppressing the immune system and neutralizing inflammation – all of which are affected by, and respond to, stress. Although it is natural for the body to handle stress with a series of stress responses, it is not built to do so for severe or prolonged states of stress. If you improve gut microbiome health and function, you will improve coritisol production as well.
Chronic stress can dysregulate the adrenal glands and affect cortisol production, causing Adrenal Fatigue Syndrome (AFS). The usual trajectory of AFS is that in the beginning stages, cortisol output increases and then when the adrenal glands are exhausted at the later stages, cortisol output drops significantly.
Each of the four stages of AFS is marked by a collection of symptoms, though throughout, fatigue is the major theme. Symptoms range from the mild to the severe and can include things like easily gaining weight and difficulty losing it, difficulty falling asleep and difficulty rising in the morning, hypoglycemia, brain fog, food sensitivities, irritable bowel, lowered immunity, low libido, PMS, fertility problems, anxiety, heart palpitations, mild depression and others.
But we’re not talking only about mental or emotional stress here. Health problems can cause AFS, and mitochondria that are not functioning properly are one example.
 Cytochrome P450 resides in the inner membrane of the mitochondria. So when there is a problem there, adrenal hormone production is directly affected. Not having enough cortisol, AFS symptoms can develop.
Cytochrome P450 resides in the inner membrane of the mitochondria. So when there is a problem there, adrenal hormone production is directly affected. Not having enough cortisol, AFS symptoms can develop.
But it’s a little more than that…
Symptoms of mitochondrial disease and AFS are similar, but the causal factors of the fatigue in both conditions are different. Dysfunction in ATP production will of course lead to fatigue, as there isn’t enough life energy for the body to function optimally.
With AFS, there isn’t enough of the hormone that neutralizes stress and the body has to downgrade some of its functions in an effort to conserve energy. That also leads to a lessening of ATP and a state of fatigue.
On a larger scale, the adrenal glands and cortisol are only one part of the NEM stress response. The NEM is composed of six circuits that work together to neutralize stress and the damage it causes the body. They are the neuroaffective, the cardionomic, the hormone, the metabolism, the inflammation and the detoxification responses.
These circuits can also dysregulate if stress is chronic, or if there isn’t enough mitochondrial ATP, or if there is a medical condition that is not addressed. Thankfully, if we improve gut microbiome, all of these elements, along with the mitochondria, will function better.
 In the gut, there are cells with their mitochondria and ATP production right next to where the bacteria that make up the gut microbiota reside. The gut’s bacteria interact with the body’s cells mostly through the cell’s mitochondria, and, as we mentioned earlier, this could be because the bacteria and the cell’s mitochondria share some functional and structural similarities, such as similar genetic origins.Studies show that if you improve gut microbiome, the health of the microbiome will improve the quality and diversity of the mitochondria’s functions.
In the gut, there are cells with their mitochondria and ATP production right next to where the bacteria that make up the gut microbiota reside. The gut’s bacteria interact with the body’s cells mostly through the cell’s mitochondria, and, as we mentioned earlier, this could be because the bacteria and the cell’s mitochondria share some functional and structural similarities, such as similar genetic origins.Studies show that if you improve gut microbiome, the health of the microbiome will improve the quality and diversity of the mitochondria’s functions.
The gut microbiome is intimately linked with the brain, immune system and the different hormonal systems of the body. It also has a major influence over chronic disease risk and genetic expression.
One of the big reasons why is because the gut is where inflammation begins. With much of the body’s immune tissue located there, the gut’s microbiome produces cytokines that help regulate the immune response.
Cytokines are types of proteins, glycoproteins and peptides that help cells communicate during an immune response. They help stimulate the cells needed for the immune response to move to the sites of inflammation or injury.
These cytokines also signal the brain to produce neurochemicals in order to support the inflammation response. These neurochemicals can affect mitochondrial ATP production and also the hormone response involving cortisol. In fact, the gut is sometimes referred to as the second brain for good reasons.
When you have any degree of dysbiosis, where gut flora is out of balance, this can create a state of chronic inflammation that affects the brain as well as systemically. Chronic inflammation acts like a constant negative force on the delicate balance of hormones and the mitochondrial processes that are so essential for energy.
That is because a dysbiotic microbiome will increase the permeability of the intestinal epithelial barrier, creating leaks. This barrier is a single-cell layer, and it is the largest and most important one that protects the body from the environment. Its selective permeability allows the absorption of nutrients, water and electrolytes while keeping out antigens, gut flora and toxins from the bloodstream.
When there are leaks in this barrier – which is sometimes referred to as a “leaky gut” – substances enter the system that aren’t supposed to be there and the immune system sees them as threats and attacks them.
If these leaks are not sealed, it creates a state where the immune response is constantly triggered. As more and more cytokines adversely affect mitochondrial ATP production, and cortisol levels are thrown out of balance, a state of fatigue and a host of other symptoms inevitably follow. Improving the health of the gut’s microbiome will help seal these leaks and protect ATP production.
 The relationship between dysbiosis and mitochondrial function is a two-way street. Mitochondria produce reactive oxygen species, also called free radicals, when they break down the carbohydrates and fatty acids in order to produce ATP.
The relationship between dysbiosis and mitochondrial function is a two-way street. Mitochondria produce reactive oxygen species, also called free radicals, when they break down the carbohydrates and fatty acids in order to produce ATP.
Although a certain amount of free radicals are inevitable in the process of cellular respiration and energy production, if there is an excess of them in the system without sufficient neutralization by antioxidants, you get a state called oxidative stress, resulting in reactive metabolites that are destructive in nature.
Therefore, oxidative stress has many health hazards. It speeds up the aging process and can cause a number of conditions including cardiovascular disease, age-related cancers, liver congestion, extracellular matrix pollution.
As well, oxidative stress has an impact on mitochondrial health. It can trigger mitochondrial genetic mutations, change the permeability of mitochondrial membranes, cause damage to the mitochondrial respiratory chain and impact the mitochondria’s defense systems.
All of this can lead to mitochondrial dysfunction, which can then lead to many of the problematic health conditions associated with it. This is especially the case with neurodegenerative diseases like Parkinson’s disease and Alzheimer’s disease. The clinical picture becomes convoluted and confusing even to the best of practitioners. Most healthcare professionals give up and patients are abandoned when the situation becomes severe.
The production of free radicals by the mitochondria also plays a role in inflammation and the immune system response, and it is sometimes targeted by pathogens. Too many free radicals will damage the ability of the microbiota to regulate the gut epithelial barrier and increase the permeability of the gut lining.
So now that we know how free radicals released by the mitochondria can affect the gut, let’s now look at how metabolites released by the gut affect mitochondria.
The gut’s microbiome releases metabolites that can influence many things, including ATP production. The production of these metabolites is not something static. Although, it can be affected by things like your diet, whether you were breastfed or not, if you’ve been taking antibiotics, if you use disinfectants, and if you’re exposed to toxins, among others. If you improve gut microbiome health then you will improve these metabolites.
As these bioactive metabolites enter circulation, they can have an effect on your health and even behavior. Some of these metabolites are inert. They are harmless but have to be excreted. Others are reactive and toxic.
These reactive metabolites can be most problematic as they add to the removal workload burden of an already weak body. Untimely or incomplete clearance of such reactive metabolites can trigger adrenal crashes, multiple chemical sensitivities, food intolerance, paradoxical reaction to drugs and nutritional supplements, and exaggerated response to medications.
For example, we have seen that when we do metabolite testing and there are higher than optimal levels of the reactive metabolites, we find that sufferers also tend to have a multitude of non specific symptoms such as those mentioned above.
It is clear that the relationship between microbiota and mitochondria can be thrown out of balance by free radicals on one hand and metabolites on the other.
Since the microbiota acts on mitochondrial activity in order to strengthen interaction with host cells, if the relationship is not working properly, that interaction is in turn weakened.
So, understanding the microbiota-mitochondria relationship can open up new windows into the treatment of mitochondrial and metabolic diseases, and how to improve the gut balance in the microbiome in order to support mitochondrial function. This balance depends on the quality and diversity of the microbiota.
 The relationship between mitochondria and microbiota is just one example of how the gut’s microbiome can affect the rest of the body. Dysbiosis can impact nutrient supply, protection from pathogens and susceptibility to infections, vitamin production, and other metabolic and immunological issues.
The relationship between mitochondria and microbiota is just one example of how the gut’s microbiome can affect the rest of the body. Dysbiosis can impact nutrient supply, protection from pathogens and susceptibility to infections, vitamin production, and other metabolic and immunological issues.
As we know, the microbiome is vital for the body’s immune response. With such a large chunk of the immune system’s tissues there, a strong and healthy microbiota will yield a strong and healthy immune system that can fight off pathogens, clear out toxins and damaged cells, and return to normal after its job is done. A weak gut makes for a weak immune response.
Also, over 80 percent of serotonin comes from the gut, so if we improve gut microbiome, it can help with issues like depression and anxiety. There are opioid receptors in the gut that can affect the pain throughout the entire body.
Diet has also been shown time and again to alter heart function, and as the heart needs a lot of energy, what you eat plays a key role in providing the necessary fuel for your mitochondria to produce ATP.
Nutrition and the gut microbiome are prime environmental triggers for the development and modification of lifestyle-related chronic disease, including chronic inflammatory diseases of the GI tract, such as Crohn’s disease and ulcerative colitis.
More Americans die of Alzheimer’s disease than anywhere else in the world, and Americans die of more cancers than many other parts of the world.
The answer could be found in how people in the West eat. In the US, we have the Standard American Diet, which is very high in fat and low in fiber, and full of sodium and processed sugar. There is also a higher tendency to eat fast food in Western countries.
Other studies show the effects on health of populations that take on similar diets after centuries of eating differently. For example, in the Somali diaspora that migrated to Western countries, there is a significant increase in autism compared to the level that exists in Somalia itself.
This seems to confirm the idea that diet can help improve gut microbiome, and produces metabolites, which in turn affect mitochondrial function and genetics, as well as behavior.
There is a scientific field called nutrigenomics that studies the effects of food on genes, and it focuses on how to prevent or treat diseases along those lines. With regards to obesity, the general consensus is that both genetic and environmental factors play a role.
For example, you are more likely to be overweight if your mother is overweight. Previously, this link was thought to be because of the passing down of unhealthy eating habits, but recently we’re seeing that it also has to do with the mother’s microbiota. The microbiota of an overweight mother differs from that of a mother who has a healthy weight.
Another factor is whether you’ve been inoculated or not as an infant, because that has an effect on the early development, as well as, how you will improve gut microbiome.
 Over the last few decades, obesity among adults and children has risen significantly. It has become a worldwide epidemic, affecting 35 percent of the global populations and half of Americans over 50 years of age. Obesity creates a proinflammatory environment in the body, and we are also seeing that it is a disease of inflammation. As we have seen, inflammation starts in the gut.
Over the last few decades, obesity among adults and children has risen significantly. It has become a worldwide epidemic, affecting 35 percent of the global populations and half of Americans over 50 years of age. Obesity creates a proinflammatory environment in the body, and we are also seeing that it is a disease of inflammation. As we have seen, inflammation starts in the gut.
Recent studies show that the gut microbiota plays a central role in maintaining healthy body weight, and in the prevention and treatment of obesity. Prebiotics have become one weapon in the fight against obesity, with some formulas out there whose purpose is to help with weight loss and leanness.
Prebiotics are a special type of plant fiber that helps feed and strengthen the good bacteria already present in the gut. Probiotics are foods or formulas that contain live “good” bacteria.
 Removing certain things from your life and diet can help improve gut microbiome. Along with mitochondrial dysfunction and an unhealthy diet, there are a few things that can weaken the gut microbiome:
Removing certain things from your life and diet can help improve gut microbiome. Along with mitochondrial dysfunction and an unhealthy diet, there are a few things that can weaken the gut microbiome:
So, it goes without saying that if you want to improve gut microbiome, you want to stay away from these things as much as possible. Of course, some things will be unavoidable, so it’s just a matter of doing your best.
Another stressor on the gut flora is smoking. The influence that cigarettes can have on the microbiota can explain the weight gain that is seen after people quit smoking. In fact, one of the main concerns of smokers who want to quit is how they will avoid this weight gain.
Before, it was thought that the weight gain after smoking cessation had to do with the issue of oral fixation. We’re now seeing that it’s also about a modification in the gut’s microbiota, and how it becomes more efficient at extracting calories from ingested food after the influence of smoking has stopped.
Even with the risk of weight gain, quitting cigarettes should top the list of things to avoid if you want to balance your gut flora and, of course, reverse the lung damage and free radicals that come from smoking. That doesn’t mean that you should let your weight get out of control, because as we have discussed, that is also a cause of health problems.
Another interesting observation is how a 24-hour fast can produce a marked change in the gut’s microbial ecology. This may be one of the reasons that people seem to feel better after fasting. The other reasons are that there is a lessening of burden on the GI tract and less exposure to allergenic foods, which also improve gut microbiome.
Does that mean you should immediately begin a fast? The answer is No, because this really depends on the condition of your health. For example, if you suffer from adrenal fatigue, you are probably already suffering from nutrient deficiencies and lack of energy, as well as a higher risk for hypoglycemia. Fasting can trigger adrenal crashes in a weak body.
An adrenal fatigue diet is a much better option that can help support your adrenals. The great thing is that, this kind of diet can also improve gut microbiome.
 You also want to improve gut microbiome by adding certain things to your health and lifestyle that promote gut flora balance. This includes bone broth, fermented pickles, sauerkraut and kimchi (just keep an eye on sodium content), naturally fermented yogurt made of raw dairy, miso, kefir, unpasteurized milk and tempeh. Those with systemic candida need to be careful as the body may not be able to tolerate fermented foods well.
You also want to improve gut microbiome by adding certain things to your health and lifestyle that promote gut flora balance. This includes bone broth, fermented pickles, sauerkraut and kimchi (just keep an eye on sodium content), naturally fermented yogurt made of raw dairy, miso, kefir, unpasteurized milk and tempeh. Those with systemic candida need to be careful as the body may not be able to tolerate fermented foods well.
You can also consider adding supplements and digestive enzymes to help your gut and digestion. Probiotics have been found to help with reducing LDL cholesterol, improving eczema, reducing insulin resistance and nutrient absorption. This is another testament to how we can improve gut microbiome functions that affect the rest of the body. Side effects of probiotics can include constipation, anxiety, diarrhea, and fatigue. The weaker the body, the bigger the risk.
So far, we’ve focused on how we can improve gut microbiome that affects your mitochondrial ATP production and overall health. This can definitely help with mitochondrial disease or dysfunction. It can also help a lot with adrenal fatigue and a dysregulated NEM stress response. In fact, it’s not so much about brain cells or adrenal cells when we’re talking about fatigue. It has much more to do with the gut microbiome.
You will, of course, want to address any other condition you might have, like adrenal fatigue. Also, a healthy thyroid is essential for the mitochondria, as thyroid hormone stimulate cellular respiration and regulate mitochondrial function. So, if you have any thyroid issues, make sure to address them right away.
But what happens when the mitochondria within the cells of the affected organs, like thyroid or adrenal cells for example, can’t respond to the therapy? Would an adaptogen help?
An adaptogen is a substance that helps the body adapt to and resist stress, whether physical or environmental. Adaptive herbs like Rhodiola and Ashwagandha have been used since ancient times in Traditional Chinese Medicine and Ayurvedic Medicine respectively. They can be supportive of the adrenal glands, helping the body to adapt to and protect itself from stress.
Unfortunately, these also have very undesirable long term effects so extreme care should be in place prior to beginning any herbal or glandular therapy. Proper professional guidance is a must, and any inappropriate use of these natural compounds is one of the most common recovery errors in those with advanced adrenal fatigue. They can be considered if the body is strong, however.
Would supporting the mitochondria throughout the entire body help effect changes in adrenal cells so they become more adaptive naturally?
Since there aren’t any medications that treat mitochondria specifically, you can support their functioning through supplementation. Vitamins B1, B2, B6, B12, C and E are important, so are folic acid, pantethine and pantothenic acid, niacin and biotin. Some of these vitamins also have antioxidant activity, which helps neutralize the free radicals created by, or affecting, the mitochondria.
You’ll want to take supplement formulas that are made to improve mitochondrial function, and they are usually cocktails of the ones listed above. You should also consider coenzyme Q10, arginine, glutathione, magnesium, hawthorn, vitamin D, L-carnitine and marine phytoplanktons.
You will also want formulas that are fat-soluble or made in a way that makes them bioavailable enough to enter the cells. An oral liquid that is absorbed in the small intestine is preferred, with the carrier lipids being phospholipids. High quality and alcohol-free are a must.
 By now, it could be a little overwhelming to consider all of these supplemental requirements as well as an adrenal fatigue diet and a diet that improves the gut microbiome. If that is your case, there are two pieces of advice we highly suggest you follow.
By now, it could be a little overwhelming to consider all of these supplemental requirements as well as an adrenal fatigue diet and a diet that improves the gut microbiome. If that is your case, there are two pieces of advice we highly suggest you follow.
The first is to avoid the shotgun approach to supplementation. It may sometimes feel easier to just take a bunch of different vitamins and minerals hoping that you are covering all your bases, but eventually this backfires. Some supplements that are good for one condition may adversely affect another.
So you don’t want to take glandulars for adrenal fatigue, supplements for mitochondrial function, prebiotics and probiotics for your gut. That is simply too much on your system and may lead to a crash. It will also not help with figuring out which supplements are actually helpful for you.
The second piece of advice is to get nutritional coaching that takes a holistic approach to your health. It needs to take into consideration your overall state of health and energy, as well as any specific conditions you have and is focused on how to improve gut microbiome health. Then, gradually and gently, make changes to your diet and supplementation regimen.
Now, to get more specific, if you have mitochondrial dysfunction and AFS at the same time, you will need to take care with the mitochondrial supplementation. The reason is that when you boost mitochondrial function, and in turn increase ATP production, this energy boost will cover up, but not heal, the tiredness caused by adrenal fatigue.
What could happen is that you feel better and have more energy from the supplements, so you stop taking them thinking your health has improved, only to crash suddenly because your adrenals are still weak. To avoid this common mistake, your adrenals must be supported first before you start taking mitochondrial supplements, especially if your AFS is advanced.
 Expert medical supervision is required when dealing with both of these conditions at once to avoid crashes and worsening fatigue. Timing is crucial, and the delicate balance of the gut flora should also be taken into consideration. By learning to improve gut microbiome, you can support all of these issues concurrently, as well as reduce all forms of stress as much as possible.
Expert medical supervision is required when dealing with both of these conditions at once to avoid crashes and worsening fatigue. Timing is crucial, and the delicate balance of the gut flora should also be taken into consideration. By learning to improve gut microbiome, you can support all of these issues concurrently, as well as reduce all forms of stress as much as possible.
Reducing stress is something that you need to consider from many angles. First of all, inflammation is a huge stressor on the body. So if there is inflammation, an anti-inflammatory diet might actually be where to start. Bringing down inflammation will help with dysbiosis, AFS and overall health.
Doing adrenal breathing exercises will help with stress management, relaxation and adrenal support. Other breathing techniques can lower anxiety, help you fall asleep and calm your mind. If you’re ready, adrenal yoga can also bring in a gentle form of physical activity that also helps reduce stress.
Other things to consider before taking a mitochondrial supplementation cocktail is how much toxic load you have. If it is higher than normal, you should consider a detoxification protocol. You’ll need to decongest the liver and cleanse the extracellular matrix as well. But once again, these things need to be done with care if you have AFS, as your body is in a fragile state.
Finally, dealing with these conditions means your need for rest and sleep will be increased. Having reduced ATP production and fatigue from AFS will automatically make it more challenging to keep up the usual level of daily activity, so let yourself rest. Give the process of recovery all the time it needs. It takes time to rebuild the gut flora and improve gut microbiome, so be patient.
The gut’s microbiome has been implicated in almost every physical health condition, as well as a few psychological conditions as well. That is why it is paramount to improve gut microbiome balance if you want to lead a healthy, active and disease free life.