 It is said that a healthy gut leads to a healthy life; but around 70% of Americans suffer from gastrointestinal disorders or related symptoms. With modern populations chronically stressed out and processed food now a staple in the everyday diet, statistics like this are rather unsurprising.
It is said that a healthy gut leads to a healthy life; but around 70% of Americans suffer from gastrointestinal disorders or related symptoms. With modern populations chronically stressed out and processed food now a staple in the everyday diet, statistics like this are rather unsurprising.
More and more researchers are discovering just how much our gut health affects our overall health. Many believe that supporting gut health and restoring the integrity of the intestinal barrier should be a priority in terms of health goals for the 21st century.
For many decades, companies have been developing and mass-producing food-like products that hardly resemble the whole foods from which they were originally derived. Most of the water, fiber and nutrients have been replaced with ingredients like seed oils, corn syrup, MSG, and artificial flavorings, colorings, and sweeteners that do not exist in nature. These products are scientifically designed to stimulate our taste buds and induce cravings, leading to overconsumption and, of course, higher profits for food manufacturers. Boxed, canned, or wrapped in plastic – processed foods now dominate our grocery store shelves, and the effects have been detrimental.
Eating a diet that impairs the integrity of your gut will ultimately impair the integrity of your health. Unhealthy lifestyles are taking a toll on the collective health of the nation.
In order to understand the relationship between gastrointestinal (GI) disorders, Adrenal Fatigue Syndrome (AFS), the NeuroEndoMetabolic (NEM) Stress Response, and achieving optimal health, we must first understand why the gut is such an influential part of the body.
The primary purpose of the gut (gastrointestinal or digestive tract) is to absorb nutrients from food – but what people don’t realize is that the gut is also an integral part of our body’s immune system. The gut produces three quarters of the body’s neurotransmitters, contains two third’s of the body’s immune tissues, houses a genome that is one hundred times larger than the human microbiome, and has ten times the amount of bacteria than the rest of the human body combined.
Gastrointestinal disorders affect the gastrointestinal tract, including the esophagus, stomach, small intestine, large intestine, and rectum, along with organs that aid in digestion, such as the liver, pancreas and gallbladder.
When you take a bite of food (a mix of macronutrients, micronutrients, water and fiber) and begin to chew, this commences the breakdown process of the food into smaller pieces. Enzymes in your saliva start to break the carbohydrates down into simple sugars, and once you swallow, the food is now in your stomach where proteins are tackled by digestive enzymes. The stomach signals to your brain that you’ve eaten and that more energy can be used. Next, your stomach sends the food, mixed with digestive enzymes, to your small intestine where it is further broken down by pancreatic enzymes and bile salts.
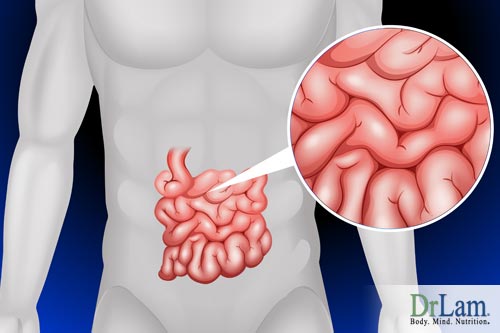 The small intestine is extremely long – if stretched out, it would be the length of a tennis court. But more importantly, the small intestine is the most valuable component of the digestive tract. It serves as a holding tank while food is properly digested and absorbs vital nutrients for your body. Basically, the semi permeable intestinal membrane functions similarly to our skin (but on a much larger scale) in that it’s meant to keep the good stuff in and the bad stuff out. This lining acts as a barrier between your insides and the outside world, and is therefore, it is of utmost importance to your immune system.
The small intestine is extremely long – if stretched out, it would be the length of a tennis court. But more importantly, the small intestine is the most valuable component of the digestive tract. It serves as a holding tank while food is properly digested and absorbs vital nutrients for your body. Basically, the semi permeable intestinal membrane functions similarly to our skin (but on a much larger scale) in that it’s meant to keep the good stuff in and the bad stuff out. This lining acts as a barrier between your insides and the outside world, and is therefore, it is of utmost importance to your immune system.
Once all of the food has been adequately broken down, the most useful nutrients are absorbed through the intestinal barrier to ultimately end up in the bloodstream where they can be transported throughout the body. The remainder of the food passes through the large intestine, where some water and nutrients are further absorbed, and finally, the solid waste is excreted via defecation.
It is important to note that the contents of the small intestine are technically still ‘outside’ of the body, as nothing has actually ‘entered’ the body until it passes through the wall of the small intestine into the bloodstream – essentially the digestive tract is just one hollow tube from mouth to anus. Anything eaten that isn’t absorbed into the bloodstream will pass right through the system. A functioning gut prevents pathogens from entering the body.
In determining gut health and factors leading to gastrointestinal disorders, we must understand these closely related variables: the immune system, gut flora or intestinal microbiota, and intestinal permeability.
Gut-associated lymphoid tissue (GALT) is the gastrointestinal tract’s immune system that works to protect the body from invasion by harmful pathogens. The small intestine contains the largest amount of lymphoid tissue in the entire body; the GALT has various kinds of lymphoid tissue that boast many different kinds of immune cells, like T and B lymphocytes (white blood cells). These T and B cells are a vital component of the immune response, working to identify invaders and generate responses to eliminate malicious pathogens or pathogen-infected cells.
The gut is home to a large and dynamic bacterial population of around 100 trillion microorganisms – this bacterial community is known as the gut microbiota or gut flora. While many of these bacteria are still to be described, there are at least 1000 known species containing over three million different genes, which is 150 times greater than human genes.
Microbiota can weigh up to two kilograms collectively; one third of these bacteria are typical to most humans, however the remaining two thirds of the microbiota are unique to each person. In fact, it’s likely that crime scene investigators will eventually be able to identify people based on unique bacterial footprints left behind in the absence of their DNA.
 The gut flora has three major functions, including metabolic activities, trophic effects, and protective activities. Often referred to as our hidden metabolic ‘organ’ because of its exceptional benefits to our wellbeing, gut flora are able to salvage energy and absorbable nutrients by fermenting non-digestible dietary residues to release short-chain fatty acids (SCFAs) and vitamin K. The SCFAs regulate epithelial cell proliferation and differentiation within the colon to prevent neoplasia from developing. Microbiota have significant nutritional benefits (trophic effects) on intestinal epithelia and immune system function.
The gut flora has three major functions, including metabolic activities, trophic effects, and protective activities. Often referred to as our hidden metabolic ‘organ’ because of its exceptional benefits to our wellbeing, gut flora are able to salvage energy and absorbable nutrients by fermenting non-digestible dietary residues to release short-chain fatty acids (SCFAs) and vitamin K. The SCFAs regulate epithelial cell proliferation and differentiation within the colon to prevent neoplasia from developing. Microbiota have significant nutritional benefits (trophic effects) on intestinal epithelia and immune system function.
Gut flora also have a barrier effect: they protect the colonized human host against invasion by harmful alien microbes. Resident bacteria (the good guys) help by providing resistance against colonization by malicious pathogenic microbes (the bad guys).
It’s obvious that these bacteria in our gut can be incredibly effective in promoting our health, but to avoid gastrointestinal disorders, we need to take extra special care. According to an article published in Therapeutic Advances in Gastroenterology, “disruption to the gut microbiota has been linked with gastrointestinal conditions such as inflammatory bowel disease and obesity”. Another study linked gut flora disruption to colon cancer and multisystem organ failure.
There are a number of things that can disrupt your gut flora. For example, when you’re sick and take antibiotics, it can take up to three months for your gut microbiota to return to normal. Antibiotics can lead to something known as dysbiosis, which is when you have a microbial imbalance in your body – poor diet choices and overconsumption of alcohol can also cause dysbiosis. Allergenic foods, toxins from medications and the environment, and infections such as those from bacterial overgrowth, parasites and candida overgrowth can also cause dysbiosis.
The relationship between a human host and his/her microbiota significantly impacts the immune system, as they exchange chemical signals to communicate. This helps the immune system to determine potentially harmful bacteria from the good bacteria, and thus resulting in an anti-inflammatory response as the immune system works to fight off these pathogens.
With regards to AFS and gastrointestinal disorders, the common denominator boils down to one thing: stress. The ability to deal with stress is pertinent to human survival, and in this day and age, the amount of stress on the average person has become astronomical. Whether it’s emotional, mental, work-related, physical, or environmental stress, tremendous strain on the body can lead to imbalances in our NEM stress response.
Our bodily stress regulation systems are controlled by the adrenal glands, and when they’re consistently overworked, they become dysfunctional, leading to a host of maladies as the body loses its ability to effectively cope with stress. If this continues, the NEM stress response system can also become deregulated. The NEM stress response system is how your body deals with stress.
 Gastrointestinal disorders can lead to AFS. Stressors such as chronic disease, chronic infection, malabsorption, maldigestion, toxic exposure from foods, excessive sugar in the diet and general chronic stress are all variables that can lead to AFS.
Gastrointestinal disorders can lead to AFS. Stressors such as chronic disease, chronic infection, malabsorption, maldigestion, toxic exposure from foods, excessive sugar in the diet and general chronic stress are all variables that can lead to AFS.
And vice versa, AFS can be the cause of certain gastrointestinal disorders. Particularly in the more advanced stages of AFS when the adrenal glands are exhausted, the body does not function properly. Adrenal fatigue forces the body into maintenance mode, struggling to maintain balance and wreaking further havoc. AFS symptoms can include dyspepsia, constipation, and diarrhea.
 The inflammatory response is one of the six NEM stress responses, and it is composed of the immune system, the brain, the GI tract and the microbiome. Though acute inflammation is a normal and healthy reaction to threats such as infections or injuries, if it becomes chronic it can devastate the system causing gastrointestinal disorders.
The inflammatory response is one of the six NEM stress responses, and it is composed of the immune system, the brain, the GI tract and the microbiome. Though acute inflammation is a normal and healthy reaction to threats such as infections or injuries, if it becomes chronic it can devastate the system causing gastrointestinal disorders.
Chronic inflammation can occur when the body is exposed to infections or environmental antigens, or due to an autoimmune reaction – when the immune system not only attacks the foreign bodies but also the body’s own tissues.
Some indications of chronic inflammation include frequent infections, pain of unknown origin, food sensitivity, leaky gut, irritable bowel syndrome, inflammatory bowel disease, autoimmune disease, and small intestinal bacterial overgrowth.
Most inflammatory diseases start in the gut, and then spread throughout the rest of the body. When the permeability of gut lining increases and unwanted particles enter the bloodstream, it triggers an immune reaction. This can bring on inflammation, allergies and related diseases. Sometimes toxins that pass through can reach the brain, leading to depression and neurological issues. If this becomes systemic, digestion is compromised and malabsorption ensues, making it more difficult for the body to get the nutrients and energy it needs from food, even if the diet is a healthy one.
The connection between AFS, dysbiosis and inflammation cannot be overlooked. The microbiome actually changes when exposed to stress. The microbiome balance is also implicated in inflammation, as dysbiosis can be the trigger for many inflammatory and metabolic disorders.
Part of the stress response mounted to deal with inflammation is the secretion of cortisol by the adrenal glands. Cortisol helps the body return to a normal, calm state once the inflammation has done its job. But with chronic stress, this response is triggered constantly and cortisol secretion goes into overdrive, eventually exhausting the adrenals. As AFS advances, the body is unable to handle inflammation efficiently. Inflammation can also cause or add to some of the symptoms of AFS, like brain fog, depression, anxiety, hypoglycemia and bloating.
Let us now look at some of the most common gastrointestinal disorders:
Gluten sensitivity has increased significantly in the last few decades. And because their symptoms resemble other gastrointestinal disorders and conditions, they usually go undiagnosed or get mistaken for something else. Gluten, composed of glutenin and gliadin, is the protein found in many types of grains including wheat, spelt, rye, barley, kamut and semolina. It is the protein that makes dough sticky and fluffy.
Gluten is not limited to breads and grains, it’s also added to other types of processed foods, supplements, health and beauty products, and medications.
 So why has gluten sensitivity increased so much? Recently, wheat has been crossbred with other proteins in order to grow faster and survive challenging environmental conditions. It has also been processed in order to become more water-soluble so that it can be easily mixed with other substances. Finally, people nowadays are consuming much larger amounts of wheat than ever before. These factors seem to be contributing to the growing epidemic of gluten sensitivity and intolerance.
So why has gluten sensitivity increased so much? Recently, wheat has been crossbred with other proteins in order to grow faster and survive challenging environmental conditions. It has also been processed in order to become more water-soluble so that it can be easily mixed with other substances. Finally, people nowadays are consuming much larger amounts of wheat than ever before. These factors seem to be contributing to the growing epidemic of gluten sensitivity and intolerance.
When gluten is ingested, it is broken down by a certain enzyme into its components gliadin and glutenin. When these proteins reach the gut-associated lymphoid tissue (GALT), they are assessed for harmfulness. If you are gluten sensitive, the GALT produces antibodies to attack these proteins. If you have Celiac disease, the GALT’s antibodies attack the proteins as well as the enzyme that break down the gluten in the first place.
This enzyme’s other function is to hold together the microvilli in the gut - the little hair-like structures that protrude from the intestinal walls and help absorb nutrients from food. If this enzyme is attacked, the microvilli are compromised and this affects the gut wall integrity, causing leaky gut and the many symptoms that come along with that. In some cases, the antibodies can attack other tissues and organs such as the skin and brain, causing another autoimmune disorder.
Other trigger foods that can cause inflammation in the body include dairy, certain types of oils that contain linoleic acid such as corn, peanut, safflower and sunflower, refined carbohydrates, and simple carbohydrates.
Identifying what foods you are sensitive to and eliminating them from your diet will help your gut heal and calm your inflammation. Because chronic inflammation, AFS, and the NEM stress response are so closely tied, adjusting your diet in this way can be a big step towards healing from adrenal fatigue and reducing the risk of gastrointestinal disorders.
Constipation is when bowel movements occur less frequently than is considered normal or healthy, and when defecation becomes difficult. Though it’s quite normal to have constipation once in awhile, it can carry the risk of complications, including gastrointestinal disorders, if it occurs frequently.
“Normal” is somewhat subjective with regards to how often one goes to the bathroom, though once a day seems to be a healthy average. Anything longer than three days can make passing stool difficult as it hardens and dries up more and more.
Constipation can be very uncomfortable, and going to the bathroom after a bout of constipation can induce straining, which can cause a host of issues such as diverticular disease and hemorrhoids. It can also be quite painful.
Constipation can have many causes, including eating a diet low in fiber, low water intake, too much dairy, irritable bowel syndrome, colon cancer, issues with the nerves or muscles in the colon, inactivity, pregnancy, some medications, hypothyroidism and stress.
In the beginning stages of adrenal fatigue, the body’s low energy state weakens its ability to excrete waste. Digestion slows, and this lack of timeliness makes the waste material accumulate internally, causing toxicity and inflammation. Symptoms of this include brain fog, food allergies and intolerance, pain, anxiety, yeast infections, irritable bowel syndrome, chemical sensitivity and others.
 If left untreated, and as AFS progresses, this only gets worse. By the time adrenal exhaustion is advanced, there is a musculoskeletal system breakdown, including the breakdown of the collagen structure of internal organs. The GI tract motility and contraction are compromised, causing further constipation and indigestion. Acid production is not high enough to break down food and the body is unable to assimilate nutrients, depleting the cells.
If left untreated, and as AFS progresses, this only gets worse. By the time adrenal exhaustion is advanced, there is a musculoskeletal system breakdown, including the breakdown of the collagen structure of internal organs. The GI tract motility and contraction are compromised, causing further constipation and indigestion. Acid production is not high enough to break down food and the body is unable to assimilate nutrients, depleting the cells.
The thyroid also slows down to reduce metabolic rate and conserve energy, causing further fatigue and constipation. The lowered ability for clearance of waste products from the body and the buildup of toxicity affects liver and kidney function. If constipation becomes severe and persistent, enemas are sometimes required to empty bowels. Probiotics can also help improve gut flora and regulate bowel movements and help prevent gastrointestinal disorders.
Diarrhea, as uncomfortable as it can be, is not usually a serious problem unless it becomes persistent – causing dehydration and loss of electrolytes. Chronic diarrhea can also be indicative of another, more serious condition. If diarrhea is accompanied by other symptoms such as blood or mucus in the stool, fever, severe pain or weight loss, this can be indicative of a deeper issue and you should consult with your primary medical doctor.
The most common causes of diarrhea are intestinal viruses, bacteria (food poisoning) or eating food one is sensitive/allergic to. Other causes include gastrointestinal conditions and disorders such as Crohn’s disease and IBS, hyperthyroidism, malabsorption, overuse of alcohol, certain medications, diabetes and some types of cancer. Usually, diarrhea not associated with other conditions, can be alleviated with over-the-counter medications, if even that. Most people will feel better eating lighter meals, resting and drinking fluids to stay hydrated.
For those who suffer from AFS, constipation will be more prevalent than diarrhea, though severe diarrhea can be indicative of an advanced stage of adrenal exhaustion. It is very important to stay hydrated to maintain fluid balance. Digestive enzymes or bentonite clay may also help to regulate and normalize bowel movements and help prevent gastrointestinal disorders.
As mentioned, one of the functions of the GI tract is to act as a barrier preventing toxins, undigested food particles, microbes or other foreign bodies from entering the bloodstream. In a healthy state, the junctions between the mucosal cells that form the lining of the gut are tight enough to only let through the nutrients from food that the body needs. With leaky gut, the lining is compromised, leaking out particles that are treated as pathogens by the immune system, which attacks them, causing inflammation.
Symptoms of leaky gut include pain, fatigue, anxiety, depression, insomnia and brain fog. Furthermore, leaky gut can trigger other conditions such as autoimmune disease, allergies, food sensitivities, acne, candida, PMS and IBS.
 One of the main causes of leaky gut is dysbiosis. Age and stress also contribute, and AFS has a two-way relationship with leaky gut. As mentioned, stress increases the permeability of the gut, and the resulting immune response and inflammation affects the balance of the microbiome.
One of the main causes of leaky gut is dysbiosis. Age and stress also contribute, and AFS has a two-way relationship with leaky gut. As mentioned, stress increases the permeability of the gut, and the resulting immune response and inflammation affects the balance of the microbiome.
If you suffer from leaky gut, it is important to eliminate inflammatory foods from your diet, reduce exposure to toxins and begin a nutritional and supplementation plan that restores balance to your microbiome, which will seal up leaks naturally. Probiotics, digestive enzymes, glutamine, and licorice root are all supplements that can help heal a leaky gut and prevent gastrointestinal disorders.
IBS is a very common syndrome that affects twice as many women as it does men. Its symptoms include diarrhea, constipation, abdominal pain, bloating, lower back pain, loss of appetite, nausea, headaches, joint pain, bad breath, frequent urination, anxiety and fatigue. As it has no recognized pathology, a process of elimination usually determines IBS, where other similar conditions are ruled out by lab tests. In essence, it is a condition where the GI tract is in a state of irritation.
Stress plays a huge role in IBS, though other factors can contribute, such as antibiotic use, depression, anxiety, infections, dysbiosis, immune system problems, hormonal imbalance and adrenal fatigue. As previously mentioned, with advancing AFS, the body is slowing down its metabolism in order to conserve energy, and gut movement is also slowed down. This causes food to move through the system slower than usual, causing constipation, with a possibility of diarrhea once in awhile, adding to the irritation of the gut and worsening the symptoms of IBS. Anti-inflammatory supplements such as omega 3 fatty acids, and quercetin are beneficial to help IBS. Peppermint oil and fiber may also help with the diarrhea aiding in preventing Gastrointestinal disorders.
Small Intestinal Bacterial Overgrowth (SIBO) is a growth of the bacteria in the small intestine beyond the healthy limit, in healthy people, these bacteria are actually more commonly found in the colon, not the small intestines. SIBO has similar symptoms to IBS. In fact, it’s common for people to suffer from both conditions simultaneously. Some of these symptoms include bloating, diarrhea, abdominal pain, constipation and gas.
SIBO can develop due to a number of causes, such as a diet high in sugar, refined carbohydrates, and alcohol. Scars from Crohn’s disease or diverticular (sacs or pockets) that form in the wall of the small intestine can also catch and collect bacteria, instead of letting it pass through to the colon. Some medications, like antibiotics, also disrupt the balance of the gut flora in the small intestine, possibly leading to gastrointestinal disorders.
Other infections such as those from candida and Lyme disease, as well as the Epstein Barr virus, can weaken the immune system, allowing the bacteria overgrowth. Stress and aging are other factors. If left untreated, SIBO can become debilitating with chronic diarrhea, weight loss and malabsorption. AFS can aggravate or even trigger SIBO as it has a direct effect on gut flora balance. Fiber, prebiotics, starches, and gums can help with SIBO.
 Diverticular disease occurs when pockets, called diverticula, develop in the lining of the large intestine. At that point, this condition is called diverticulosis and it is not particularly dangerous; neither does it have obvious symptoms. These diverticula can develop due to pressure from gas, solids or liquids on weak areas of the bowel walls, and from straining during defecation.
Diverticular disease occurs when pockets, called diverticula, develop in the lining of the large intestine. At that point, this condition is called diverticulosis and it is not particularly dangerous; neither does it have obvious symptoms. These diverticula can develop due to pressure from gas, solids or liquids on weak areas of the bowel walls, and from straining during defecation.
Sometimes the diverticula become infected and inflamed when they collect waste and bacterial build-up. This turns the diverticulosis to diverticulitis, which can become a very uncomfortable condition with symptoms including diarrhea alternating with constipation, pain and tenderness in the lower abdomen, chills, or fever.
Another possible complication is when blood vessels near the diverticula are continuously exposed to injury, causing diverticular bleeding.
Complications can arise for about 20% of those with diverticulosis, and the risk increases with age.
More serious issues can occur if a tear develops in the intestinal wall, which would allow waste to leak out into the abdominal cavity, possibly causing infections, abscesses and/or obstructions. Infections can also cause scar tissue to form in the colon, creating blockage. A complete blockage would require emergency surgery.
Diverticulitis can also produce fistulas - connections between two organs. In this case, the most common is a fistula between the bladder and the colon.
Though diverticulosis is very common with age, affecting almost all Americans over the age of 80, it is still important to try your best to prevent or mitigate it as much as possible. The first thing to keep in mind is to avoid straining and constipation. Dietary fiber plays a central role in keeping things moving along regularly. Exercise is also great for healthy bowel movement.
Because constipation usually follows AFS, and in later stages the bowel movements slow down to such a degree that constipation becomes chronic, it is advisable to take care of adrenal fatigue in order to avoid the development of diverticular disease. It is also important to eat a healthy diet, get enough rest and sleep, and do the right kind of exercise for your condition.
If you have AFS and a gastrointestinal disorder, you need to be careful with the changes you make to your diet and supplementation. The reason for this is that some of the recommended supplements and health plans for one condition may adversely affect the other.
For example:
 Because trying to navigate adrenal fatigue on your own can actually worsen your condition and add to the symptoms of the gastrointestinal disorder you may suffer from, it is highly recommended that you seek the right guidance from a medical professional experienced in both.
Because trying to navigate adrenal fatigue on your own can actually worsen your condition and add to the symptoms of the gastrointestinal disorder you may suffer from, it is highly recommended that you seek the right guidance from a medical professional experienced in both.
The first important step would be to get your microbiome back to a healthy state. A holistic recovery plan will include nutritional coaching to make sure you are getting the right kind of nutrients, eliminating inflammatory foods and strengthening your gut flora without causing adrenal crashes. Your nutritional plan may include supplements, herbs and enzymes to help with both conditions. Once gut flora is in balance, many of the symptoms and inflammations will subside on their own. And because digestion is enhanced, you will be able to get enough nutrients and energy from food again, reducing fatigue, brain fog and other symptoms.