 Magnesium, although constituting only a small fraction of bone matter, plays a disproportionately important role in maintain the optimum level of calcium in the body. This relationship becomes critical when one deals with reversing osteoporosis.
Magnesium, although constituting only a small fraction of bone matter, plays a disproportionately important role in maintain the optimum level of calcium in the body. This relationship becomes critical when one deals with reversing osteoporosis.
Magnesium acts to balance calcium in our body, much like progesterone balance the effect of estrogen, and omega-3 balances omega-6 fatty acids.
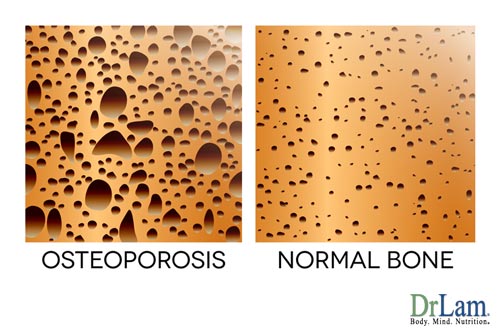
Magnesium has been shown to prevent the formation of calcium oxalate crystals, the most common cause of kidney stones. Studies have shown that 500 mg a day of magnesium reduce the recurrence rate of kidney stones by as much as 90%. Magnesium is also nature's "calcium channel blocker", preventing the entry of excessive calcium in to the cell that causes contractions, contributing to chest pain, hypertension, and arrhythmias. Magnesium deficiency can cause various abnormalities of calcium metabolism, resulting in the formation of calcium deposits in arteries. Osteoporotic women who were deficient in magnesium had abnormal calcium crystals in their bones, whereas osteoporotic women with normal magnesium status had normal calcium crystals in bone.
Magnesium balances the body's calcium supply and keeping it from being excreted. Without enough magnesium and other trace minerals, calcium ingested, especially if excessive, will be deposited not in the bone but perhaps in the wall of our arteries.
It is interesting to note that human autopsy studies have shown a close correlation between osteoporosis and abdominal aortic calcification. Since magnesium deficiency can promote osteoporosis and calcium deposit in aorta, logic follows that magnesium is likely to be the primary factor and that calcium is secondary when it comes to prevention of bone loss, which is key when looking at reversing osteoporosis.
 The use of calcium supplementation for the management of Primary Postmenopausal Osteoporosis (PPMO) has increased significantly since 1987, the year when the National Institute of Health increased their recommended daily intake of calcium to 1,500 mg for prevention of PPMO. This was done because of a study that showed that such a large dose is necessary for elderly women to maintain calcium balance.
The use of calcium supplementation for the management of Primary Postmenopausal Osteoporosis (PPMO) has increased significantly since 1987, the year when the National Institute of Health increased their recommended daily intake of calcium to 1,500 mg for prevention of PPMO. This was done because of a study that showed that such a large dose is necessary for elderly women to maintain calcium balance.
This recommendation was made adopted in spite of the different conclusions made by some clinical studies presented in the same proceedings. Results of some of these controlled studies presented showed no significant effect of calcium intake on mineral density on trabecular bone and only a slight effect on cortical bone. Since PPMO is predominately due to demineralization of trabecular bone, there is no justification for calcium mega-dosing in post-menopausal women. In fact, soft tissue calcification can be a serious risk factor during calcium mega-dosing under certain conditions. Certain investigators, notably Dr. Guy Abraham, postulated that a total dietary program emphasizing magnesium instead of calcium for the management of PPMO would be more effective for preventing bone loss and may help with reversing osteoporosis. His concerns about low magnesium for osteoporosis are similar to his concerns for women with premenstrual tension syndrome.
To test this hypothesis, 19 postmenopausal women on hormonal replacement were given a supplement consisting of 500 mg calcium (50% of RDA) and 600 mg of magnesium (200% of RDA). Serial bone density studies were conducted every 3 months. Subjects receiving the treatment showed an 11% increase in mean bone density versus 0.7% in the untreated group over a period of 9 months. With the exception of the report by Dr. John Lee, M.D, on natural progesterone therapy (which every post-menopausal women should consider), no other studies have
Dr. Abraham also showed that in postmenopausal women on hormonal replacement therapy, the magnesium emphasized program resulted in a calcaneous bone density 16 times greater than that of dietary advice alone. At the start of the study, 15 subjects were below the fracture threshold. After a year of treatment with magnesium supplementation, only 7 of them were below the fracture threshold. Unfortunately, the use of hormone replacement therapy (HRT) increase substantially the risk of estrogen related cancer such as breast and cervical cancer.
It is probably unlikely that magnesium alone is responsible for all the change reported by Dr Abraham, as Dr. Abraham's protocol include dietary changes, exercise recommendations and multiple vitamin supplementations as well. The take home lesson is that magnesium is more important than most people think. Having the optimum amount of magnesium in relation to calcium, and not the absolute level of either one in the body, is critical to preventing and reversing osteoporosis effects.
Researchers such as Dr. Abraham further postulate that PPMO is predominately a skeletal manifestation of chronic magnesium deficiency, facilitated by estrogen withdrawal during the postmenopausal period. Dr. John Lee reported significant increase in bone density through natural progesterone. Natural progesterone is an antagonist of estrogen. While estrogen prevents the osteoclast from breaking down bone, leading to increased bone density as the bone degradation process is slowed, natural progesterone actually increase the number of osteoblast that is responsible for production of bone, leading to increase in bone density.
Dr Abraham suggested raising the RDA of magnesium to 1000 mg/day and lowering the RDA for calcium to 500 mg/day. His proposed daily intake for calcium would be more in line with the World health Organization's "practical allowance" of 400 - 500 mg daily for adults. Such a reversal of the magnesium/calcium ratio would most probably lower the incidence and prevalence of many other degenerative diseases as well.
a. Eat a diet rich in magnesium such as whole grain, nuts , green leafy vegetables, and seeds.
b. Avoid refined sugar, white flour, fats, coffee,and alcholol which can deplete magnesium
c. Magnesium supplement, 300-1000 mg a day. Too much magnesium can cause loose stool that resolves if you reduce the magnesium intake. In fact, many naturally oriented doctor use this as a end point to titrate the amount of magnesium needed. Those who have renal failure should not take excessive magnesium without physician supervision.
d. Natural Progesterone cream, 20 mg a day. Postmenopausal women should take it from day 1 to day 25 of each month.
e. Strength training exercises that have been known to increase bone density. Do it.

Magnesium has been under appreciated in its role in preventing and reversing osteoporosis. The tradition model of giving calcium to magnesium in the ratio of 2:1 is outdated. Adequate magnesium is necessary for proper calcium absorption. In the early postmenopausal period, untreated women typically lose 3 to 8% of their bone mass per year. Maintaining a supplement regiment of magnesium to calcium in a one to one ratio is the most prudent approach.
For most, this means increasing magnesium intake and reducing calcium supplement intake, since most people have an over consumption of calcium and deficient in magnesium consumption. This works out to about 500 mg to 1000mg of magnesium and the same amount of calcium, depending on your diet. If you are on a high vegetable diet characteristic of Asians, chances are you are consuming about 500 mg of magnesium a day already. Therefore only 500 mg of magnesium intake in the form of supplement is needed balanced with 500 mg of calcium a day. Most American diet consumes only about 250 mg of magnesium a day (substantially less than the RDA of 350 mg), so extra supplementation is needed.
The key word is balance. In an elderly person with chronic degenerative disease, the arteries and joints are slowly calcifying. Taking in 1500 mg of calcium a day as recommended in the traditional model simply add to this insult, leading to calcium deposit in muscles and other soft tissues while being depleted in bone concurrently. This "double whammy" accelerate osteoporosis and bone loss, while increasing calcium deposit in and soft tissue at a time when we want the exact reverse - more in bone and less in outside. Fortifying with more magnesium will keep calcium balance in check and protect the bone from and may help in reversing osteoporosis.
It should be noted that measuring magnesium level is blood serum is not accurate. The best way to know your magnesium state is to measure the amount of magnesium you have inside your cell, where it counts. Ask your doctor for red pack cell studies and not serum studies of this mineral.
© Copyright 2016 Michael Lam, M.D. All Rights Reserved.

