 No matter her age, a woman’s hormones must work in harmony in order for her to have good health. If one hormone is out of balance, the harmony quickly goes awry. Female hormone imbalance symptoms will then make themselves known. The symptoms that come with this kind of imbalance can be very similar to those seen in adrenal fatigue.
No matter her age, a woman’s hormones must work in harmony in order for her to have good health. If one hormone is out of balance, the harmony quickly goes awry. Female hormone imbalance symptoms will then make themselves known. The symptoms that come with this kind of imbalance can be very similar to those seen in adrenal fatigue.
It’s common for women’s hormones to fluctuate throughout their monthly cycle. Normally, this cycle will complete itself and hormone levels will return to normal. However, at other times female hormone imbalance symptoms may appear for a variety of reasons.
One of the most typical reasons for this kind of imbalance is menopause. Usually, women begin enduring menopause symptoms in their late 40s or early 50s. The most frequent kind of treatment for these symptoms is providing synthetic hormone replacement therapy to control the symptoms. Some women as young as 18 may need some kind of medical intervention to deal with female hormone imbalance symptoms.
Prescribing oral synthetic estrogen and progestin is the usual approach to treating these symptoms. However, there are alternative medicine interventions that can be used and are better for the women in the long run.
Why not continue the traditional treatment with oral synthetic estrogen and progestin? Research has shown oral estrogen will often lead to increased inflammation and progestin often brings on atherosclerosis. So as well as relieving women of female hormone imbalance symptoms, these two hormones that are frequently prescribed together as treatment for hormonal imbalance can bring on unwanted results.
The increased inflammation brought on by the oral estrogen often used in traditional hormone replacement therapy can become a major problem. Chronic inflammation is seen more and more often in our stress-filled world already. This source of continuing stress leads to activation of the body’s natural stress responses, resulting in more stimulation of the body’s immune system. In addition, this prompts activation of the adrenal glands to secrete more cortisol to fight the stress effects.
Continuing stress can lead to the immune system getting out of control. Inflammation results again.
The specific connections between female hormone imbalance symptoms and related conditions aren’t clearly known. What is known is that the levels of chronic inflammation typically rise during and after menopause - when these changing levels are most frequent.
These hormonal changes that lead up to symptoms of menopause also add to the kind of weight gain that comes around the middle of the body. These kinds of fat cells create extra cytokines and C-reactive protein that increases inflammation.
This chronic inflammation also is affected by, and in turn affects the neuroendocrine system and oxidative stress.  Likewise, metabolic dysregulation seems to be one result of the stress we experience on a daily basis. This leads to increased inability to resolve inflammation, which leads to more aging. Aging then increases the risk of hormone imbalance. As inflammation becomes chronic, it activates the immune response - which then has a negative effect on tissue.
Likewise, metabolic dysregulation seems to be one result of the stress we experience on a daily basis. This leads to increased inability to resolve inflammation, which leads to more aging. Aging then increases the risk of hormone imbalance. As inflammation becomes chronic, it activates the immune response - which then has a negative effect on tissue.
This chronic inflammation, an insidious symptom of imbalanced female hormones, may be the basis of all chronic illnesses. Autoimmune diseases fall into the category of chronic illnesses.
Living longer gives rise to an increase in autoimmune diseases. People are living longer - as shown by a 60 percent decrease in the death rate in the U.S. from 1935 to 2010. Currently, the National Institutes of Health report 23 million people living with these diseases. Other sources place the number at up to 50 million.
Many of these autoimmune diseases we don’t even have names for, but all of them begin with inflammation. The same inflammation that comes with imbalanced levels of estrogen, progesterone, and testosterone. Increasing longevity means more years of living with the female hormone imbalance symptoms, and therefore increasing symptoms of Adrenal Fatigue Syndrome (AFS).
Over and over again, the conditions and symptoms described when female hormone imbalance symptoms are reported closely resembled the symptoms of AFS. These symptoms become another source of stress. When the body is under stress, which is a chronic condition in our world today, it responds with the natural activation of the hypothalamic-pituitary-adrenal (HPA) axis.
In this process of activation, numerous hormones are secreted as the body prepares to fight against or flee from the stressor. Cortisol is one of the main hormones secreted by the adrenals to fight the effects of stress on the body. As stress continues, the adrenal glands reach the point of exhaustion. They can no longer secrete cortisol to fight stress.
Once the point of adrenal gland fatigue is reached, their ability to produce and keep in balance other hormones, such as estrogen, progesterone, and testosterone is significantly reduced. When these female hormone imbalance symptoms occur (and, yes, testosterone is found in females too), these are signals from the body that needed support is missing.
When women begin experiencing symptoms like abnormal weight gain around the middle of the body, fluctuations in blood pressure, cravings for certain foods, feeling tired and wired, not being able to sleep well or at all, fuzzy thinking, and low libido, AFS may be a reason. These symptoms will worsen with time if stress continues. Ultimately, physical breakdown on a system-wide basis will occur.
Food cravings seen in AFS and in women suffering from imbalanced hormones can lead to women eating the wrong foods. Ingesting the kinds of foods (sweets or salty foods for example) that often are craved can lead to detrimental effects on the gut microbiome.
 Although understanding the importance of the gut system in the United States is relatively new, the concept of gut health, the microbiome, and their importance have been known for centuries. To show the extent of this importance, keep in mind the gut has ten times more microbes than there are cells in the human body. Also, there are one hundred times more genes in the microbiome than in the human genome. This makes the microbiome in our gut possibly the largest organ system in the body.
Although understanding the importance of the gut system in the United States is relatively new, the concept of gut health, the microbiome, and their importance have been known for centuries. To show the extent of this importance, keep in mind the gut has ten times more microbes than there are cells in the human body. Also, there are one hundred times more genes in the microbiome than in the human genome. This makes the microbiome in our gut possibly the largest organ system in the body.
The gut microbiome plays an important role in keeping hormones in balance. An essential enzyme that helps metabolize estrogen is produced there. The complete set of bacterial genes that produce this enzyme is called the estrobolome. These gut flora can make you likely to have more than enough estrogen or likely to have too little. This makes the gut essential in keeping hormones balanced.
Since the kinds of foods we eat affect the gut system, when there is an increase in sugar consumption due to cravings seen in AFS and in female hormone imbalance symptoms, our gut system is among the first to feel it. Without good nutrients, the gut (along with the rest of the body) begins breaking down. With up to 80 percent of our immune response tied to our gut, impaired intestinal functioning leads to many chronic illnesses.
With all of the information we have regarding female hormone imbalance symptoms and AFS, we know that the entire body system must be considered when confronted with these conditions. Most conventionally trained physicians become specialists and divide up a patient’s body, treating only what lies within their specialty area. However, our bodies’ systems work in communication with each other, affecting each other’s functioning and being affected by every other system in our bodies.
According to research and numerous conferences held recently, it appears that conventional medicine may be going in the direction of the interrelationship of systems in the body. This is the viewpoint of the NeuroEndoMetabolic (NEM) approach to stress response. All systems of the body work in interaction with all other body systems to respond to changes in any given system. What affects one, affects the others.
When the hypothalamic-pituitary-adrenal (HPA) axis is activated by stress, the hormone response to stress is also activated. Cortisol is secreted by the adrenals, thyroid hormones are released or not released, and fatigue often results. This decreases the desire for sex.
Symptoms develop in situations of adrenal fatigue that are much the same as seen in female hormone imbalance symptoms. Increased PMS symptoms, low libido, breast diseases, irregular menses, loss of sleep, and others.
With continuing stress, the thyroid function slows down, leading the body to conserve energy by reducing metabolic rate. This leads to warning signs of metabolic dysregulation such as craving for sugar, gaining weight around the abdomen, and, ultimately, development of type 2 diabetes. Along with these symptoms can come insomnia, anxiety, depression, and more foggy cognitions.
 This is an indication of the triggering of the neuro-affective response as part of the NEM model. Also with symptoms of a dysfunctional metabolic system comes a triggering of the inflammatory response. The gut microbiome begins working ineffectively and more inflammation results.
This is an indication of the triggering of the neuro-affective response as part of the NEM model. Also with symptoms of a dysfunctional metabolic system comes a triggering of the inflammatory response. The gut microbiome begins working ineffectively and more inflammation results.
Over and over again, the effects of inflammation are being studied and reported. Chronic inflammation brought on by stress, sleep disruption, foods we eat, metabolic irregularities, and problems in the gut microbiome appears to be involved in a myriad of significant physical complications. This emphasis on inflammation goes hand-in-hand with the AFS and NEM models for stress response.
We specialize in helping people get control over their stress response because that has a domino effect on the rest of their health. A strong and balanced NEM and strong and healthy adrenals can help your body better adapt to stress. They also play a big role in overall hormone balance.
 Common female hormone imbalance symptoms and adrenal fatigue share striking similarities. Like with AFS, hormone imbalance can strike women of nearly any age - from 18 on. Many things influence hormone levels in women: age, pregnancy, some medications, poor diet, and lack of exercise.
Common female hormone imbalance symptoms and adrenal fatigue share striking similarities. Like with AFS, hormone imbalance can strike women of nearly any age - from 18 on. Many things influence hormone levels in women: age, pregnancy, some medications, poor diet, and lack of exercise.
One major factor can be seen as causative in both the female hormone imbalance symptoms and AFS. That common major factor is stress.
Hormone imbalance in women is much more common than once thought. Up to 80 percent of women may experience female hormone imbalance symptoms in their lifetime. These symptoms can be seen well in advance of menopause, during the time of menopause, and after menopause.
Even though these female hormone imbalance symptoms may be clear, they’re not easy to fix. Plus, they ravage your emotional, physical, and reproductive health.
Normally, women have an approximately 28 day menstrual cycle in which hormones play an important part. A normal balance among the female hormones readies the body to release an egg for fertilization and the uterus for optimum implantation of the fertilized egg. If the egg is not fertilized, it and the lining of the uterus are expelled during the several days at the end of this normal cycle. Then it all starts over.
During this normal cycle, even balanced hormones lead to some of the female hormone imbalance symptoms. However, normally these symptoms last only a short while. This balance is necessary for a woman’s body to work the way it should and to stay stable. In cases of an imbalance in these hormones, severe and long-lasting symptoms may occur.
There are a number of female hormone imbalance symptoms that must be considered. Some of the common ones are:
A drop in progesterone levels may be the culprit leading to sleep problems. These may include difficulty going to sleep, not getting restful sleep, or waking up early and not being able to resume sleep. Of course, not getting sufficient sleep can bring on other problems.
Even though many women experience acne breakouts during menses, these typically clear up in a few days. With imbalanced hormones, the acne may become deep, cystic acne which is hard to clear up. This kind of acne may appear on the face, neck, or the trunk and may be due to an overabundance of testosterone. The higher the level of testosterone, the more severe the breakout.
 An estrogen deficiency may be the cause of poor memory and concentration during menses, perimenopause, and menopause. The stress fighting hormone, cortisol, can also be a part of this problem. If you find yourself forgetful when under stress, cortisol may be the reason.
An estrogen deficiency may be the cause of poor memory and concentration during menses, perimenopause, and menopause. The stress fighting hormone, cortisol, can also be a part of this problem. If you find yourself forgetful when under stress, cortisol may be the reason.
One of the common female hormone imbalance symptoms and in AFS is craving for certain foods. Craving sweets is often an indication of lack of sleep due to imbalanced hormones. This can occur in both males and females. Craving salty foods points more to adrenal gland fatigue and may be an indication of minerals being lost through urination.
During menstruation, flare-ups of symptoms of irritable bowel syndrome are common. This may be due to the variations of estrogen and progesterone during that time. It is possible that problems with the thyroid hormone may play a part as well.
In both AFS and imbalanced hormones, fatigue is a factor. Not sleeping well results in feeling unrested in the mornings and throughout the day. Poor sleep patterns are seen frequently with both of these conditions. Hot flashes and night sweats may be brought on by a deficiency in estrogen, while insomnia may be an indication of out of balance progesterone levels.
All of these are seen within female hormone imbalance symptoms as well as AFS. Often, they are the result of low testosterone levels.
High levels of estrogen can bring on significant weight increase, especially in the abdominal area. When progesterone levels are out of balance, an unexplained weight gain that is hard to lose may occur. If you have AFS and your adrenals are fatigued, your thyroid may slow down metabolism. When this happens, your pancreas may respond by storing fat around your midsection.
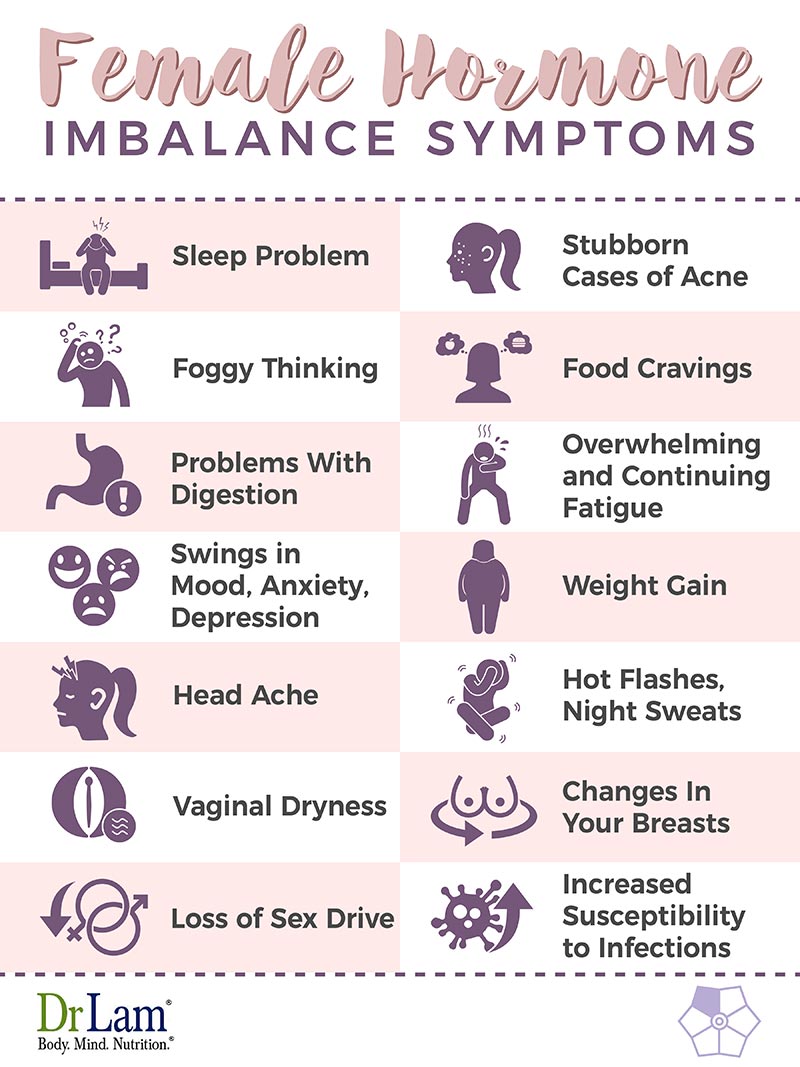
Progesterone that is out of balance may be the culprit behind your headaches, especially during menstruation.
Every woman who is going or has gone through menopause knows what it’s like to wake up in the middle of the night drenched in sweat or to suddenly be overcome by a feeling of absolutely burning up for no apparent reason. These female hormone imbalance symptoms have been thought to be due to a lack of estrogen. Some practitioners now think they’re caused by a surplus of estrogen and lack of progesterone or possibly an imbalance of other hormones from other organs in your body. Whatever the cause, women know (and men do, too) they are very uncomfortable.
Lack of estrogen is the most likely cause of this symptom. Of course, this makes intercourse painful and can lead to difficulties in your relationships.
 During menopause especially, women can experience a higher than normal level of estrogen. This can lead to breast pain, lumps in the breasts, fibroid tumors, and cysts. With progesterone levels out of balance, painful breasts also can occur. The lumps often cause concern for women, so periodic mammograms are recommended during this time.
During menopause especially, women can experience a higher than normal level of estrogen. This can lead to breast pain, lumps in the breasts, fibroid tumors, and cysts. With progesterone levels out of balance, painful breasts also can occur. The lumps often cause concern for women, so periodic mammograms are recommended during this time.
Low estrogen levels can lead to lack of interest in sex. The vaginal dryness and painful breasts frequently seen during times when hormones are out of balance also add to this lack. No one wants to engage in intercourse when it’s painful or when foreplay brings discomfort.
Estrogen levels that are either too high or too low can lead to more infections. Too much estrogen can lead to chronic yeast infections and too little estrogen can lead to more urinary tract infections.
Many of the female hormone imbalance symptoms seem to be found mostly in menopausal women, but it’s not the only time this imbalance can hit you.
Age is often a causative factor in these symptoms, but medications like birth control pills can also have an effect on your body chemistry. Of course, pregnancy pushes your hormones in directions you don’t often expect. Other things can lead to hormonal imbalance as well. Some women are genetically likely to have this kind of situation. Irregular sleep patterns, not enough exercise, and diet can all cause your hormonal imbalance. Researchers and clinicians are also seeing stress as a contributing factor to female hormone imbalance symptoms.
 To start your recovery from female hormone imbalance symptoms you need to start with hormone rebalancing. Hormone rebalancing needs to start with good nutrition, because food is the primary building block of estrogen and progesterone. Of critical importance is optimization of the microbiome in the gut and the need for adequate and effective foods to nourish our GI tract.
To start your recovery from female hormone imbalance symptoms you need to start with hormone rebalancing. Hormone rebalancing needs to start with good nutrition, because food is the primary building block of estrogen and progesterone. Of critical importance is optimization of the microbiome in the gut and the need for adequate and effective foods to nourish our GI tract.
It is important to understand that any remedy, especially when attempting to relieve or correct female hormone imbalance symptoms, must be considered from the whole body or NEM model. Keeping in mind how the various systems in our bodies interact will allow a successful solution.
The fact is that all our inner systems are connected and that they all communicate with hormones are important. When hormones are out of balance, the symptoms they create are your body’s way of telling you it’s not getting the support needed for optimum functioning.
That’s why expert guidance is a must when it comes to hormone balance. All the recommendations we’ve given thus far should be adapted to your specific condition and needs. This ensures you avoid the common pitfalls and risks that can come with recovery as much as possible. You can ask more about this process in an initial consultation we provide for free by calling on +1 (626) 571-1234.
Most often these female hormone imbalance symptoms are treated with prescription medications. This is in spite of evidence of significant side effects of these medications. For instance, giving estrogen orally may increase inflammation and bring on all the unwanted effects of this increase.
A longitudinal study, called the Women’s Health Initiative, of a total of approximately 27,000 women over a period of about eight years found significant detrimental effects from the use of synthetic hormones. One finding of increased risk of breast cancer led to the stopping of one part of the study, the part where women were treated with estrogen and progestin compounds. The estrogen only study appeared to increase the risk of stroke also. The risk of dementia and mild cognitive impairment were seen to be increased in both parts of the study.
As might be expected, physicians stopped prescribing these medications for their female patients and about 65 percent of women already taking the medicines stopped. It does appear that there were some flaws in this study that may have skewed the findings in a negative direction.
There are some new studies that seem to indicate usefulness of synthetic hormones for women who are early in menopause. Unfortunately, there is no indication that this benefit would continue if women continue taking these hormones as they age.
Some of the possible benefits for younger women of synthetic hormones are prevention of heart disease, hip fractures, and osteoporosis, along with a 30 percent decrease in the risk of developing diabetes.
Thus, the age at which women begin taking synthetic hormones may make a difference in the beneficial effects they experience. Healthy women in their 50s may have a slight risk of blood clots, but researchers feel this risk is not likely to cause problems. On the other hand, women first taking synthetic hormones in their 60s may have more risk.
This factor of age and assumed health is one of the possible flaws in the Women’s Health Initiative study. The study investigated women whose average age was 63. Possibly, the researchers were studying women who were already ill. The researchers involved in the study reported their intent to be looking at whether hormone therapy would protect older women against becoming ill. Clearly, it did not.
 In spite of what appear to be disturbing long-term side effects of synthetic hormone replacement therapy, the FDA still says this should be the treatment of choice for women with severe female hormone imbalance symptoms; the research is still divided regarding long-term use. For certain, continued and regular physical exams should remain part of every woman’s schedule when they’re on hormone replacement therapy with synthetics.
In spite of what appear to be disturbing long-term side effects of synthetic hormone replacement therapy, the FDA still says this should be the treatment of choice for women with severe female hormone imbalance symptoms; the research is still divided regarding long-term use. For certain, continued and regular physical exams should remain part of every woman’s schedule when they’re on hormone replacement therapy with synthetics.
So, if synthetic hormone replacement is so dangerous, what are the other options? One is bioidentical hormone replacement (bHRT)
These substances are biochemically the same as human hormones and are made from natural materials. Typically, they are compounded individually by a pharmacist to give a unique dose to each patient. Delivery methods are also individualized, making these hormones more tolerable for many patients.
Bioidentical hormones have been researched and used for several years by millions of women. Results of use of these hormones has nearly uniformly been positive.
Has been shown to be very effective in the relief of vaginal dryness, painful intercourse, and UTIs. These are common symptoms of estrogen deficiency. The estriol in the bi-estrogen deals with these female hormone imbalance symptoms. Estradiol, the second ingredient in bi-estrogen, also brings relief from vaginal dryness. Also, it relieves night sweats and hot flashes, increases mood and sleep, brings more energy, improves memory and thinking, and reduces the risk of developing type 2 diabetes.
Adds estrone to the combination of estriol and estradiol seen in bi-estrogen. This bioidentical hormone is typically used with women who are either underweight or of low normal weight.
Often given to women who have a surplus of estrogen compared to progesterone. This is also known as estrogen dominance. Natural progesterone appears to increase bone density, thus possibly lowering the risk of osteoporosis. Sleep is improved, libido increased, blood pressure lowered, and it helps to regulate blood glucose.
Used with women to help increase libido, increase bone mass, lower cholesterol and triglycerides, increase alertness, and give a sense of well-being.
Can improve libido, increase bone mass, improve mood and sense of well-being, lower cholesterol and triglycerides, and help regulate blood glucose levels.
Even with the many benefits outlined above, bioidentical hormones also have some side effects that may not be pleasant. Any side effects with these hormones typically will be related to dosage, so adjustments in dosage may be necessary after a period of time if these side effects occur.
With testosterone treatment, both men and women have experienced increased aggression, irritability, and outbreaks of acne. These side effects typically happen in the early stages of therapy and usually resolve once the level of testosterone is balanced.
Estrogen therapy may lead to some side effects in some women. These side effects include tenderness in the breasts, spotting, cramping, and bloating. Once again, these typically occur in the early stages of therapy and usually resolve once balanced levels of the hormone are achieved.
With some of the bioidentical hormones, some patients complain of itching or redness at the site of injection or insertion. Once their bodies adjust, these female hormone imbalance symptoms typically disappear.
 Some people choose not to use either synthetic or bioidentical hormones because of significant or potential side effects. Herbal remedies are sometimes used.
Some people choose not to use either synthetic or bioidentical hormones because of significant or potential side effects. Herbal remedies are sometimes used.
These herbal remedies are the most commonly chosen alternative ways of balancing hormone levels. They may be the easiest route to follow, and they appear to be the only good way to get directly to the source of the hormonal imbalance and rectify it.
Basically, there are two types of herbs used for this purpose: phytoestrogenic and non-estrogenic herbs. The phytoestrogenic herbs have estrogenic ingredients made by plants. Thus, they work to change the hormone imbalance by bringing the plant-based estrogens into the body. One potential difficulty with this approach is that by adding outside sources of estrogen, women’s bodies may produce less estrogen on their own. If this happens, it adds to the decrease of the body’s own estrogen.
Black cohosh is one of the phytoestrogenic herbs. It appears to decrease spasms and inflammation. As we have seen, inflammation is implicated in both female hormone imbalance symptoms and AFS. This herb helps relax the uterine muscles, easing menstruation and the cramping that often comes with it. It also can help regulate menstrual periods. Herbs, however, are foreign to the body. The risk of developing toxic reactive metabolite overload tends to be much higher than that of normal naturally occurring compounds like magnesium.
Non-estrogenic herbs stimulate the woman’s production of hormones by providing nourishment to the pituitary and endocrine glands, helping them to produce natural hormones better. This herb not only brings about a balance of estrogen, it also helps balance progesterone and testosterone. Using these herbs may be the safest way to improve the balance of female hormones naturally. They don’t add any outside hormones to the body, relying on stimulation and nourishment of the body’s own production of hormones.
Other herbs that may help in balancing female hormones are not as easy to classify as those above. One of these is chasteberry. It supports women’s menstrual cycle and has some benefits for PMS symptoms and menopause. It does contain progesterone. Chasteberry appears to help regulate how much prolactin is secreted by the pituitary gland, thus decreasing breast tenderness and soreness.
Ashwagandha root is another herb used to counter some of the female hormone imbalance symptoms. An adaptogen, ashwagandha root nourishes bones and muscles, decreasing joint movement discomfort. It also calms the mind and helps people go to sleep. An improvement in cognitive function has been seen with use of this herb. Unfortunately, this compound can worsen those with adrenal fatigue.
Lifestyle changes are another approach to be considered in striving to change imbalanced hormone levels. We are what we eat is a common saying that holds a great deal of truth. Food intake in the U.S. is often made up of foods that are fast, but not good or good for us. Making changes in what we put in our bodies can make a change in our bodies.
Making changes in lifestyle is the type of recommendation for imbalanced hormones that holds the least risk, but requires the most self-discipline. Food choices are not the only element involved in this kind of change. Reducing stress in our lives is important, as is regular physical exercise.
 Increasing foods high in omega-3 and omega-6 fatty acids will begin changing the imbalance in hormone levels. Foods like flax seeds, pumpkin seeds, and sunflower seeds will increase omega-3 levels. Eggs, nuts, and poultry contain omega-6 nutrients.
Increasing foods high in omega-3 and omega-6 fatty acids will begin changing the imbalance in hormone levels. Foods like flax seeds, pumpkin seeds, and sunflower seeds will increase omega-3 levels. Eggs, nuts, and poultry contain omega-6 nutrients.
Reducing salt intake is another factor in reducing bloating and easing both physical and emotional symptoms. This may be counterproductive for those with AFS. Limiting sugar and caffeine intake can decrease PMS symptoms. Avoiding or at least decreasing foods with aspartame and MSG (both excitotoxins) will improve brain functioning and decrease PMS symptoms.
Vitamin B6, zinc, and magnesium are all necessary for improving hormone imbalance. Eating whole grains, nuts, legumes, seafood, poultry, and vegetables will add these nutrients to your body.
Female hormone balancing is a complex subject. Reaching a positive outcome requires a personalized approach. Traditional synthetic hormones have their place, and natural bioidentical hormones have their defects. The capable practitioner also must factor in the gut microbiome and inflammatory ramifications of hormone replacement. Sufferers with adrenal fatigue face more difficulty. Each compound has its pros and cons. Navigating through this maze successfully requires much clinical experience.
We have helped thousands of women regain their hormone balance and, in turn, get their energy, vitality, and health back. Our focus is on you as a whole person, taking into account your physical, emotional, and social wellbeing. We also create health and nutrition plans that fit your specific needs and lifestyle. If that approach feels right for you, give us a call to set up a free initial consultation with one of our coaches.