 Excessive tiredness and lethargy are common complaints among adult patients. Symptoms such as excessive tiredness, fearfulness, allergies, frequent influenza, arthritis, anxiety, depression, reduced memory, difficulties in concentrating, insomnia, feeling worn-out, and the inability to lose weight after extensive efforts all point to Adrenal Fatigue. A weak adrenal system has profound systemic decompensatory actions, manifesting in a wide range of symptoms, including excessive tiredness. No organ is spared. The affected organs and their resulting conditions can be broadly classified into five major categories: metabolic system imbalance, musculoskeletal system breakdown, neurological system dysfunction, hormonal system imbalance/overload, and immune system dysfunction.
Excessive tiredness and lethargy are common complaints among adult patients. Symptoms such as excessive tiredness, fearfulness, allergies, frequent influenza, arthritis, anxiety, depression, reduced memory, difficulties in concentrating, insomnia, feeling worn-out, and the inability to lose weight after extensive efforts all point to Adrenal Fatigue. A weak adrenal system has profound systemic decompensatory actions, manifesting in a wide range of symptoms, including excessive tiredness. No organ is spared. The affected organs and their resulting conditions can be broadly classified into five major categories: metabolic system imbalance, musculoskeletal system breakdown, neurological system dysfunction, hormonal system imbalance/overload, and immune system dysfunction.
Hypoglycemia (low blood sugar) is common with Adrenal Fatigue. This is normally due to the combination of low cortisol and high insulin levels when the body is under stress. The normal stress response by the adrenals is to increase the blood glucose level. Glucose release is slowed as the output of cortisol reduces in adrenal exhaustion. This slowing, along with a high insulin level, leads to an increased demand for glucose. Ultimately, this leads to hypoglycemia with common symptoms of dizziness and fainting. As cellular energy demand is not being met by blood glucose, the body will turn to protein and fat as sources of energy. This pathway is not quite as efficient so the body is put in overdrive in order to provide the required energy. This increased demand is difficult or impossible to meet without adequate cortisol levels to elevate blood sugar levels by facilitating the conversion of glycogen, fats, and proteins to new glucose supplies. Clinically, one of the hallmarks of Adrenal Fatigue is irregular blood sugar patterns with hypoglycemia. In the presence of increased insulin and decreased cortisol, the blood sugar level drops rapidly, and frequent small meals are needed to replenish the body's energy needs.
Hypoglycemia itself is a significant stress on the entire body, and especially on the adrenals. While this can be overcome with a sugar fix consisting of an instant load of sugary drinks such as juice or soda, this is only a quick-fix remedy. Usually, the symptoms like excessive tiredness will disappear immediately, but then return after 1-2 hours. Reactivation and restoration of normal cell functions require extra amounts of energy beyond what is normally required for the maintenance of normal energy burn. With each hypoglycemic episode, more cells are damaged. Thus, the body reaches a new low with each incidence of hypoglycemia. If this happens at the same time as the demand for glucose increases, the stage is set for an adrenal crisis. With each plunge, the Adrenal Fatigue and excessive tiredness increases and hypoglycemia worsens. By the end of the day, the person may feel exhausted with excessive tiredness despite not having done anything. Low blood sugar levels are most likely to occur at around 10:00 AM, 2:00 PM, and from 3-4:00 PM.
Hypoglycemia is also related to autonomic nervous system dysfunction which is described in greater detail below.

Collagen and protein are broken down in a catabolic state of function during Adrenal Fatigue. This can lead to chronic pain syndromes, joint pain, chronic fatigue and excessive tiredness, and fibromyalgia.
Glucocorticoids, primarily cortisol, are steroidal hormones produced by the adrenal glands in response to stress. Cortisol output is usually high in stage 1 and 2 of Adrenal Fatigue. As Adrenal Fatigue progresses, cortisol output is often pushed to its limit. A chronically high cortisol output leads to a state of catabolism ( the breakdown of proteins in order to generate energy).
The cycle of catabolism is normally followed by a process of rebuilding or anabolism. In Adrenal Fatigue, the rebuilding process, normally carried out by androgens, is overwhelmed by the amount of catabolic hormones. Therefore the rebuilding process will be slow and sluggish. Broken down muscles are not adequately replaced. Collagen is broken down without significant replenishment. Outwardly, wrinkles start to develop as premature aging sets in. Internally, organ and muscle breakdown lead to chronic muscle and joint pains of unknown origin, especially after strenuous exercise or heavy lifting.
As the collagen structures of internal organs breakdown, their functions are compromised. Gastrointestinal track motility and contraction forces are reduced. Adrenal Fatigue is often associated with the poor ability to digest proteins and common symptoms include indigestion and irritable bowel syndrome. The amount of acid production in the body may not be sufficient to help break down the digested foods, resulting in further improper digestion.
It is therefore no surprise that secondary fibromyalgia and chronic fatigue syndrome are commonly associated with adrenal exhaustion. Many have postulated that Adrenal Fatigue often precedes fibromyalgia and chronic fatigue. These may indeed be part of the many symptoms of adrenal dysfunction.
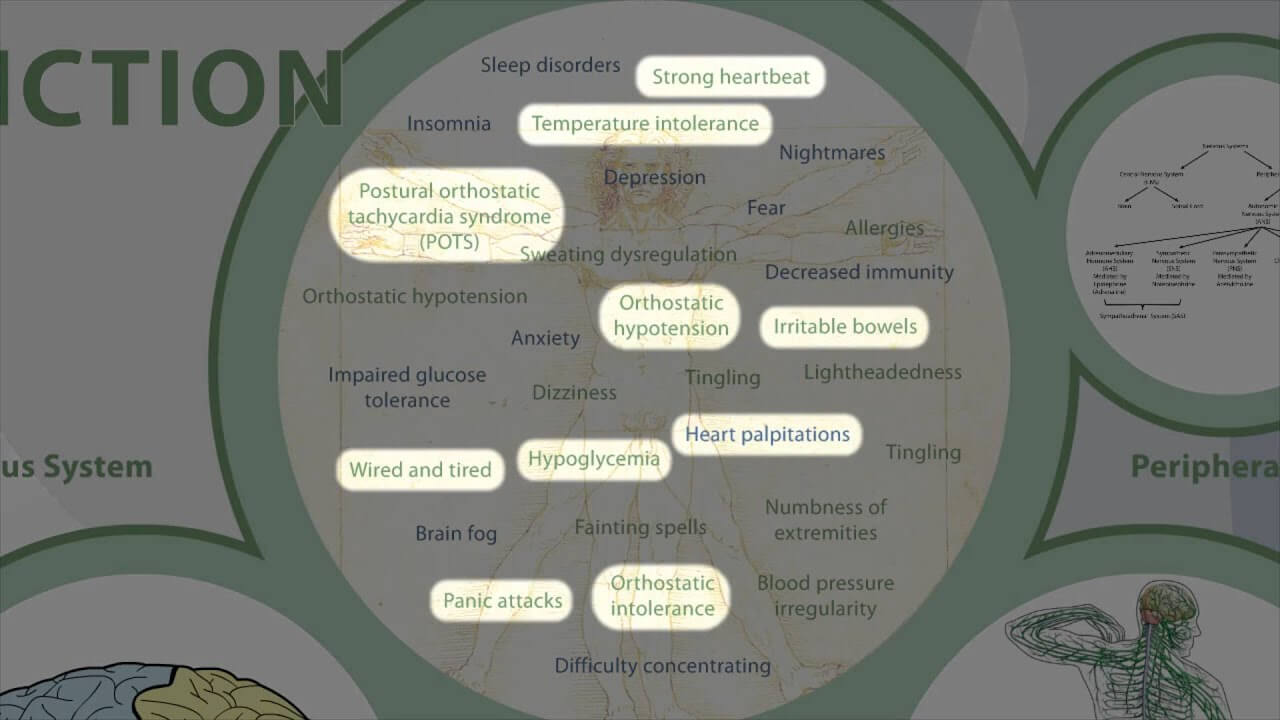
Adrenal Fatigue can lead to insomnia, sleep disorders, brain fog, anxiety and depression if the central nervous system is involved. Peripheral nervous system dysfunction is often associated with orthostatic hypotension, dizziness, lightheadedness, temperature intolerance, fainting spells, tingling and a numbness sensation of extremities, and sweating dysregulation.
If one suffers from adrenal exhaustion, one's brain requires increased energy and is especially affected by a lack of glucose as well as toxic metabolite build up in the body. As far as the body is concerned, ensuring a well functioning brain is a top priority. Most mechanisms involved in regulating the body's blood sugar are designed to ensure that the brain always has adequate glucose with which to function with. Insufficient glucose available to brain tissues contributes to the many central nervous system expressions of Adrenal Fatigue including sleep disorders, brain fog, anxiety and depression.
Sleep Disorders: Both too high and too low night time cortisol levels can cause sleep disturbances. The liver is often lacking the necessary glycogen reserve required by the adrenals to keep blood glucose stable during the night. When this happens, blood glucose levels may sometimes fall below the threshold and hypoglycemic (low blood sugar) symptoms occur. This can lead to sleep disruption during the night.  Waking up between 1:00 and 3:00 AM is a characteristic of low blood sugar during this time. Sometimes it is accompanied by nightmares, sudden onset of heart palpitations, anxiety attacks, and cold sweats. Lack of sleep can be a significant burden in itself. The body's ability to self repair is compromised when one is sleep deprived. This further contributes to Adrenal Fatigue and sets off a vicious downward spiral of cascading dysfunction.
Waking up between 1:00 and 3:00 AM is a characteristic of low blood sugar during this time. Sometimes it is accompanied by nightmares, sudden onset of heart palpitations, anxiety attacks, and cold sweats. Lack of sleep can be a significant burden in itself. The body's ability to self repair is compromised when one is sleep deprived. This further contributes to Adrenal Fatigue and sets off a vicious downward spiral of cascading dysfunction.
Every time the wake/sleep cycle is altered, it takes some time for the body and cortisol levels to normalize. Chronic lack of sleep is strongly associated with decreased immunity, impaired glucose tolerance, and decreased alertness and concentration.
Cortisol, DHEA, testosterone and estrogen are key hormones produced in the adrenals. Decreased levels of each of these hormones and reduced adrenal function have been linked to depression. It comes as no surprise that adrenal exhaustion is strongly associated with increased fears, anxiety, depression, and difficulties concentrating.
Brain fog is a mental state where your memory becomes clouded and unclear. It is not a state of loss of memory, immediate or long-past. It is a state where your memory appears to be "so close and yet so far" in terms of your ability to recollect. Sometimes you cannot remember where you put your keys, or what you did yesterday. You are confused. It is often associated with Adrenal Fatigue, hormonal imbalance, PMS, estrogen dominance, heavy metal poisoning, and hypothyroidism. Brain fog is usually transient in its duration, lasting anywhere from hours to days, and in advanced cases can become chronic.
Brain fog and excessive tiredness can present itself in many ways such as the loss of mental acuity, forgetfulness, the inability to think clearly, short term disorientation which can last a few minutes, a decreased attention span, confusion, spaciness, difficulty in acquiring new skills, a reduction in creativity, short term memory problems, and a reduced ability to concentrate.
The exact pathophysiology is unclear. It has been postulated that excessive metabolite build up in the brain over time due to poor clearance is a major factor. Brain fog usually goes away as the body's detoxification system kicks in. But if the system is not performing optimally, brain fog may remain for a long time. Some people try to do various types of detoxification, thinking that this will help. Sometimes it does, but most of the time, inexperienced detoxification methods can worsen brain fog and excessive tiredness. They may even trigger a re-toxification reaction, with symptoms such as fever, muscle and joint pain and general malaise.
The peripheral nervous system of the body is divided into two parts. The somatic nervous system regulates skeletal muscle functions that help us deal with the outside world, and the autonomic nervous system (ANS) regulates the functions of the smooth muscles and glands within the body for proper inner world workings.  The ANS is further divided into the parasympathetic nervous system (PNS), the sympathetic nervous system (SNS), and the adrenomedullary hormonal system (AHS). The PNS regulates the vegetative processes such as urination and digestive function. Dysfunction of the PNS leads to a wide variety of illness including abnormal gastric acid secretion, reduced gut motion, erectile dysfunction, loss of urinary control, and bowl movement irregularities. The SNS regulates the unconscious "housekeeping" functions of the body, including blood pressure, body temperature, force of the heartbeat, and heart rate. SNS dysregulation is common in Adrenal Fatigue. The AHS (also called the sympathetic adrenergic system) regulates the emergency and distress functions such as those responsible for the body's "fight or flight" response. When this response is activated fainting, shock, extreme fear, hypoglycemia, and low body temperature can occur. The combination of the AHS and the SNS constitutes the sympathoadrenal system (SAS).
The ANS is further divided into the parasympathetic nervous system (PNS), the sympathetic nervous system (SNS), and the adrenomedullary hormonal system (AHS). The PNS regulates the vegetative processes such as urination and digestive function. Dysfunction of the PNS leads to a wide variety of illness including abnormal gastric acid secretion, reduced gut motion, erectile dysfunction, loss of urinary control, and bowl movement irregularities. The SNS regulates the unconscious "housekeeping" functions of the body, including blood pressure, body temperature, force of the heartbeat, and heart rate. SNS dysregulation is common in Adrenal Fatigue. The AHS (also called the sympathetic adrenergic system) regulates the emergency and distress functions such as those responsible for the body's "fight or flight" response. When this response is activated fainting, shock, extreme fear, hypoglycemia, and low body temperature can occur. The combination of the AHS and the SNS constitutes the sympathoadrenal system (SAS).
The other parts of the ANS include the enteric nervous system (ENS) which regulates enteric functions and the sympathetic cholinergic system (SCS) which regulates sweating.
Maintaining a normal balance within the ANS, especially the SAS, is vital to optimal bodily function and homeostasis and the avoidance of excessive tiredness. Overstimulation of the SAS is commonly seen in advanced stage Adrenal Fatigue. It is usually a secondary compensatory response triggered by stress. The resulting influx of symptoms, like excessive tiredness, is known as the reactive sympathoadrenal response (RSR) (also called reactive sympathoadrenal overtone (RSO)). The body is flooded in a sea of adrenaline and norepinephrine. Symptoms include a faster than normal resting heart rate, anxiety and panic attacks, heart palpitations that come at will, strong heart beat, irritable bowel, being "wired and tired", POTS, orthostatic intolerance, orthostatic hypotension, hypoglycemia, excessive tiredness, and temperature intolerance, just to mention a few. There would also be periodic burst adrenaline where all these symptoms can be amplified into a sense of impending doom. We shall examine the mechanism of this condition further below.
Neurotransmitters are endogenous chemicals, which relay, amplify and modulate signals between a neuron and another cell. They are present in the synaptic junction of each nerve. Major neurotransmitters include glutamate, GABA, glycine, serine, dopamine, norepinephrine, epinephrine, histamine, serotonin, melatonin, acetylcholine, and nitric oxide. Some neurotransmitters are commonly described as "excitatory" or "inhibitory". By far the most prevalent transmitter is glutamate, which is excitatory at well over 90% of the synapses in the human brain. It is also used at most synapses that are "modifiable", i.e. capable of increasing or decreasing in strength. The next most prevalent is GABA, which is inhibitory at more than 90% of the synapses that do not use glutamate. Many sedative/tranquilizing drugs act by enhancing the effects of GABA. There are other neurotransmitters, such as acetylcholine, for which both excitatory and inhibitory receptors exist.  GABA also operates in many regions of the brain, but uses different types of receptors. Serotonin is produced by and found in the intestine. It functions to regulate appetite, sleep, memory, learning, temperature, mood, behavior, muscle contraction, and function of the endocrine and cardiovascular system. If there is a dysregulation it could cause symptoms like excessive tiredness. It is also speculated to have a role in depression, as some depressed patients are seen to have lower concentrations of metabolites of serotonin in their cerebrospinal fluid and brain tissue.
GABA also operates in many regions of the brain, but uses different types of receptors. Serotonin is produced by and found in the intestine. It functions to regulate appetite, sleep, memory, learning, temperature, mood, behavior, muscle contraction, and function of the endocrine and cardiovascular system. If there is a dysregulation it could cause symptoms like excessive tiredness. It is also speculated to have a role in depression, as some depressed patients are seen to have lower concentrations of metabolites of serotonin in their cerebrospinal fluid and brain tissue.
In Adrenal Fatigue, many normal neurotransmitter functions are altered. In early stages of Adrenal Fatigue (Stage 1 and 2), serotonin levels tend to be weakened, epinephrine and norepinephrine are elevated, and GABA tends to increase to compensate.
As Adrenal Fatigue progresses, cortisol output will start to fall. Thyroid binding globulin tends to rise which leads to reduced T4 and T3 with a corresponding rise in TSH. DHEA increases and the body is put on overdrive to produce more cortisol. Serotonin falls as dopamine and norepinephrine continues to rise as the sympathetic nervous system is activated.
In advance Adrenal Fatigue (Stage 3 or higher), DHEA starts to fall along with cortisol and serotonin. Epinephrine, dopamine, norepinephrine, and GABA may remain high or erratic in their levels. The autonomic nervous system is dysregulated, leading to adrenaline rushes and reactive sympatho-adrenal responses classically responsible for the "wired and tired" sensation.
Key hormones associated with adrenal exhaustion and excessive tiredness include epinephrine (adrenaline), norepinephrine, estrogen, testosterone, melatonin, progesterone and thyroid. Their imbalances can lead to estrogen dominance, hypothyroidism, adrenaline rushes, fragile blood pressure, hirsutism, hair loss and acne.
Norepinephrine is a neurotransmitter secreted under the control of the SNS. Adrenaline is a hormone secreted from the adrenal medulla under the control of the adrenomedullary hormone system (AHS) and deals with emergency functions of the body. While adrenaline is released during normal daily activities, its release is increased during extreme distress. Chronic or acute stress leading to Adrenal Fatigue increases AHS activation. A rise in the absolute level of adrenaline in the body leads to an increased heart rate, increased blood sugar, increased respiration, reduced serum potassium, relaxation of skeletal muscle blood vessels, an increase in energy, an increase in emotional sweating, constriction of skin blood vessels (pallor), relaxation of the gut and trembling. This adrenaline overload, along with norepinephrine, worsen the existing ANS imbalance already common in people with Adrenal Fatigue, and it triggers an additional host of dysfunctions above and beyond those already experienced.
In normal people, excess adrenaline released from the adrenal glands during stress is quickly sopped up by efficient adrenaline transporters which carry away these undesirable hormones before they can wreak havoc as they circulate in the body.  For example, standing requires blood vessels to contract to keep gravity from allowing all your blood from pooling in your legs. This is accomplished through the release of small amounts of adrenaline, the body's "fight or flight" hormone. The body releases just the right amount of this hormone throughout the day as we move around and change positions. Excess adrenaline is cleared out of the body. The body's blood pressure is thus maintained in a normal state. Unfortunately in people suffering from adrenal exhaustion, the excessive activation of the SAS leads to a massive amount of adrenaline and norepinephrine being released which can remain in circulation for longer than the usual duration before they are inactivated. Blood pressures of people who are in adrenal exhausted states and suffer from excessive tiredness are usually below normal levels, but they can abruptly increase and stay high if a large amount of adrenaline is released quickly into the bloodstream. Alternatively, the heart rate may be elevated for no apparent reason. Consistent high levels of norepinephrine and epinephrine also lower the threshold of normal cardiac rhythm, triggering abnormal cardiac arrhythmias such as atrial fibrillation, whether they are vagally mediated or sympathetically mediated. Adrenaline release as part of the body's emergency responses is usually self limiting in normal people. In people suffering from adrenal exhaustion and excessive tiredness, however, these symptoms not only persist but can become exaggerated. The mechanisms of these pathways physiologically are not fully known. Research studies are pointing to the loss of a negative feedback loop function, leading to a positive feedback loop response, as a possible etiology.
For example, standing requires blood vessels to contract to keep gravity from allowing all your blood from pooling in your legs. This is accomplished through the release of small amounts of adrenaline, the body's "fight or flight" hormone. The body releases just the right amount of this hormone throughout the day as we move around and change positions. Excess adrenaline is cleared out of the body. The body's blood pressure is thus maintained in a normal state. Unfortunately in people suffering from adrenal exhaustion, the excessive activation of the SAS leads to a massive amount of adrenaline and norepinephrine being released which can remain in circulation for longer than the usual duration before they are inactivated. Blood pressures of people who are in adrenal exhausted states and suffer from excessive tiredness are usually below normal levels, but they can abruptly increase and stay high if a large amount of adrenaline is released quickly into the bloodstream. Alternatively, the heart rate may be elevated for no apparent reason. Consistent high levels of norepinephrine and epinephrine also lower the threshold of normal cardiac rhythm, triggering abnormal cardiac arrhythmias such as atrial fibrillation, whether they are vagally mediated or sympathetically mediated. Adrenaline release as part of the body's emergency responses is usually self limiting in normal people. In people suffering from adrenal exhaustion and excessive tiredness, however, these symptoms not only persist but can become exaggerated. The mechanisms of these pathways physiologically are not fully known. Research studies are pointing to the loss of a negative feedback loop function, leading to a positive feedback loop response, as a possible etiology.
As mentioned earlier, adrenaline is a hormone that is stimulatory in nature. Symptoms of excessive adrenaline include heart palpitation, irritability, and anxiety. Less common are symptoms of dizziness, cold sweats, brain fog and orthostatic hypotension. In addition to possible adrenaline overload, those with weak adrenals may have a reduced capacity to clear the unwanted excess adrenaline and its metabolites from the body. This leads to excessive internal build up. In addition, a defective norepinephrine transporter system can worsen the condition and contributes to further excessive adrenaline level. This is because norepinephrine is the chemical father of epinephrine and its level is tied to epinephrine. As mentioned earlier, adrenaline and norepinephrine overload in the context of Adrenal Fatigue is usually a compensatory reaction of the ANS as the SAS is activated. This leads to a myriad of symptoms that are clinically confusing and hard to understand, such as unexplained orthostatic intolerance, fragile blood pressure, extreme lightheadedness, "spaciness", tachycardia, irregular heart rate, temperature intolerance, body fluid imbalance, sweating, fainting, loss of bowel and urination control, sense of impending doom, and dizziness. Sometimes these symptoms may be associated with and triggered by a diet high in carbohydrates or by a stressful event.  Other times, they can be triggered when at rest or from events that are not stressful at all, such as watching an action movie, taking a cold drink, being startled as the phone rings in a quiet room, etc. In layman's terms, the body's internal thermostat appears to be malfunctioning. The heating and cooling control systems are broken and the body activates the emergency mode (SAS) frequently. While the ultimate goal of ensuring survival has been met, the fine control is compromised. It's like getting into a bath or shower with either very cold or very hot water running but not the pleasant warm water that is suitable for bathing. The body therefore goes through wild metabolic and hormonal internal gyrations like a roller-coaster ride with fluctuations in blood sugar, body temperature, blood pressure, heart rate and emotional state. Laboratory studies are usually found to be normal as these symptoms remain sub-clinical.
Other times, they can be triggered when at rest or from events that are not stressful at all, such as watching an action movie, taking a cold drink, being startled as the phone rings in a quiet room, etc. In layman's terms, the body's internal thermostat appears to be malfunctioning. The heating and cooling control systems are broken and the body activates the emergency mode (SAS) frequently. While the ultimate goal of ensuring survival has been met, the fine control is compromised. It's like getting into a bath or shower with either very cold or very hot water running but not the pleasant warm water that is suitable for bathing. The body therefore goes through wild metabolic and hormonal internal gyrations like a roller-coaster ride with fluctuations in blood sugar, body temperature, blood pressure, heart rate and emotional state. Laboratory studies are usually found to be normal as these symptoms remain sub-clinical.
There may be a genetic component in this convoluted picture, but it is clear clinically that those with weak adrenals have a higher tendency to be more sensitive to excessive adrenaline / norepinephrine, and are more prone to suffer symptoms resembling sub-clinical dysautonomia. Unless a clinician is alert, this reactive state is often missed. Patients are often started on a failed approach of prescription drugs such as anti-depressants to control the symptoms rather than healing the adrenals.
Estrogen and progesterone imbalance leads to a continuum of Estrogen Dominance conditions including PMS, endometriosis, PCOS, cystic breast disease, breast cancer, and irregular menstrual periods, just to name a few. Here is how:
When the adrenals are stressed, the adrenal's response is to increase cortisol output. This requires more of the precursor, progesterone. Cortisol output rises in Stage 1 and 2 of Adrenal Fatigue. As adrenal weakness advances, cortisol output starts to decline due to being overworked. The precursor progesterone becomes deficient as the increased need for cortisol depletes the progesterone levels used in making cortisol. As more progesterone ( and also pregnenolone) is shunted or sequestered to make cortisol, less is available to balance off the estrogen. As a result, there is a relative increase in estrogen in the body compared to progesterone. This progesterone deficiency is commonly called Estrogen Dominance (ED). What is so bad about estrogen dominance? It is the root cause of a myriad of illnesses. Conditions associated with this include fibrocystic breast disease, PMS, uterine fibroids, breast cancer, endometriosis, infertility problems, endometrial polyps, PCOS, autoimmune disorders, low blood sugar problems, and menstrual pain, among many others
Adrenal Fatigue and Estrogen Dominance are very similar in their symptom presentation and share a lot in common. Most women who have one tend to have the other to some degree.  Because the symptoms are similar, Estrogen Dominance, when prominent, can mask underlying Adrenal Fatigue which then is overlooked. Clinicians can be misled into believing that the root problem is Estrogen Dominance when in fact it is Adrenal Fatigue in disguise. Administration of hormone replacement, natural or otherwise, may give temporary relief but normally fails over time if the adrenals are not healed. On the converse, if the recovery focus is placed on healing the adrenals first, symptoms of Estrogen Dominance often resolve on their own as adrenal health returns.
Because the symptoms are similar, Estrogen Dominance, when prominent, can mask underlying Adrenal Fatigue which then is overlooked. Clinicians can be misled into believing that the root problem is Estrogen Dominance when in fact it is Adrenal Fatigue in disguise. Administration of hormone replacement, natural or otherwise, may give temporary relief but normally fails over time if the adrenals are not healed. On the converse, if the recovery focus is placed on healing the adrenals first, symptoms of Estrogen Dominance often resolve on their own as adrenal health returns.
Another common reason for low progesterone levels is an anovulatory cycle (a menstrual cycle in which there is no ovulation). In Adrenal Fatigue, the body's emergency repair system is activated. Priority is given to metabolic balance to keep the basic bodily function such as blood pressure and blood sugar stable. Reproductive functions are considered a low priority at this point. Ovulation can be temporarily shutdown. In fact, many women in high stress environments do have irregular menstrual cycles and amenorrhea for this reason. Without the ovulation, there is no corpus luteum to make additional progesterone for the cycle. The lowered progesterone level leaves us with an excessive estrogenic effect due to deficiency of progesterone.
Estrogen Dominance can also be caused by excessive estrogenic stimulation. As Adrenal Fatigue progresses, weight gain is usually the norm as the body tries to slow down metabolism to conserve energy. Excessive fatty tissue is accumulated. Fat cells make estrogen and estrogen causes fatty tissue growth. Both lead to excessive estrogen and relative progesterone deficiency.
Estrogen also increases thyroid-binding proteins in the bloodstream. Thyroid blood test results may therefore be normal although there may be an insufficient free thyroid hormone level in the tissues, resulting in a state of sub-clinical or secondary clinical hypothyroidism.
When estrogen levels are high, the adrenal cortex also fails to respond to signals from the brain. A woman with estrogen dominance may have adequate levels well within the normal range of total cortisol in her bloodstream. However, her free available cortisol level may be low. Since only free cortisol can pass through cell membranes and activate receptors inside the cell, the effectiveness of cortisol is blunted at the cellular level.
Just as estrogen dominance can contribute to adrenal insufficiency, adrenal insufficiency can contribute to estrogen dominance. Cortisol is made in the adrenal cortex from progesterone. When the adrenals are weak, there is a tendency towards a lowered progesterone output in favor of cortisol. A low progesterone level is often the result leading to a state of relative estrogen dominance with its many undesirable consequences mentioned above. This forms a vicious cycle. Excessive estrogen affects both thyroid and adrenal functions. In turn, dysfunctional thyroid glands and Adrenal Fatigue make estrogen dominance worse.
 Thyroid hormone imbalances leading to clinical or sub-clinical hypothyroidism that is refractory to thyroid replacement therapy.
Thyroid hormone imbalances leading to clinical or sub-clinical hypothyroidism that is refractory to thyroid replacement therapy.
When the adrenals are weak, the ability of the adrenals to handle the stress associated with normal body functions and energy requirements is often compromised. To enhance survival, the adrenals force a down-regulation of energy production. In other words, the body is being forced to slow down in order to conserve energy. The body needs to rest in times of stress. Lower energy output reduces the workload of the body. This slowdown can result in hypothyroid symptoms despite sufficient circulating levels of T4 and T3.
Laboratory tests of T4 and T3 may look normal and TSH may increase. Classic symptoms of hypothyroidism are evident with persistent low body temperature. The physician reading the tests may be misled into prescribing thyroid replacement. In such cases, thyroid replacement without first considering adrenal fortification often fails. Thyroid replacement tends to increase metabolic functions. Raising the basal metabolic rate is akin to putting all systems of the body into overdrive at a time when the body is trying to rest with down-regulation.What the body wants (to slow down) and what the medications are designed to do (to speed up) are diametrically opposed to each other.
Thyroid medication administered under such circumstances may, in some cases, lead to a temporary relief of symptoms and a boost of energy at first. This is often short lived, and comes at a price. Those who are less fortunate with constitutionally weak adrenals may be intolerant to thyroid medications right from the start. Those that are able to accept thyroid replacement and remain stable may find themselves requiring it for life, often at increasing doses as time passes. The overall fatigue level continues to increase well beyond what the medications are trying to combat. Only by increasing medication dosage or switching to more powerful thyroid medication can the worsening excessive tiredness be avoided. The tendency is to switch from one medication to another. Starting with synthetic T4, to T4/T3 blends and ultimately, to potent the T3. The patient is subjected to an ongoing trial and error period as one drug after another fails. As this is going on, the body continues to decompensate as the medication usually prescribed becomes stronger and stronger. The patient's condition often continues to get worse despite the physician's best attempt to help. It comes as no surprise that as many as 70% of patients on thyroid replacement continues to complain of hypothyroid symptoms. Ultimately, excessive tiredness returns with a vengeance with time or stress, as thyroid medication further deteriorates pre-existing adrenal weakness and often precipitates an adrenal crisis.
Cortical Hormone Imbalance. The adrenal cortex comprises 80 percent of the adrenal gland and is responsible for producing over 50 different types of hormones in three major classes - mineralcorticoids, glucocorticoids, and androgens.
 Aldosterone, a mineralcorticoid, modulates the delicate balance of minerals in the cell, especially sodium and potassium. It therefore regulates our blood pressure. Stress increases the release of aldosterone, causing sodium retention (leading to water retention and high blood pressure) and loss of potassium and magnesium. Higher than normal blood pressure is a sign of early Adrenal Fatigue. Magnesium is involved in over 300 enzymatic reactions in the body. When the body lacks magnesium, it will suffer from a variety of pathological conditions such as cardiac arrhythmias, uterine fibroid, and blood pressure imbalance.
Aldosterone, a mineralcorticoid, modulates the delicate balance of minerals in the cell, especially sodium and potassium. It therefore regulates our blood pressure. Stress increases the release of aldosterone, causing sodium retention (leading to water retention and high blood pressure) and loss of potassium and magnesium. Higher than normal blood pressure is a sign of early Adrenal Fatigue. Magnesium is involved in over 300 enzymatic reactions in the body. When the body lacks magnesium, it will suffer from a variety of pathological conditions such as cardiac arrhythmias, uterine fibroid, and blood pressure imbalance.
The most important glucocorticoid is cortisol. In early Adrenal Fatigue, the cortisol level rises to help the body overcome stress. As Adrenal Fatigue advances, cortisol output generally drops and the body's ability to handle stress is reduced. Cortisol contracts mid-size arteries. People with low cortisol (as in advanced stages of Adrenal Fatigue) tend to have low blood pressure and reduced reactivity to other body agents that constrict blood vessels. Lower than normal blood pressure is a sign of advanced Adrenal Fatigue.
As Adrenal Fatigue worsens, the body's overall ability to maintain stable blood pressure is reduced, resulting ultimately in a condition known as labile blood pressure where the blood pressure varies and fluctuates widely.
Androgen imbalance. Both male and female hormones are secreted by the adrenal cortex, but their quantity is small and their effects are usually masked by the hormones from the testes and ovaries.
In adrenal exhaustion and excessive tiredness, the masculinization effect of androgen secretion may become evident after menopause or under stress - when estrogen levels from the ovaries decrease in absolute terms but increase in relative terms in a state of estrogen dominance. In women, the androgens ( testosterone and related hormones ) affect the secondary sex characteristics, leading to an increased conversion from testosterone to dihydrotestosterone or DHT and ultimately resulting in:
In men, a low libido is invariably an indicative sign of adrenal exhaustion and excessive tiredness. The body is in the process of preparing itself for survival. Production of hormones deemed less important by the body, such as reproductive hormones, is shunted to produce cortisol to ensure survival. Sex drive is reduced in both men and women, and period irregularity in women becomes common. Miscarriage prevalence is also increased. Long term androgen excess also increases the risk of infertility, cardiovascular disease, hypertension, osteoporosis, uterine cancer, and pituitary adenoma.
This can result in exaggerated autoimmune responses such as rheumatoid arthritis and Hashimoto's Thyroiditis, allergic rhinitis, skin sensitivities, psoriasis, hypoactive immune state of function, frequent infections, internal dysbiosis, candidiasis, recurrent herpes infection, HIV and Hepatitis C.
 Allergic reactions usually have strong adrenal components. Most allergies involve the release of histamine and other pro-inflammatory substances. The body's response is cortisol, a strong anti-inflammatory hormone. The level of circulating cortisol corresponds directly to the degree of inflammation in the body and the resulting symptoms of allergies. The weaker the adrenals, the stronger the effects of the allergies because the more histamine is released, the more cortisol it takes to control the inflammatory response and the harder the adrenals have to work to produce more cortisol. When the adrenals are exhausted, cortisol output is compromised, allowing unopposed histamine to inflame the tissues more. This vicious circle can lead to progressively deepening adrenal exhaustion and more severe allergic reactions. People with food and environmental allergies commonly have weak adrenal functionality. Common food allergens include wheat, corn, soy, milk, and eggs. One also can be gluten-free and still have wheat allergies.
Allergic reactions usually have strong adrenal components. Most allergies involve the release of histamine and other pro-inflammatory substances. The body's response is cortisol, a strong anti-inflammatory hormone. The level of circulating cortisol corresponds directly to the degree of inflammation in the body and the resulting symptoms of allergies. The weaker the adrenals, the stronger the effects of the allergies because the more histamine is released, the more cortisol it takes to control the inflammatory response and the harder the adrenals have to work to produce more cortisol. When the adrenals are exhausted, cortisol output is compromised, allowing unopposed histamine to inflame the tissues more. This vicious circle can lead to progressively deepening adrenal exhaustion and more severe allergic reactions. People with food and environmental allergies commonly have weak adrenal functionality. Common food allergens include wheat, corn, soy, milk, and eggs. One also can be gluten-free and still have wheat allergies.
Autoimmune disease such as Hashimoto's Disease or rheumatoid arthritis represent a spectrum of diseases in which the white blood cells of the immune system become overly active. Chemical messengers called cytokines form an integral part of the immune system. As messengers, cytokines inform and trigger other immune cells to activate, grow, or possibly die. Excessive chemical messengers known as cytokines are elevated in fibromyalgia and chronic fatigue, leading to excessive inflammation and flu-like symptoms. Chronic inflammation can reflect an improperly functioning immune system.The degree of hyperactivity of the immune response is also modulated by cortisol. If one has adrenal weakness, the cortisol output will drop below normal level, making one's body more susceptible to autoimmune and inflammatory reactions. Toxins released from viruses become un-opposed. The inflammatory reaction will only surge upwards as the overall condition worsens. In other words, the cortisol levels are inadequate in response to the reactions taking place in particular tissues or locations in the body.
Steroid medications such as prednisone or hydrocortisone are commonly prescribed to suppress autoimmune responses. These drugs mimic the anti-inflammatory effects of cortisol. While there may be a temporary sense of well-being and lack of excessive tiredness, this is usually short lived due to the many side effects associated with these medications. Long term use is to be avoided unless under close medical supervision.
A body under stress needs the anti-inflammatory effects of cortisol to restrain various physiological mechanisms and to prevent them from causing havoc inside the body, as in the case of toxins secreted by the over-reactive white blood cells in an auto-immune disease setting. Cortisol thus protects the body from autoimmune processes and uncontrolled inflammation. Lack of a sufficient level of cortisol commonly seen in people with advanced Adrenal Fatigue as the body's protective functions have been compromised leads to the unrestrained damage to the body by the overactive white blood cells.
One of the most frequently overlooked causes of Adrenal Fatigue are chronic infections. Respiratory illnesses and herpes are more common in people suffering from Adrenal Fatigue, and Adrenal Fatigue tends to predispose people towards developing respiratory problems.  Respiratory infections such as colds, bronchitis, sinus infections, mycoplasma infections, pneumonia, and the flu are especially hard on the adrenal glands and fatigue them rapidly. Recurrent respiratory infections are one of the most significant problems that can hamper full recovery in people suffering from Adrenal Fatigue.
Respiratory infections such as colds, bronchitis, sinus infections, mycoplasma infections, pneumonia, and the flu are especially hard on the adrenal glands and fatigue them rapidly. Recurrent respiratory infections are one of the most significant problems that can hamper full recovery in people suffering from Adrenal Fatigue.
Adrenal Fatigue can occur after just one single episode of serious infection. Such infections can be a respiratory infection or a gastric infection. Poorly performed dental procedures such as a root canal can also be a trigger. The more severe the infection, the more frequently it occurs or the longer it lasts, and the more excessive tiredness one has, the more likely it is that the adrenals are involved. It is not unusual for an infection to trigger an adrenal crisis and excessive tiredness. At the same time, chronic infections (such as prolonged flu, periodontitis, or candidiasis) of known or unknown origins may also act as triggers as well. Adrenal Fatigue can also take place over time as the adrenals are gradually fatigued by prolonged or recurrent infections. Stealth viruses and other infectious agents such as parasites and fungus are commonly overlooked culprits. The direct effects of a smoldering pathogen in the body, as well as the systematic stress the infection creates, will overload the adrenals chronically and weaken the body's immune system. This makes it harder to fight off the infection. Therefore, it is no surprise that adrenal exhaustion and excessive tiredness is commonly associated with frequent and repeated infections ranging from the common cold to sinus infections to gastrointestinal dysbiosis, with slower than normal healing times. The immune weakness that results from the weakened adrenals also sets the stage for pathogens responsible for fibromyalgia to be activated, resulting in greater debilitation. One must think of adrenal exhaustion and excessive tiredness as the cause if there is a longer than normal recovery period after an illness with decreased stamina and pronounced morning excessive tiredness.
Feeling better after exercise is generally a function of adrenaline being released into the body during exercise. Do be careful. As adrenaline wears off, energy slumps can occur. Many people experience a crash after exercise and don't know why.
If you don't have advanced stages of AFS, any exercise is good for the body provided they are not extreme. Walking, biking, hiking, yoga, and flexibility exercise in moderation are all safe for everyone as long as there aren't other medical issues. If you have advanced stages of AFS, make sure you follow professional guidance before embarking on exercise.
Some studies have shown that vaccination causes immune dysregulation. When anything is changed in your body the adrenals are affected because of the stress.
Cupping is a traditional Chinese Medicine method to increase circulation in the body so toxins can be removed from the skin. It can be considered for those who are in mild stages of AFS, but those with severe AFS should be careful as you can crash the body in the process.
Breastfeeding takes a lot of energy and nutrients from the mother’s body, plus it is a 24/7 job, at no set time your baby will need feedings. So a lack of sleep, postpartum, caring for the infant can all be very stressful during the first couple months for a new mother. Any stress does affect the adrenal glands.