 The widespread and common use of natural progesterone (hereafter referred to as progesterone) for hormone balance and menopausal symptoms, especially estrogen dominance, has potentially important negative clinical implications when used by those with a weak body – such as those with Adrenal Fatigue Syndrome (AFS). Excessive progesterone can cause imbalances with many other hormones in the body, making progesterone side effects and toxicity both serious and hard to identify. Extreme caution should be used when considering progesterone, and this article details why.
The widespread and common use of natural progesterone (hereafter referred to as progesterone) for hormone balance and menopausal symptoms, especially estrogen dominance, has potentially important negative clinical implications when used by those with a weak body – such as those with Adrenal Fatigue Syndrome (AFS). Excessive progesterone can cause imbalances with many other hormones in the body, making progesterone side effects and toxicity both serious and hard to identify. Extreme caution should be used when considering progesterone, and this article details why.
Although a natural compound, inappropriate use of natural progesterone can worsen sub-clinical liver congestion, trigger multiple progesterone side effects and toxicity symptoms, and worsen adrenal fatigue. Abrupt withdrawals can also result in adrenal crashes and potentially cause irreparable damage. In the extreme, it can lead to a state that is known as brittle adrenals, where the body exhibit fluctuating symptoms resembling both extremes of cortisol level (too high and too low). Fortunately, this affects only a small number of AFS sufferers, but if you are one of them, life is downright miserable.
When a patient complains of fatigue or menopausal discomfort to a doctor, the typical medical workup consists of investigating thyroid function, anemia, and metabolic issues. Female and male hormones are often investigated by way of saliva or serum laboratory tests. Functional or alternative medicine practitioners commonly obtain diurnal cortisol, estrogen, progesterone, DHEA, and testosterone as baseline hormonal information through laboratory studies. While most laboratory studies are normal, DHEA and progesterone level are often low.
At this point, patients are told they have a hormonal imbalance and will need natural hormone replacement that can include estrogen, progesterone, and sometimes also testosterone. Typically, patients are also given thyroid support, vitamin C, vitamin B, glandulars, herbs, DHEA and pregnenolone at the same time. Such a multi-hormone approach is designed to replace diminishing hormones the body may be experiencing. The key to success or failure of such an approach lies largely in the dosage and delivery system of the hormone replacement. Some doctors tend to be quite aggressive, while others are more conservative.
This symptom patching “shotgun” approach often produces positive results in the beginning. For most sufferers, the fatigue of unknown origin improves. Anxiety tends to improve as well, due largely to progesterone effects. There is a general increase in energy, with fewer energy slumps. Sleep tends to improve from natural progesterone’s sedative effect. A sense of calm returns. Symptoms consistent with estrogen dominance, include: PMS, water retention, brain fog, anxiety, and heavy menses. Because progesterone opposes estrogen, these symptoms may subside if a person is indeed in estrogen dominance. For some, the benefit is significant and remarkable. They are given what appears to be a new lease on life. For the first time in years, many report feeling vibrant and energetic with a positive outlook on life.
Unfortunately, for most this honeymoon does not last indefinitely. While some people continue to do well on such a program, many report this multiple hormone replacement approach gradually loses effectiveness over time. Those who are already in advanced stages of adrenal fatigue prior to beginning such program are particularly vulnerable. Over months or years, there is a slow but gradual loss of the positive clinical outcome as compared to the initial benefit. As time progresses, many return to their doctor for more help.
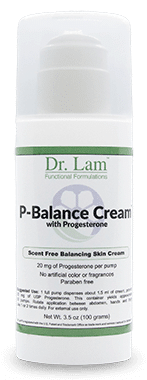
 To achieve the same effect, physicians generally recommend more hormone replacement by way of stronger dose. Thyroid replacement, for example, progresses over time from primarily a low dose T4 replacement program, to a combination of T4/T3 replacement, then finally to a high dose strong T3 replacement. In like manner, the dosage of transdermal natural progesterone may start at a 20 mg dose, but ultimately can be much more. Sufferers may be switched to other delivery systems, such as sublingual forms, to enhance absorption. Oral progesterone favored by most physicians may start at 100 to 200 mg per day but can be increased significantly over time.
To achieve the same effect, physicians generally recommend more hormone replacement by way of stronger dose. Thyroid replacement, for example, progresses over time from primarily a low dose T4 replacement program, to a combination of T4/T3 replacement, then finally to a high dose strong T3 replacement. In like manner, the dosage of transdermal natural progesterone may start at a 20 mg dose, but ultimately can be much more. Sufferers may be switched to other delivery systems, such as sublingual forms, to enhance absorption. Oral progesterone favored by most physicians may start at 100 to 200 mg per day but can be increased significantly over time.
Is this the right strategy? Let us take a step back and understand what progesterone actually do first physiologically in our body.
Progesterone is one of the major female hormones, along with estrogen, produced by the ovaries. These two hormones work together to regulate a woman's menstrual cycle. Natural progesterone has an identical chemical structure to that made in a woman's body by the ovarian corpus luteum. It is not the same as the synthetically derived progesterone referred to as progestins, which are chemically modified and recommended by conventional doctors. Progestins have the opposite effect to natural progesterone. They are used as morning after pills to trigger abortions and in birth control pills. To be clear, this discussion deals only with natural progesterone.
Progesterone is a calming hormone. It opposes estrogen. It is known as a lipophilic hormone. In other words, it “loves fat” such as adipose tissues. It tends to stay in areas of the body where such tissue is prominent, such as the abdomen and organs. All steroid hormones love fat, including estrogen and testosterone. However, progesterone loves fat the most out of them all. When hormones are trapped in fat, the body can only metabolize a limited amout a day. One study reported that it took four months for women to clear half of the 42 mg per day dose they used for 40 days. Excessive progesterone therefore may lead to accumulation in the body. This accumulation can have negative effects.
Natural progesterone is available in pill form, as a topical gel, vaginal gel, sublingual spray, or as an oil. Under normal conditions in healthy individuals, 20 to 30 mg a day for women and 6 to 10 mg a day for men is considered a physiological amount. There usually are little, if any, progesterone side effects.
However, the same cannot be said for those with adrenal fatigue or those who take high doses. Many in advanced stages of adrenal fatigue cannot tolerate natural progesterone, even in small amounts. Healthy women on high dose progesterone can develop toxicity symptoms over time.
This occurs for many reasons, including progesterone’s own intrinsic properties as well as it being a precursor to many other hormones. A flow-through to other hormones includes estrogen and its metabolites, testosterone and its metabolites, DHEA, aldosterone, and ultimately, cortisol can occur.
To understand this, first it is helpful to know how natural progesterone should be used and the many ways its inappropriate use can be problematic.

Estrogen dominance exhibits symptoms such as: water retention, anxiety, breast tenderness, spotting, dizziness, hot flashes, fatigue, headaches, nausea, and irritability. These symptoms may become worse when first beginning natural progesterone.
Because estrogen and progesterone receptor sites are very similar at the cellular level, estrogen receptor sites can ‘wake up’ when occupied by progesterone molecules, enhancing the action of estrogen for a short period of time. It is easy to draw the conclusion that this is a sign the body is responding well to the progesterone, and sufferers are encouraged to “brave through” this estrogenic effect, as it is supposed to eventually go away. However, ignoring the underlying dysfunction when alerted by the body is a recipe for disaster.
Fortunately, this is usually short lived for most, lasting a few days to a few weeks. For some, however, this is just the beginning of their nightmare. The more advanced the adrenal fatigue, the higher the risk of this phenomena. Clinically, this is more prevalent in those with sensitive or thin bodies as well. It points to underlying receptor site dysfunction or liver congestion.
If there is concurrent stress that activates the body’s stress handling HPA hormonal axis, as is the case in adrenal fatigue, natural progesterone can make matters worse. In other words, if your body’s ability to deal with stress is compromised, progesterone does not improve symptoms.
Stress triggers the body to put the adrenal glands on overdrive to increase output of the anti-stress hormone cortisol. This is what happens in the early stages of adrenal fatigue. Cortisol, unfortunately, competes for progesterone receptors. The higher the level of stress experienced, the more cortisol the adrenals produce. This means that those receptor sites may be occupied by cortisol rather than progesterone. This leads to reduced progesterone availability to cells. Also, progesterone is a precursor to the synthesis of cortisol. In times of stress, progesterone may be shunted to make more cortisol, resulting in less progesterone being available to the cell as well. Multiple mechanisms therefore can result in lower than normal levels of free progesterone during stress, while estrogen dominance symptoms rise. This may be reflected in laboratory test showing lower than normal progesterone levels in absolute terms, or a low progesterone to estrogen ratio. Physicians not alert to this lowered progesterone level in times of stress may prescribe progesterone in their best intention to increase the progesterone level.
 In other words, if you are not managing your stress levels properly, the natural progesterone cream you are currently using may not be effective. Physicians may then prescribe cortisol. Sometimes it can be helpful, but cortisol has its own set of problems, including tolerance, resistance, dependency and withdrawal issues. In addition, cortisol can also lead to loss of magnesium and potassium, further complicating the clinical picture and triggering electrolyte imbalances. Menstrual bleeding may increase as estrogen dominance symptoms worsen. High dose progesterone is often prescribed to control or offset estrogen overload and excessive bleeding. This can trigger a host of side effects and toxicity issues.
In other words, if you are not managing your stress levels properly, the natural progesterone cream you are currently using may not be effective. Physicians may then prescribe cortisol. Sometimes it can be helpful, but cortisol has its own set of problems, including tolerance, resistance, dependency and withdrawal issues. In addition, cortisol can also lead to loss of magnesium and potassium, further complicating the clinical picture and triggering electrolyte imbalances. Menstrual bleeding may increase as estrogen dominance symptoms worsen. High dose progesterone is often prescribed to control or offset estrogen overload and excessive bleeding. This can trigger a host of side effects and toxicity issues.
While a one-time overdose of natural progesterone cream is rare (except in people who are very weak or sensitive), the body’s ability to handle excessive progesterone can be overwhelmed over a long period of time. Progesterone side effects and toxicity are eventually triggered due to a cumulative saturation effect of progesterone in the cells. The common belief that natural progesterone is “harmless”, even in high doses, is quite naïve.
Stopping progesterone abruptly without proper titration can also be problematic. Many have experienced a huge wave and additional surging of progesterone as it comes out of our tissues soon after abrupt withdrawal. It is a very unpleasant experience. An aldosterone surge can occur that leads to electrolyte imbalances – which in severe cases requires hospitalization.
 Progesterone side effects include many unpleasant symptoms and dangerous conditions.
Progesterone side effects include many unpleasant symptoms and dangerous conditions.
About thirty percent of users experience headache, fifteen percent experience dizziness, and twenty percent experience back or joint pain. Other symptoms include increased sweating, nervous tremors, and speech disorders.
Excess progesterone regulates estrogen receptors down. With fewer estrogen receptors, the brain cannot respond to the hormone in the normal way. Its response to estrogen is needed for serotonin production. While this one of the many progesterone side effects is desirable for those who have insomnia, and many use natural progesterone as a sleep-aid as a result, the lack of serotonin can also cause depression.
Twenty-five percent of patients experience some breast tenderness that tend to subside with time, and ten percent experience vaginal discharge. Twenty percent of women will experience abdominal pain and a small number experience bloating, diarrhea and nausea. These GI symptoms are often attributable to activation of systemic candida.
Excess progesterone can block the conversion of testosterone to DHT causing a lowered sex drive. This primarily happens to men.
Water retention is likely caused by excess conversion to deoxycortisone, a mineralocorticoid made in the adrenal glands which causes water retention. Those who are prone to the estrogenic effect may also be susceptible to this.
Excessive progesterone can also lead to the increase in androgen production and ultimately increase estrogen as the body shunts the excessive progesterone to these other hormones. Estrogen dominance symptoms can emerge, both in males or females.
Cellular immunity is an important part of our overall immune system that protects us from viral infections. This is in contrast to bacterial infections that are attacked by macrophages or neutrophils from the innate arm of the immune system. Excessive progesterone suppresses the cellular immune system involving T and B lymphocytes. Upper respiratory infections increases, with more cold and flu-like symptoms.
Miscellaneous progesterone side effects can include:
Topical progesterone provides a seamless delivery of the hormone into the bloodstream. This delivery method prevents the complications associated with oral progesterone replacement, which gets processed through the gastrointestinal (GI) tract and liver. Because over 80 percent of natural progesterone is metabolized by its first pass through the liver, a much higher dose is required for oral delivery as compared to topical methods.
 Anyone with liver pathology either clinical or sub-clinical, is at risk with high dose progesterone. Those who have normal liver function according to laboratory tests, but who have sub-clinical and possibly unrecognized liver congestion, are also at risk for progesterone side effects.
Anyone with liver pathology either clinical or sub-clinical, is at risk with high dose progesterone. Those who have normal liver function according to laboratory tests, but who have sub-clinical and possibly unrecognized liver congestion, are also at risk for progesterone side effects.
While topically progesterone is better compared to oral for those with hepatic constraints, it is not without its own problems. When progesterone cream is administered through the skin, most of it goes into the bloodstream, but some also builds up and accumulates in the subcutaneous fat layer. With long term use, a cumulative saturation effect can result. The body’s self-regulation process is automatically activated, and the body initiates a down-regulation of progesterone receptors, making them more resistant to activation. This is the body’s way of rejecting excessive progesterone in the system. Effectiveness of the progesterone is therefore reduced. Unfortunately, precursors of progesterone such as pregnenolone are shunted to make DHEA, testosterone, and estrogen instead, thus creating a different set of problems as these other hormone levels rise.
Instead of lowering natural progesterone, a frequent clinical mistake is to do just the reverse – increase progesterone in order to “normalize” laboratory values.
As the body is subjected to more progesterone, the liver has to work harder and harder, as it has the burden of having to metabolize and detoxify excessive amounts of that hormone. In turn, this puts more stress on the adrenal glands. This vicious cycle only makes matter worse.
As mentioned above, progesterone is a precursor to many other important hormones. Excessive Progesterone side effects over time can trigger imbalances of other hormones including estrogen, testosterone, aldosterone, and cortisol by a variety of mechanisms. These include shunting, “stealing”, and down-regulation processes. Those with pre-existing adrenal fatigue in advanced stages are most at risk due to already weakened pathway integrity in the adrenals where they are regulated.
Clinical symptoms that arise from excessive Progesterone side effects can include hyper adrenal function similar to Cushing’s Disease. Symptoms of high cortisol include: hypertension, insomnia, memory loss, feeling hot, edema, irritability, anxiety, muscle weakness, glucose intolerance, increased thirst, and increased urination. Fortunately, this is rare. Such hyper-cortisol symptoms can be fleeting, often lasting only for a short time.
The body’s self regulatory system usually will be triggered to rebalance the hormones and return itself to the normal state. For some, that works. For a small number of people, the body overshoots and enters a state of low cortisol output, similar to Addison’s Disease. This low cortisol results in symptoms that include: extreme fatigue, lymph stagnation, salt craving, low energy, low blood pressure, nausea, vomiting, diarrhea, abdominal pain, and muscle pain. These symptoms also can be fleeting in nature, only lasting a short time. Then the body reverts to the previous high cortisol state. The body is constantly in a state of extreme fluctuation like a yo-yo.
 This is clinically referred to as brittle adrenals. The pattern resembles that of a roller-coaster ride that can occur multiple times during the day. The body is drained nutritionally and hormonally in its effort to effect self rebalancing. Over time, the body is unable to adjust and becomes destabilized. The HPA axis by this time is dysregulated. The body has lost its ability to self regulate and fine tune itself in terms of cortisol output. It is like taking a shower with alternating hot and cold water that is beyond one’s control – but never the desired warm water.
This is clinically referred to as brittle adrenals. The pattern resembles that of a roller-coaster ride that can occur multiple times during the day. The body is drained nutritionally and hormonally in its effort to effect self rebalancing. Over time, the body is unable to adjust and becomes destabilized. The HPA axis by this time is dysregulated. The body has lost its ability to self regulate and fine tune itself in terms of cortisol output. It is like taking a shower with alternating hot and cold water that is beyond one’s control – but never the desired warm water.
Ultimately, such extreme swings in cortisol output also destabilizes the body’s metabolic pathways. Blood sugar regulation becomes problematic, and electrolyte imbalance follows along with fluid dysregulation. Like a light switch that has been flipped on and off multiple times continuously – eventually it breaks. The body is unable to adjust in a timely manner to provide the cushion to handle the extreme hormonal variance. The effort drains the body and resilience is reduced. Such hormonal swings between two extremes, the high cortisol state and the low cortisol state, is a nightmare in the making. This is similar to brittle diabetes, where a person’s blood sugar can quickly go from high to low for no apparent reason.
With the phenomena of brittle adrenals, sufferers are unable to conduct a normal life. Swings between anxiety and depression, low appetite and hunger, low sodium and low potassium, constipation and diarrhea, and low and high magnesium are just some of the vacillating states experienced multiple times during the day. When the cortisol is high, one resorts to using phosphatidylserine, antihistamine, and anti-inflammatory drugs – bringing some relief. When the cortisol is low, salt water, electrolyte replenishment, and vitamin C can be helpful. Unfortunately, these are simply symptomatic patches and the cycle repeats itself multiple times during the day.
Ultimately, this unrelenting roller coaster ride renders the body to a state of extreme weakness. Toxic reactive metabolite built-up can lead to hypersensitivity reactions, congested extracellular matrix, and receptor site damage. This process usually starts slowly but tend to gather steam as the body becomes weaker over time. Vital signs can become unstable. Multiple and frequent visits to the emergency room become the norm, often only to be told all is well and sent home to “relax”. Sufferers are eventually bed-bound, because the liver and extra cellular matrix will become congested over time. Overall, the body becomes flooded in a sea of toxin quite toxic with reactive metabolite overload (RMO). The body’s defense is to activate the reactive metabolite response (RMR) as a last resort to reduce toxic metabolites. Multiple organs and systems are put on overdrive to remove as much reactive metabolites as quickly as possible. Intracellular communications and extracellular matrix congestion and burden increases. Inevitably, RMR will lead to additional reactive metabolites being generated. As the body’s toxic load increases, it eventually enters a positive loop of ever reducing stability. Unless multiple laboratory cortisol levels are being drawn and tracked multiple times throughout the day to track the fluctuating burden on the adrenals, doctors are universally lost to understand and eventually give up.
 This brittle adrenal phenomena is not exclusively seen in those with progesterone overload, although it seems to be most common. Taking a step back, it is seen most commonly in a body that is weak to begin with at the foundation level, though it may not clinically evident. Other triggers of brittle adrenal include abrupt withdrawal from natural progesterone, inappropriate use of steroids, vaccine toxicity, rampant systemic inflammation, stealth infections, and end stage AFS.
This brittle adrenal phenomena is not exclusively seen in those with progesterone overload, although it seems to be most common. Taking a step back, it is seen most commonly in a body that is weak to begin with at the foundation level, though it may not clinically evident. Other triggers of brittle adrenal include abrupt withdrawal from natural progesterone, inappropriate use of steroids, vaccine toxicity, rampant systemic inflammation, stealth infections, and end stage AFS.
Needless to say, those with brittle adrenals or symptoms resembling this must quickly seek professional help. Most conventional physicians are at a loss as far as knowing what to do. Recovery is possible with a comprehensive plan to stabilize the body’s adrenals, slowly returning cortisol output into balance and reestablishing feedback loops so the body can self regulate. Reactive metabolite volume must be kept under control, while extracellular matrix decongested. This is a very slow process that requires clinical skills, patience, understanding, and some trial and error, because the body is very unstable. The slightest wrong move can worsen the situation, even in the best of clinical hands.
While the use of natural progesterone has its place in rebalancing the body’s hormones, caution is advised when a stage of adrenal fatigue exists. The more advanced the state of adrenal fatigue, the bigger the risk.
Progesterone side effects, toxicity, and brittle adrenals are all very undesirable outcomes that can surface. The proper dosage, frequency, delivery system, and timing must be carefully factored in prior to using progesterone. An exit strategy should be in place beforehand when adrenal fatigue is present. Laboratory tests are unfortunately not helpful in this situation and can be misleading. Close clinical monitoring is required.
Address Progesterone Side Effects and Nourish Adrenals