What many people don’t know is that obesity and inflammation tend to go hand in hand. One has a tendency to influence the other, often resulting in a never-ending loop – gaining weight results in inflammation which, in turn, may trigger a set of symptoms that promotes more weight gain. And so, the cycle continues. But why is there a connection between obesity and inflammation? How does it work? And can something be done about it?
Before answering these questions, we first need to understand what is meant by the terms obesity and inflammation.
If you have a body mass index (BMI) over 30, you’re considered obese. Simply put, you’re carrying around more fat than what is healthy or the norm. With regards to BMI:

Before you start thinking all body fat is bad, you also need to recognize that some fat is essential for your health and wellbeing. Fat serves as an energy reservoir and is needed to perform certain functions in the body that don’t work without it. It’s only excess body fat, like when we talk about obesity, that begins to pose serious health risks. Among these, a higher risk of stroke, heart attack, cancers, and diabetes. That’s where inflammation comes into play.
Inflammation is linked to your body’s immune response and usually occurs when your body encounters a stressor. A wound to the knee, for example, may result in inflammation that presents as swelling, pain, heat, and even perhaps, the discharge of pus. In this instance, inflammation should subside once the stressor has been addressed, e.g., the wound starts to heal.
Systemic inflammation is chronic low-grade inflammation throughout the entire body and may be accompanied by a small rise in immune system markers in your blood or tissues. This type of inflammation—which is found in obesity—could potentially lead to the development of various health conditions, including heart problems and certain types of cancer.
There are a number of possible causes of systemic inflammation including aging, chronic infections, and even mild autoimmune conditions or an allergy. But the biggest culprit is thought to be metabolic syndrome.
Metabolic syndrome presents as a cluster of different conditions—such as obesity, poor physical fitness, sleep issues, and stress—that may increase your risk of heart disease, stroke, or Type 2 diabetes. However, just because you have one of these issues doesn’t necessarily mean you have metabolic syndrome. But it does mean you’re at a higher risk, and if you develop more of these metabolic issues, you may run the risk of developing some of the associated complications.
Taking the above into consideration, you can probably see that obesity and inflammation are very much related. What we need to understand, however, is the HOW. To understand this, we first need to understand the role of body fat.
To understand the link between obesity and inflammation, you need to understand what fat is and how it functions. Your body has two types of fat: brown adipose tissue (BAT) and white adipose tissue (WAT).
When it comes to obesity and inflammation, not much research has been conducted on BAT. What is known, however, is that all mammals have BAT – although, babies have a lot more than adults. The fat is darker in color due to a higher iron content than what is found in WAT. In adults, BAT is more predominant around the neck area.
Furthermore, the main function of BAT is believed to be generating heat by burning calories. This suggests that people with higher levels of BAT may not feel the cold as much as those with lower BAT levels.
In a study, mice with more BAT burned energy at a higher rate compared to mice with less of this type of tissue. The mice were also less likely to suffer from obesity.
Interestingly, overweight people seem to have less BAT than people of normal weight.
 One of the determining factors of obesity and inflammation is WAT since it tends to increase your risk of metabolic conditions. This type of fat is the result of consuming too many calories and storing them in your body, especially around the torso, without burning them off. This fat can be seen as a protruding belly, for example, but may also surround your internal organs. Thus, WAT is the culprit when it comes to obesity. Over one-third of the US population is considered obese and almost three-quarters are overweight. But WAT is not all bad – only excess WAT.
One of the determining factors of obesity and inflammation is WAT since it tends to increase your risk of metabolic conditions. This type of fat is the result of consuming too many calories and storing them in your body, especially around the torso, without burning them off. This fat can be seen as a protruding belly, for example, but may also surround your internal organs. Thus, WAT is the culprit when it comes to obesity. Over one-third of the US population is considered obese and almost three-quarters are overweight. But WAT is not all bad – only excess WAT.
As a specialized, connective tissue, WAT is mainly made up of adipocytes. These cells specialize in storing energy as what we commonly refer to as fat.
But WAT is not only for fat storage. The tissue produces cytokines, called adipokines, that are linked to the immune system and endocrine functions. There are two different types of adipokines: hormones (leptin and adiponectin) and inflammatory cytokines. Thus, adipokines play a role in your body’s inflammatory response, insulin sensitivity, and regulating food intake. Leptin plays a particularly important role in the latter.
In obesity, you have an unusually high percentage of WAT.
And the increase in both the size and number of fat cells can have several negative consequences. For example, you may end up with dysregulation of inflammatory mediated cytokine and adipokine production. This can throw your ratio of leptins to adiponectin out of sync.
This dysregulation can result in various conditions affecting:
Symptoms of these conditions include hypertension, Type 2 diabetes, insulin resistance, cardiovascular disease, and non-alcoholic fatty liver disease.
Excess WAT found in obese people is referred to as Excess WAT Syndrome (eWATS). If you have eWATS, you will typically have a BMI above 30, i.e., morbid obesity. The condition associated with a number of recognized disorders and risk profiles, including:
However, by identifying and proactively addressing eWATs, you could mitigate the potential health issues before they appear.
You can identify eWATs by:
A BMI above 30 accompanied caused by eWATs requires immediate intervention. This means taking measures to get rid of the excess fat.
In terms of obesity and inflammation, eWATs can result in higher-than-normal leptin production which can cause hormone imbalances, systemic inflammation, and compromised joint health, to name but a few of the potential risks.
Leptin is a hormone secreted by your fat cells, i.e., adipocytes. So more fat cells will mean more leptin. Essentially, you have a scenario in which your leptin levels correlate with your BMI. The main function of the leptin hormone is to regulate food intake and body fat storage.
Under normal circumstances, leptin increases after you eat. In doing so, the extra leptin sends a message to your hypothalamus telling it you are full, and you should stop eating. At the same time, your body increases its energy use – fat gets burned as fuel and leptin levels return to normal.
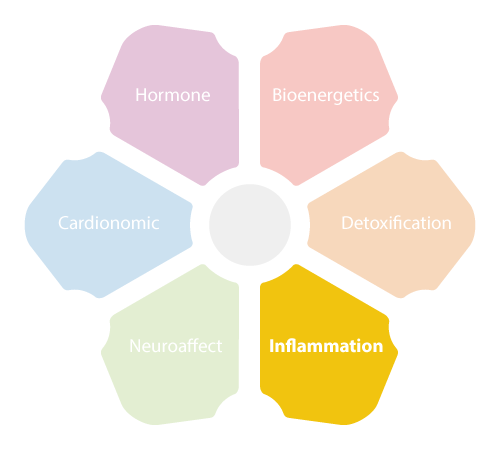 The hypothalamus, together with your pituitary gland and adrenals form what is known as the HPA axis. Your HPA axis is intimately involved in functions of the endocrine system and is connected to your body’s fight-or-flight response, otherwise known as the NeuroEndoMetabolic Stress Response or NEM.
The hypothalamus, together with your pituitary gland and adrenals form what is known as the HPA axis. Your HPA axis is intimately involved in functions of the endocrine system and is connected to your body’s fight-or-flight response, otherwise known as the NeuroEndoMetabolic Stress Response or NEM.
When obesity and inflammation come into play, however, things aren’t always so simple.
If you’re suffering from obesity and inflammation, your brain tends to resist leptin signaling so there’s nothing telling you to stop eating – referred to as reduced leptin sensitivity. This may be due to the constant increase in circulating insulin as a result of higher than normal production of the leptin hormone by excess fat cells. This can lead to overeating, increased fat storage, even more leptin, and a further decrease in leptin sensitivity. Ultimately, you gain more weight.
All metabolic tissues contain leukocytes or white blood cells, which also make up approximately one percent of your blood volume. The cells play a key role in your immune response. Their main purpose is to target viruses, bacteria, and any other foreign invaders and get rid of them. When part of your body experiences stress, for example, you scrape your knee, leukocytes rush to the site to attack the threat while blood platelets form a protective scab over the area.
Inflammation is part of the healing process and is often characterized by fluid buildup, redness, swelling, and heat. The heat is generated by increased blood flow to the injured area while pain is the result of fluid buildup putting pressure on your nerves.
The entire inflammatory response is made possible by cytokines.
The term cytokine is a general term for a group of signaling molecules—mainly proteins, peptides, and glycoproteins—that help regulate the immune system, inflammation, and hematopoiesis or blood cell production.
Some cytokines may also have autocrine actions, which means they act on the cells that secrete them; whereas paracrine signaling acts on cells in the surrounding vicinity and endocrine signaling acts on cells in other parts of the body. Moreover, cytokines may have either pro-inflammatory or anti-inflammatory properties.
Your immune system usually returns to normal once the period of stress is over and inflammation subsides.
However, with obesity and inflammation, the picture is slightly different.
 Obesity results in chronic stress and your body responds in much the same way as it would to the psychological stress you experience due to a difficult work environment, or an environmental stressor like pollution. In other words, the NEM Stress Response System comes into play and the HPA axis, mentioned earlier, calls all the shots.
Obesity results in chronic stress and your body responds in much the same way as it would to the psychological stress you experience due to a difficult work environment, or an environmental stressor like pollution. In other words, the NEM Stress Response System comes into play and the HPA axis, mentioned earlier, calls all the shots.
In addition to triggering your adrenal glands to produce an increasingly elevated amount of cortisol, your body’s automatic response is to kickstart the immune system – and inflammation as the natural result. But this can lead to a situation where there are no foreign invaders to fight off, so the chemicals your immune system releases may start to target your own body tissue. Although, please note that cortisol initially suppresses inflammation.
While this process is happening, your body attempts to repair itself by targeting and repairing the tissues under attack. But your body’s repair process may just trigger the inflammation process all over again. This can lead to a continuous cycle never allowing your body the chance to properly heal. If not addressed, this state of affairs can lead to systemic inflammation.
So, to put things into perspective, your immune system will target anything it perceives to be an enemy. It does not normally attack things it identifies as beneficial. But unfortunately, at times, your inflammation system may become dysregulated, and as a result, it may start mounting an immune response against healthy cells and tissues. This means certain antibodies no longer distinguish between normal cells and pathogens and will attack anything in their path. Regular flare-ups in the Inflammation Circuit may become the norm and are often associated with autoimmune diseases and other conditions related to inflammation.
When it comes to obesity and inflammation, osteoarthritis can be one of the consequences.
At a cellular level, eWATS is linked to osteoarthritis. In osteoarthritis, an increase of pro-inflammatory cytokines, e.g., leptin, occurs in the synovial fluid of your joints.
Synovial fluid is a clear, pale yellow viscid fluid covering the surfaces of cartilage and the synovial membrane (the membrane covering the joint). Among the components in synovial fluid, you’ll find antigen-presenting cells, mast cells, nerve fibers, and fat. The main function of synovial fluid is to lubricate your joints and reduce friction between the various components of the joint. But it also transports glucose.
In the case of osteoarthritis, we see an increase in pro-inflammatory cytokines in the synovial fluid. Leptin can be one of these cytokines. The result is inflammation of the area resulting in pain, swelling, heat, and so forth. The swelling that accompanies osteoarthritis, combined with obesity, can place a lot of pressure on your joints. This can cause increased wear and tear of the joint and may eventually compromise movement.
Osteoarthritis is caused by wear and tear from sport or a previous injury. In many cases, however, obesity and inflammation may be additional factors contributing to this condition. The dysregulation of cytokine production seen in obesity may provide the metabolic component for the development of osteoarthritis; not to mention, increased inflammation due to excess adipose tissue. Together, this increases oxidative stress.
 Both obesity and inflammation are factors that may come into play in Adrenal Fatigue.
Both obesity and inflammation are factors that may come into play in Adrenal Fatigue.
As previously mentioned, obesity and inflammation may be linked to, and play a role in functions of the HPA axis, thereby influencing your NEM Stress Response. Indeed, inflammation plays a huge role in many of the symptoms associated with Adrenal Fatigue. Among these, symptoms commonly associated with inflammation include dysregulated blood sugar levels, bloating, brain fog, anxiety, depression, and various aches and pains.
Inflammation is essentially your body’s response to stress. And obesity can be regarded as a form of physiological stress. In addition, inflammation contributes to numerous health conditions. For example, inflammation in the arteries can contribute to heart disease, inflammation in your pancreas can promote diabetes, and inflammation in the brain may contribute to the development of Alzheimer’s disease.
Health conditions with aspects of inflammation include:
In most cases, obesity and inflammation are caused by the food we eat. Much of the food in the American diet is filled with toxins and even if not toxic, may have a long-term toxic effects.
Some of these “toxic” foods and food additives include:

For example, one long-term observational study showed that both sugar and artificial sweeteners increase your risk of developing Type 2 diabetes and both may cause weight gain.
It seems that artificial sweeteners, despite containing zero calories, do not switch on your brain’s satiety hormones, which may cause you to overeat. Similarly, people who switch to artificial sweeteners may initially experience some weight loss, but long-term studies actually suggest more weight gain than loss.
Furthermore, in some people, the body may deem artificial ingredients in sweeteners to be pathogens, resulting in an inflammatory response.
Stevia, a naturally occurring sweetener, may be a better option in the long run if you’re looking for an alternative to sugar.
Conventional approaches to managing obesity and inflammation target the symptoms not the problem. For example, a low-calorie diet and medications suppress your appetite. Or with metabolic symptoms such as heart disease and osteoarthritis, the particular condition is targeted without addressing the root cause.
If you’re suffering from Adrenal Fatigue, the above approaches may add even more pressure onto your already overtaxed body. Therefore, it is necessary to make gradual changes to your overall health that support adrenal function while tackling both obesity and inflammation.
 Lifestyle modifications are some of the first changes you should implement. Obese people tend to lead sedentary lifestyles. Adding some exercise into your daily schedule may promote better blood flow and help you burn off extra calories. This doesn’t mean you have to jump off the couch and go for a 10-mile jog or join the gym. Gentle exercises, such as walking, yoga, and Pilates, are highly recommended.
Lifestyle modifications are some of the first changes you should implement. Obese people tend to lead sedentary lifestyles. Adding some exercise into your daily schedule may promote better blood flow and help you burn off extra calories. This doesn’t mean you have to jump off the couch and go for a 10-mile jog or join the gym. Gentle exercises, such as walking, yoga, and Pilates, are highly recommended.
Yoga strengthens your core muscles, promotes joint strength and flexibility, relieves stress, and gives you a whole-body workout. The benefits of Pilates include improved bone density, weight loss, stronger core muscles, improved flexibility, and improved cardiovascular health. Walking, whether timed or just taking the dog for a brisk walk can help reduce body fat, increases muscle strength, promotes bone help, improves cardiovascular health, and helps manage high blood pressure, high cholesterol, joint pain, and diabetes.
You should check with your physician first to make sure your body can tolerate a certain type of exercise before making drastic lifestyle changes. Your body must be in the right condition before making these changes.
In terms of diet, obesity and inflammation can be managed, to a large extent, by making the right food choices. Correct food choices don’t mean following a low-calorie diet and taking the latest diet pills, potions, or powders. Instead, it’s best to gradually incorporate healthier foods into your diet and start to slowly cut down your portion sizes. But not too quickly as you don’t want your body to think you’re starving it. Once your body goes into starvation mode, it may hang onto fat as if your life (literally) depended on it.
The first port of call is cutting out foods high in fats and sugars and staying away from processed foods and takeout. The second step is to introduce nutritious whole foods into your diet that actively target and fight inflammation while providing adrenal support.
Foods with anti-inflammatory properties that provide adrenal support include:
 When it comes to obesity and inflammation, your aim should be to reduce visceral fat and lower systemic inflammation. You should also implement efforts to normalize leptin production, for example, by making lifestyle changes and changing your attitude towards your diet. If you are suffering from AFS, it’s important to seek the guidance of an AFS specialist who can help get you started on the right track to recovery. If you’re dealing with obesity and inflammation, you may need to start exercising and losing weight slowly. There is no one size fits all solution, so find a health coach that can give you a personalized recovery plan – one that involves treating any underlying problems causing your AFS and helping you with your obesity and inflammation along the way.
When it comes to obesity and inflammation, your aim should be to reduce visceral fat and lower systemic inflammation. You should also implement efforts to normalize leptin production, for example, by making lifestyle changes and changing your attitude towards your diet. If you are suffering from AFS, it’s important to seek the guidance of an AFS specialist who can help get you started on the right track to recovery. If you’re dealing with obesity and inflammation, you may need to start exercising and losing weight slowly. There is no one size fits all solution, so find a health coach that can give you a personalized recovery plan – one that involves treating any underlying problems causing your AFS and helping you with your obesity and inflammation along the way.
There are many possible factors responsible for a heart condition. For example, you can inherit a predisposition to heart arrhythmias or high cholesterol. But yes, according to research, obesity and inflammation may also be factors contributing to a number of heart-related issues.
