 Unless you have celiac disease, you may not be aware of the many ways gluten sensitivity affects health. Gluten sensitivity is often associated with gastrointestinal symptoms that are the usual clues for food sensitivity, but these are not the only type of symptoms it can cause. If you’ve been experiencing neurological symptoms with no clear cause, gluten could be to blame. Research is showing more and more that, for those with gluten sensitivity, there is a bigger relationship between gluten and brain health than previously thought. Gluten seems to have a wide range of activity on the body, from inflammation to neurotoxicity. And because celiac and gluten sensitivity are becoming more and more common and often go unidentified, the effects of gluten on brain health are becoming more and more of an issue.
Unless you have celiac disease, you may not be aware of the many ways gluten sensitivity affects health. Gluten sensitivity is often associated with gastrointestinal symptoms that are the usual clues for food sensitivity, but these are not the only type of symptoms it can cause. If you’ve been experiencing neurological symptoms with no clear cause, gluten could be to blame. Research is showing more and more that, for those with gluten sensitivity, there is a bigger relationship between gluten and brain health than previously thought. Gluten seems to have a wide range of activity on the body, from inflammation to neurotoxicity. And because celiac and gluten sensitivity are becoming more and more common and often go unidentified, the effects of gluten on brain health are becoming more and more of an issue.
This appears to be because conventional gluten testing is not thorough enough. Also, though gluten intolerance and sensitivity are not new, the prevalence of these problems has increased dramatically in the last fifty years or so.
Researchers don’t know how many people have these problems because they are largely unidentified or mistaken for something else. The gastrointestinal symptoms that are the hallmark signs of gluten sensitivity or celiac disease can resemble other gastrointestinal conditions, while the neurological symptoms can resemble those of other neurological conditions.
This is especially the case in parts of the world that have not yet caught up with the growing evidence that gluten is a possible culprit in many conditions that otherwise have no clear cause, such as many autoimmune and inflammatory issues.
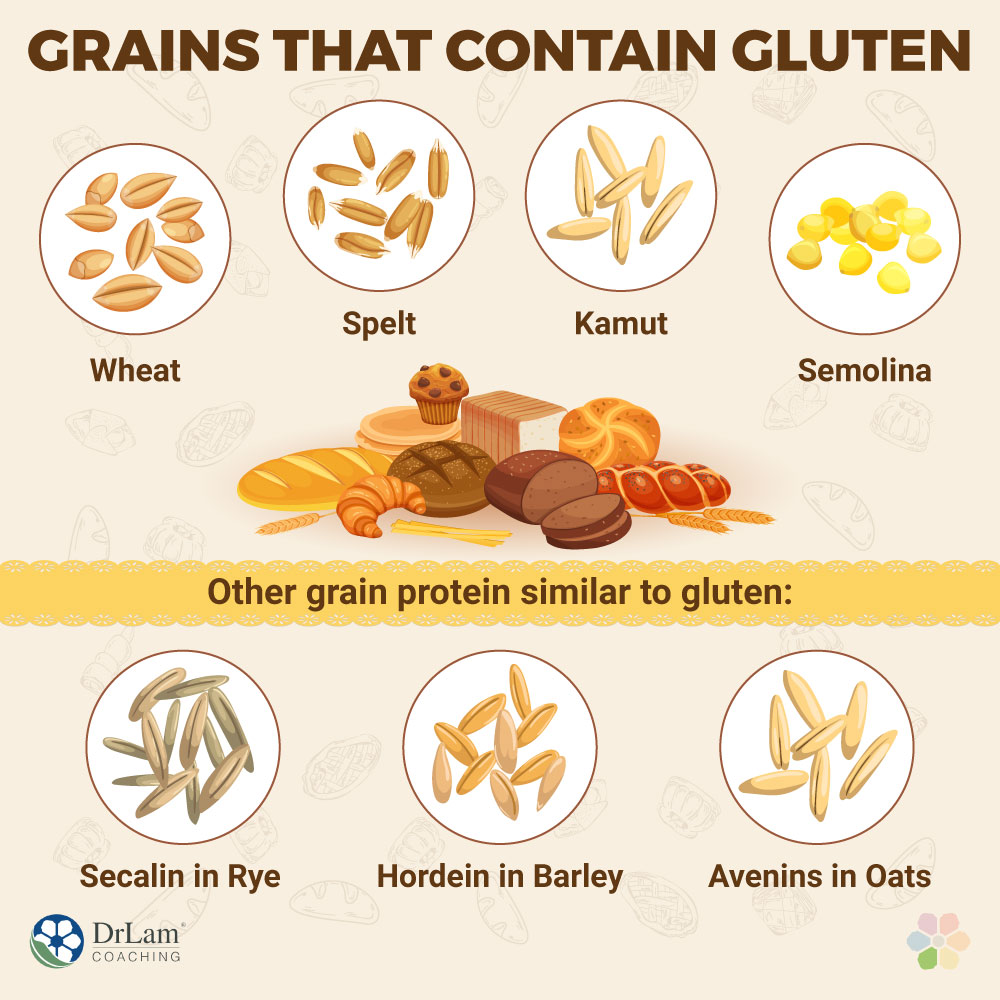
When you hear the word gluten, you probably immediately think “wheat.” And you’re right, that is the main product that contains gluten. Wheat products like pasta, bread, cakes, muffins, croissants, and other baked goods are everywhere. If you’re familiar with baking, you’ll know gluten is what makes the dough nice and fluffy and sticky.
However, gluten is also found in spelt, barley, Kamut, and semolina. Because gluten is heat stable and acts as a very good as a binder, it is also added to processed foods in order to enhance their moisture retention, flavor, and texture. Other products that can contain gluten are salad dressings, mayonnaise, supplements, and even medications and beauty products.
This means people who are advised to go on a gluten-free diet need to check labels of products.
With the average Western diet containing around 5-20 g of gluten a day, it’s no wonder there is a big hype about its effects on health. Now gluten and brain health is getting more attention than ever before, instead of the traditional focus on gastrointestinal issues.
As you read on, you might feel inclined to get tested or try an elimination diet to see if your health improves and if any neurological symptoms you have begin to clear. You are already taking the first important step to better health: getting informed.
So what exactly is gluten?
The gluten that is found in wheat is a mixture of many different kinds of proteins, with the main ones being glutenin and gliadin.
Glutenin is the protein that helps dough become strong and elastic. It is the protein that is found in highest concentration in gluten. Around 47% of gluten is composed of glutenin. Though previously thought to be the non-toxic party out of the two main proteins, recent studies are showing that it can also have some toxic effects for those suffering from celiac disease.
Gliadin seems to be the main problematic protein in gluten. Gliadin is very resistant to pancreatic, gastric, and intestinal proteolytic digestion. Proteolytic enzymes, also called proteases, specialize in breaking down proteins into amino acids. These proteolytic enzymes have an especially difficult time breaking down gliadin. This means that your digestive system’s enzymes are not well equipped to process the main protein found in gluten.
However, wheat gluten is not the only type that can cause or aggravate gluten-related disorders. There are a few others to watch out for:
 Rye breads are touted as healthier alternatives to white and wheat-based breads. They have a lower glycemic index and thus do not cause as much of a blood sugar spike. They also have a lower amount of gluten.
Rye breads are touted as healthier alternatives to white and wheat-based breads. They have a lower glycemic index and thus do not cause as much of a blood sugar spike. They also have a lower amount of gluten.
However, people with gluten sensitivity should still avoid rye because it contains the protein secalin. Secalin has a very similar amino acid sequence to wheat gluten and will result in an immune reaction.
Hordein is a protein found in barley, as well as other cereals. It is also found in beer, which makes drinking beer difficult for those with gluten sensitivity or celiac disease, although there are some types of low-gluten and gluten-free beers available on the market now.
Because hordein can sometimes be found in processed foods and products, it is important that you check labels for it as well as for wheat gluten.
Avenins also have a similar sequence of amino acids as wheat gluten, which means some people with gluten sensitivity or celiac disease may have an immune reaction to them. Also, oats are sometimes cross-contaminated with wheat.
If you choose to try oats, make sure they are labeled gluten free, and give them a rinse before eating them to remove any grain dust. Steel cut oats are usually less contaminated. Also, check how you feel after eating gluten-free oats to make sure you are not sensitive to avenins as well.
The bottom line here is that, whether from wheat, barley, rye or oats, gluten and brain health can affect skin, digestion, and joints. Anyone who has celiac disease should avoid all sources of gluten if they want to live a healthier, symptom-free life.
But why is it that gluten sensitivity has become such a huge problem, when a few years ago we hardly heard about it?
It is estimated that the rate of celiac disease has gone from one in 650 people to one in 100 people, with almost 30% of the American population experiencing gluten sensitivity. Since it is a largely unidentified condition, the numbers could be much higher.
One possible answer as to why gluten sensitivity has become almost epidemic in proportion is that the wheat we are consuming today is very different than the wheat from a few decades ago.
 With such a high demand for wheat products, due to growth in population as well as growth in consumption per person, the wheat industry around the world has been crossbreeding wheat with other proteins. The goal is to help it resist environmental damage and grow faster. In some cases, the wheat is modified to get more crops out of the same stalk.
With such a high demand for wheat products, due to growth in population as well as growth in consumption per person, the wheat industry around the world has been crossbreeding wheat with other proteins. The goal is to help it resist environmental damage and grow faster. In some cases, the wheat is modified to get more crops out of the same stalk.
Gluten is also sometimes put through a process to make it more water-soluble, although it is usually not, so that it can easily mix with other ingredients. This is why it is now so easily added to processed and packaged products.
Another factor is that the way we are eating has changed. While our grandparents ate a diet composed mostly of seasonal whole foods, like locally sourced fresh fruits and vegetables, we, on the other hand, are eating a lot more processed foods with much higher levels of gluten.
All of these could be plausible causes for the growing numbers of celiac disease and gluten sensitivity cases.
Unfortunately, with so many of the world’s staple foods containing gluten, it can be very difficult to switch to a gluten-free diet. However, these numbers show that gluten and brain health sensitivity is important to consider and not just for gastrointestinal relief.
When you eat a piece of bread, cake, or any other gluten-containing product, your digestive enzymes, specifically proteases, get to work on breaking it down into its component proteins, such as the glutenin and gliadin discussed above.
The special enzyme that works on gluten is called tissue transglutaminase (tTG). This enzyme is important in the relationship between gluten and brain health, so it’s important to understand its action well.
One of the functions of tTG is to keep the gut’s microvilli close together. The microvilli are hair-like structures that line the intestinal walls. They help us absorb nutrients from food.
Once the gluten has been broken down, its component proteins go through a sort of assessment. All substances that enter the gastrointestinal tract are assessed, so the body knows how to respond to them.
This assessment is carried out by the gut’s immune system, the gut-associated lymphoid tissue (GALT), which is mainly found in the small intestine. Most of the body’s immunity starts in the gut, as the gut contains two-thirds of the body’s immune tissues.
If you have gluten sensitivity, the GALT then produces antibodies, the molecules that the immune system uses to defend the body against pathogens. These antibodies perceive gluten proteins as a threat and attack them.
If you are gluten intolerant or have celiac disease, these antibodies attack not only gluten proteins but also the enzyme that breaks them down, tTG. This creates an autoimmune reaction in the body.
When the tTG enzyme is attacked, its function of holding together the gut lining is compromised. In addition, gluten can trigger the cells of the gut lining to release zonulin, a protein that modulates the tight junctions in the gut. When zonulin is released in reaction to gluten, these tight junctions begin to break apart and create gaps or leaks.
As the gut’s lining becomes more and more permeable, substances can leak into the bloodstream that are not supposed to be there, including food particles, pathogens, and toxins. This is sometimes referred to as leaky gut. When the immune system is alerted to these substances, it mounts another attack.
 In some cases, anti-gluten antibodies can also escape into the bloodstream and travel to other parts of the body, attacking healthy tissues and organs like the brain, joints, and skin. This is one of the ways gluten and brain health intolerance creates compromises that cause autoimmunity that targets the brain.
In some cases, anti-gluten antibodies can also escape into the bloodstream and travel to other parts of the body, attacking healthy tissues and organs like the brain, joints, and skin. This is one of the ways gluten and brain health intolerance creates compromises that cause autoimmunity that targets the brain.
This vicious cycle, of an immune system on overdrive with a constantly triggered inflammation response, can create a host of other issues, including other autoimmune conditions.
As research is discovering, inflammation is the root cause of many chronic illnesses. It is also at the root of many neurological and psychological issues, including depression and brain fog. This also motivates the research on the effects of gluten and brain health.
Gluten sensitivity can manifest in many different ways. These are the conditions that fall under the approved nomenclature for gluten and brain health disorders:
 Celiac disease is a genetic disorder, with a one in ten chance of inheriting it, if an immediate family member has it. If you have a parent or sibling with the condition, you should get tested.
Celiac disease is a genetic disorder, with a one in ten chance of inheriting it, if an immediate family member has it. If you have a parent or sibling with the condition, you should get tested.
However, hereditary factors are not the most reliable way to assess risk because many people with celiac disease are not aware they have it. You may have a family member with celiac disease who does not even know it.
Underdiagnosis is especially common because most people think that digestive symptoms are the only sign of celiac. Though digestive issues are among the more obvious symptoms in children, adults are more likely to experience other symptoms including:
These symptoms fall under the non-classical cases of celiac disease. There are also those who do not experience any symptoms, and only find out later when their health has sustained heavier damage. That is called asymptomatic celiac disease.
Typically, with the classical cases of celiac disease symptoms of leaky gut syndrome begin when the immune system antibodies attack the tTG enzyme, causing damage and atrophy to the microvilli. These symptoms include diarrhea, constipation, malabsorption, bloating, and abdominal pain.
If there is malabsorption, further issues can develop, including vitamin and mineral deficiencies. This is one of the reasons why many people with celiac disease and gluten sensitivity suffer from anemia and vitamin B12 deficiency as well.
 If you experience some of the symptoms of celiac disease, yet your tests for it come out negative, you might have what is called non-celiac gluten sensitivity. If you are sensitive to gluten, removing it from your diet should bring relief from your symptoms.
If you experience some of the symptoms of celiac disease, yet your tests for it come out negative, you might have what is called non-celiac gluten sensitivity. If you are sensitive to gluten, removing it from your diet should bring relief from your symptoms.
A good way to test this is by going gluten-free for one month to see how you feel. After one month, you can reintroduce gluten back into your diet to see if you feel worse. If your symptoms return after reintroduction, then you’re better off without gluten.
Just because you don’t have an autoimmune reaction to gluten doesn’t mean that it is not causing you health damage. Recent studies show that even non-celiac gluten sensitivity can cause harm to intestinal walls and create inflammation and systemic immune reactions. In these cases as well, gluten and brain health can have negative impacts.
Ataxia is a neurological condition that affects the body’s ability to control muscular coordination. It causes an array of other symptoms as well, such as fatigue, dizziness, difficulty walking, nausea, vomiting, tremors, difficulty swallowing, difficulty speaking, clumsiness, and more.
Ataxia has many causes, including trauma to the head, infections, brain surgery, tumors, alcoholism, and physical defects in the brain, spine, or brain stem.
However, some of its causes can be traced back to gluten, known as gluten ataxia. Gluten ataxia is the most obvious example of a negative relationship between gluten and brain health.
Among all ataxias, gluten ataxia has 15% prevalence, so it is somewhat common. However, it is a major cause of idiopathic (of unknown cause) sporadic ataxias, with a 40% prevalence.
 Dermatitis herpetiformis, also called Duhring’s disease, is a non-celiac skin condition caused by gluten sensitivity that creates itchy, burning blisters. Most often, these skin bumps are concentrated around the elbows, forearms, knees, and buttocks. Though from the name it sounds like it is a type of herpes, it is actually not related to the herpes virus. It is also sometimes confused with eczema.
Dermatitis herpetiformis, also called Duhring’s disease, is a non-celiac skin condition caused by gluten sensitivity that creates itchy, burning blisters. Most often, these skin bumps are concentrated around the elbows, forearms, knees, and buttocks. Though from the name it sounds like it is a type of herpes, it is actually not related to the herpes virus. It is also sometimes confused with eczema.
Although up to 15% of patients with celiac disease will also have dermatitis herpetiformis, many patients with this skin condition will actually have normal gastrointestinal and celiac blood test results. That is because, just like gluten and brain health, gluten can also affect the skin without manifesting other symptoms.
Dermatitis herpetiformis is another example where, just because celiac blood tests come out normal, it doesn’t mean that you are not gluten sensitive. Further testing and observation should be done if you have any kind of skin, joint, neurological, or gastrointestinal symptoms that don’t seem to have a specific cause. There is a possibility it’s just gluten.
Neurological symptoms associated with celiac disease have been reported as far back as 1966. However, it wasn’t until 30 years later that a case of celiac disease with solely neurological symptoms was reported.
Many celiac patients experience neurological symptoms, especially those associated with a malfunctioning autonomic nervous system. Only recently has the wider medical community has accepted the possibility that these kinds of extraintestinal presentations of gluten sensitivity can appear without gastrointestinal symptoms.
For every symptomatic patient with celiac disease, there are eight patients with no gastrointestinal symptoms. This should further underline why we need to pay more attention to gluten’s and brain health effects when there are no gastrointestinal symptoms.
These patients usually find they have celiac when they go to the doctor with joint, skin, or neurological symptoms, or some vague autoimmunity. Sometimes, even their test results will not show any gluten sensitivity. Still, it is possible they might be suffering from celiac disease or gluten sensitivity, especially if the cause of their ailment is not identified.
In the case of patients with a known neurological conditions, 5% of them have elevated gluten antibodies. But for those whose neurological symptoms have no known cause, the percentage is up to 57%.
The effects of gluten and brain health can create many neurological manifestations. This is only a partial list:
With such a wide range of effects, the relationship between gluten and brain health has led some medical professionals to say the blood-brain barrier works the similarly to the mucosal lining of the gut. This means that what’s happening in the gut is also happening in the brain. Thankfully, there are now ways to assess this.
 Recent evidence suggests that patients with newly identified celiac disease do indeed have abnormal MR spectroscopy results showing evidence of subtle cerebellar dysfunction.
Recent evidence suggests that patients with newly identified celiac disease do indeed have abnormal MR spectroscopy results showing evidence of subtle cerebellar dysfunction.
There is a possibility of molecular mimicry in the cerebellar tissue after the activation that started in the gut. This means that there could be structural or sequential similarities between the foreign antigens (gluten in this case) and the self-antigens (the body’s own molecules that trigger antibody formation).
This mimicry could result in the cross-activation from the gut to the brain. Interestingly, eye muscles are one of the first things to be activated because they are so small.
Understanding this relationship - between an immune activation at the mucosal level and a molecular mimicry that then attacks other tissues - may end up explaining conditions that we previously thought of as vague processes, including complicated autoimmune, digestive, neurological, joint, and skin issues.
With these kinds of cross-activations, we need to have a more holistic view of the effects of gluten on brain and gut health. This is especially the case with non-celiac gluten sensitivity. We must shift from viewing it as a gut illness to viewing it as a systemic illness.
To make it more complicated, in patients with gluten ataxia and those with celiac disease with no neurological manifestations, the prevalence of antibodies is up to 60%. The levels and positivity of these antibodies can be significantly reduced by switching to a gluten-free diet for both of these patient groups.
Such findings show it is becoming more and more important to go beyond conventional gluten testing.
To test for extra-intestinal manifestations of gluten sensitivity, we need to look for immunoglobulin-G (IgG) antibodies, in addition to the immunoglobulin-A (IgA) antibodies that are more commonly tested for.
That’s because patients without overt gastrointestinal issues can have antibodies that react with different tTG isoenzymes. Isoenzymes are enzymes with the exact same function but different structures. Of these isoenzymes, we know of tTG, which is sometimes called TG2, as well as TG3 which is found in dermatitis herpetiformis, and TG6 which is found in patients with neurological manifestation.
The type of antibody that is presenting shows which systems are affected by gluten, even if symptoms are slight or absent.
To illustrate how the effects of gluten and brain health can manifest, consider these three case studies that outline different ways this relationship can present.
A 42-year old man began experiencing progressive neck, shoulder, and muscle pain with a weakness in the limbs. After three weeks, he developed difficulty urinating, accompanied by a tingling sensation and sensory disturbance in his trunk and legs. At that point, he could not even climb the stairs.
He was referred to a neurologist. After some testing, problems in his visual acuity were discovered. With a pinprick examination, hemisensory loss was found on both sides. The MRI of his brain showed mild abnormalities in his white matter, with a mild generalized atrophy.
 This picture is a pretty typical multiple sclerosis (MS) diagnosis. However, to exclude the possibility of gluten sensitivity as a cause, he was tested for antibodies and other markers. The results showed he had gluten ataxia.
This picture is a pretty typical multiple sclerosis (MS) diagnosis. However, to exclude the possibility of gluten sensitivity as a cause, he was tested for antibodies and other markers. The results showed he had gluten ataxia.
This patient was then put on a gluten-free diet and given an IV of methylprednisolone, which is a steroid that helps suppress the release of substances that create inflammation. He was also put on Betaseron, a medication that helps reduce the flare-ups that occur with MS.
After 15 days, there was significant improvement.
To repair his gut and brain barriers, he was given other medications including glutathione, glutamine, probiotics, N-acetylcysteine, EPA/DHA, vitamin D, lactoferrin, xylitol, and boswellic acid. Three months later his health had improved significantly.
Ten patients with gluten sensitivity and abnormal MRIs all experienced episodic headaches. Six of them also experienced unsteadiness, and four of them had gait ataxia. All patients were put on a gluten-free diet, and nine of them had symptoms improve.
However, even though their headaches were relieved, the white matter damage did not reverse.
This doesn’t mean brain function is in inevitable decline, though damage was done. By reducing the inflammation around the brain, even if the MRI doesn’t change, brain function can go back to normal, and there are other cases where lesions in the brain have resolved.
A 30-year old man who was previously healthy began having headaches with refractory seizures, postictal right hemiparesis, and aphasia. He also had constant hemiparesis or weakness of one side of the body. These symptoms were ongoing for two years. A brain MRI revealed multiple lesions involving white and gray matter.
After going on a gluten-free diet, his symptoms were relieved, and changes were visible in his MRI. This shows it is possible to resolve some cases of epilepsy with a gluten-free diet. However, many medical professionals are unaware of the link, so the option does not cross their minds.
These three cases show that we cannot rely only on gastrointestinal symptoms as a sign of gluten intolerance because gluten can affect brain health without presenting any digestive issues.
 The adrenal glands, which produce 50 different hormones, are part of the hypothalamic-pituitary-adrenal (HPA) axis. The HPA axis is one of the body’s first responders to stress. It acts as a hormonal cascade, sending signals from the brain to the adrenals so that they release cortisol, the most important hormone in fighting stress. Gluten and brain health functions can contribute symptoms of Adrenal Fatigue.
The adrenal glands, which produce 50 different hormones, are part of the hypothalamic-pituitary-adrenal (HPA) axis. The HPA axis is one of the body’s first responders to stress. It acts as a hormonal cascade, sending signals from the brain to the adrenals so that they release cortisol, the most important hormone in fighting stress. Gluten and brain health functions can contribute symptoms of Adrenal Fatigue.
Cortisol has many important functions, such as regulating blood sugar and blood pressure, maintaining heart and blood vessel function, suppressing the immune system, and neutralizing inflammation. Once the cortisol has completed its job, any excess then signals the hypothalamus and pituitary glands to stop producing their stimulatory hormones.
The adrenal glands and the HPA axis are part of the hormone response of the NeuroEndoMetabolic (NEM) Stress Response, which is the body’s overall mechanism for dealing with stress. The NEM is made up of six circuits composed of organs and systems that work together to respond to stress. Whether the stress is physical or psychological in nature, the NEM responds.
The hormone response of the NEM is covered above. The other circuits are the metabolic response, the neuroaffect response, the cardionomic response, the inflammation response, and the detoxification response.
Sensitivity to gluten, and to foods in general, can cause an immune system reaction that can then develop into a state of inflammation in the body. Inflammation is a huge stressor on the system, and it triggers a stress response from the NEM and the adrenal glands. Chronic conditions, including celiac, as well as the malabsorption and maldigestion that can occur with it, are also huge stressors on the body.
Although the NEM and adrenal glands are equipped to handle acute, short-term stress, when the stress becomes chronic, they begin to dysregulate. The adrenal glands first increase their output of cortisol to meet the growing demand, but once they are exhausted from being overworked, their cortisol output drops, leaving the body to fend for itself against stress without its most important weapon.
This dysregulation of cortisol causes a state of Adrenal Fatigue Syndrome (AFS), with symptoms like fatigue, brain fog, anxiety, mild depression, fertility issues, sleep disturbances, easily gaining weight and difficulty losing it, heart palpitations, PMS, food sensitivity, drug sensitivity, and more.
Many AFS symptoms are similar to those of gluten sensitivity. In fact, gluten sensitivity can lead to AFS, and AFS can worsen the symptoms of gluten sensitivity.
This is especially the case in more advanced stages of AFS when the body is forced into a state of energy conservation, and there is not enough energy for the gastrointestinal tract to function properly. Some of the symptoms of this “low maintenance mode” include constipation and diarrhea.
The gastrointestinal tract, gut microbiome, immune system and the brain are part of the NEM’s inflammation response. When this system is on constant overdrive from gluten sensitivity, or from the autoimmune reaction of celiac disease, or from the effects of gluten and brain health, inflammation becomes chronic.
This can also cause dysbiosis in the gut’s microbiome, where there is an imbalance in the gut flora. And vice versa, dysbiosis can trigger inflammation as well as metabolic issues.
 One of the NEM Stress Response’s jobs is to release cortisol to help the body return to a balanced and calm state after the inflammation has done what was needed. But if there is AFS and cortisol is no longer able to suppress the inflammation, the inflammation worsens the symptoms of both AFS and gluten sensitivity.
One of the NEM Stress Response’s jobs is to release cortisol to help the body return to a balanced and calm state after the inflammation has done what was needed. But if there is AFS and cortisol is no longer able to suppress the inflammation, the inflammation worsens the symptoms of both AFS and gluten sensitivity.
This is not limited to the adrenal glands. A consistently triggered inflammation response can affect other circuits of the NEM, each one having a negative effect on the gut, gluten and brain health sensitivity.
For example, when the neuroaffect response (which is regulated by the autonomic nervous system) is dysregulated, it can also worsen depression, anxiety, insomnia, sleep disturbances, brain fog, and panic attacks.
This can include aggravating the effects casued by gluten and brain health. Depression can get worse. This is another indication that depression is caused by stubborn, low-grade inflammation.
All the circuits of the NEM affect each other, so when one dysregulates for long enough, it causes a domino effect for the rest of the system.
Brain fog is a common problem. It can be frustrating to be unable to think clearly, feel confused, have difficulty focusing, be unable to make simple decisions, have mild memory loss, or feel lightheaded and dizzy. It does seem as though a fog has come over the brain.
Though this not a clinically recognized condition, it is a symptom of other conditions, including AFS and gluten-related disorders. It is usually the result of nutritional, hormonal, biochemical, or metabolic imbalances that affect the brain.
The reason that brain fog is a common symptom of AFS is that, when the adrenals are fatigued, the body goes into energy conservation mode and slows down processes that are not immediately vital for survival. The liver clears out toxins and metabolites at a slower pace, letting them accumulate in the system. Eventually, these substances reach the brain and cause brain fog. The effects of gluten and brain health can increase this symptom.
For those with gluten-related disorders, gluten can also interfere with the hormonal and chemical balance in the brain directly. Indirectly, gluten creates a state of malabsorption, decreasing the levels of important nutrients the brain needs to thrive. These can include vitamin B6, vitamin B12, iodine, selenium, zinc, calcium, and vitamin D.
If your brain fog stems from gluten and brain health sensitivity, then your mood, cognition, mental focus, memory, and clarity should return if you change to a gluten-free diet. If your brain fog stems from adrenal fatigue as well, following the adrenal fatigue diet, taking the right supplements and managing stress will also improve your state.
 Brain fog can come from many other factors as well, though, such as sensitivity to electromagnetic fields, depression, stress, PTSD, bowel toxicity, environmental toxins, other food sensitivities, infections, nutrient deficiencies, artificial sweeteners, additives, pesticides, or certain medications.
Brain fog can come from many other factors as well, though, such as sensitivity to electromagnetic fields, depression, stress, PTSD, bowel toxicity, environmental toxins, other food sensitivities, infections, nutrient deficiencies, artificial sweeteners, additives, pesticides, or certain medications.
Brain fog can also be affected by menstrual cycles, exercise (or lack thereof), hydration, sleep, and even body temperature.
The problem is that sometimes there are several different causes of brain fog, instead of just one. In this case, you will need to be patient and stay aware of how you feel as you make one change at a time. Nutritional coaching can also help you identify food sensitivities step by step and eliminate them from your diet.
As with many autoimmune disorders, the trigger seems to be the duration of exposure to environmental factors. In the case of gluten-related disorders, the effects of a sensitivity have a lot to do with how much and how long your system has been exposed to gluten. Unfortunately, most people have been exposed since early childhood.
This is why a thorough evaluation is highly recommended as early as possible, using the most sensitive biomarkers available and a detailed history
Even if you do not have any symptoms of gluten sensitivity or any family members who have it, if you suffer from any kind of autoimmunity, you should get tested.
This is the crucial first step, but what comes next will be the more challenging phase. That is where the real recovery will take place.
After getting tested and understanding which of your systems are affected and what type of gluten-related disorder you suffer from, you will need to find a medical practitioner who is not only versed in gluten sensitivity but also knowledgeable about any other conditions you may have.
Those with celiac disease are at a higher risk of developing a second autoimmune condition, and may not even be aware of another condition present. In the haze of different and seemingly unrelated symptoms such as skin rashes and neurological problems, it can be difficult to tell what’s what.
However, it is imperative that you find out exactly what you are dealing with so that you do not aggravate one condition through taking measures indicated for another. In addition, if you are not suffering from celiac or gluten sensitivity, removing gluten from your diet is unnecessary and may backfire, depriving you of important nutrients.
Whatever other conditions you have, if you have gluten sensitivity, you need to eliminate gluten from your diet completely. Even trace amounts can cause a negative reaction, which can set your overall recovery back.
If you have severe AFS, your gluten sensitivity will tend to increase. Especially in the later stages of AFS, you can become so sensitive that even touching a wheat product can trigger a reaction. Keep in mind that recovery from adrenal fatigue does not mean your gluten sensitivity will resolve. You should still maintain a gluten-free diet.
 A strictly gluten-free version of the AFS diet is your best bet at a fast, gentle, and full recovery. There is also a possibility that some supplements that help with adrenal fatigue will contain gluten, so be sure to check labels.
A strictly gluten-free version of the AFS diet is your best bet at a fast, gentle, and full recovery. There is also a possibility that some supplements that help with adrenal fatigue will contain gluten, so be sure to check labels.
Another thing to keep in mind is that there is a tendency in those who recently found out they have a gluten-related disorder to use highly processed wheat and gluten substitutes, such as tapioca starch foods. Many of these foods can actually cause similar molecular mimicry and auto-inflammation processes, and they are best avoided as well.
Going truly gluten-free for health and vitality means more fruits, vegetables, and clean protein.
If you also have AFS, however, there are certain types of fruits you will want to avoid or limit. These include bananas, grapefruits, dates, and other potassium-rich foods. These foods aggravate the sodium-potassium imbalance that can come with AFS. You’ll also need to avoid fruits and juices in the morning because they can cause blood sugar spikes and crashes, which someone with AFS is particularly sensitive to.
To bring down inflammation, try to follow an anti-inflammatory diet rich in antioxidants. Reduce and manage your stress levels, which are the root cause of AFS as well as stress-induced inflammation. Getting enough rest, staying hydrated, and starting a gentle exercise routine will also have many health benefits.
Good health is possible, and very probable, for those with gluten sensitivity, with a functional and holistic approach to health and nutrition. The effects of gluten and brain health can be dramatically reduced over time once gluten is out of the equation. Better digestion, clearer skin, and less joint pain are also in the cards once gluten is replaced with healthy, whole foods.
It is only recently that medicine has accepted that the relationship between gluten and brain health can manifest without any gastrointestinal symptoms. This realization has led to research and new discoveries on how gluten affects the brain and nervous system.