 Your nervous system is composed of different types of cells: neurons and glial cells. Each type affects and is affected by its surroundings – the neuronal microenvironment.
Your nervous system is composed of different types of cells: neurons and glial cells. Each type affects and is affected by its surroundings – the neuronal microenvironment.
Neurons are the cells that communicate electrical and chemical signals throughout your nervous system. They are the ones that carry orders from your central nervous system (CNS) to your muscles and organs and, as such, also report back to your brain and CNS.
Glial cells are the support cells of neurons. They include astrocytes, which help nurse neurons by supplying them with nutrients from the blood supply. Microglia are the immune cells of the nervous system. There is crosstalk between astrocytes and microglia. Oligodendrocytes are responsible for myelinating neurons. Myelin is a kind of protective sheath that also helps electrical signals pass through the neurons more quickly.
Glial cells outnumber neurons by manyfold, and though they mainly play supportive roles to neurons, they are also implicated in many neurodegenerative diseases. For example, if oligodendrocytes aren’t functioning properly, you can get problems with myelin production.
Neurodegenerative diseases are on the rise, and there are several possible reasons why. First of all, because they are usually age-related and life expectancy has increased dramatically over the last century or so, it makes sense that these diseases are becoming more prevalent. But there are other contributing factors. And some of these diseases do affect the young. One underlying cause for almost all of them is an unsafe neuronal microenvironment that can include neurotoxic or neuroinflammatory elements.
In this article, we will discuss what kind of diet and lifestyle factors could affect the neuronal microenvironment and how you can improve its state, support microglial function, and even reverse demyelination.
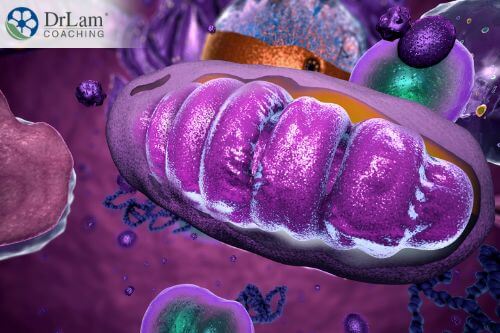
The Cell Danger Response (CDR) is important to understand when we’re dealing with chronic conditions. It’s basically the defensive state of a cell, when it has sensed there is a threat in its microenvironment.
Cells cannot go into repair or restoration while their CDR is on since they’re using all of their resources to defend themselves. It’s only after the CDR is switched off that they allocate their resources towards repairs.
Microglia are the nervous system’s immune cells. And they have three main states:
These are the same states that macrophages, the immune system cells outside the nervous system, operate in. Mitochondria also exist in these states.
M1, the activated state, happens when a threat is present and the microglia are activated. That’s when immunity is triggered and they secrete pro-inflammatory cytokines to attack whatever they see as a threat.
If the threat is taken care of and the microenvironment seems safe again, then they shift to the state of repair and restoration, M2.
In the M0 state, the microglia are just scanning and patrolling. They move around the neuronal microenvironment checking for any threats but they’re not reactive. They haven’t committed to either the M1 or M2 state yet - meaning they haven’t committed to attack or to repair.
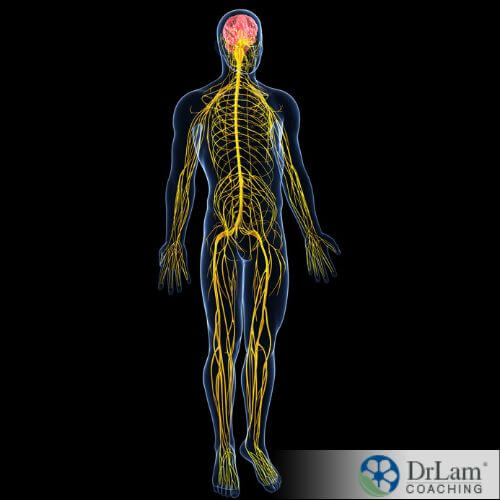
 Mitochondria are membrane-bound organelles inside cells, and their main function is to produce adenosine triphosphate, or ATP. ATP is the energy currency of life, and it’s the energy that cells need in order to power their biochemical processes.
Mitochondria are membrane-bound organelles inside cells, and their main function is to produce adenosine triphosphate, or ATP. ATP is the energy currency of life, and it’s the energy that cells need in order to power their biochemical processes.
There are different mitochondrial states as well, depending on the need of the cells they inhabit. For our purposes, we’ll be focusing on M0, M1, and M2 mitochondria, which align with microglial states. These specific types of mitochondria are small and round, and all three of them are needed for neurons to recover from injuries.
These three types of mitochondria exist in different proportions within the cells. What determines what state they all shift to is what is going on in the neuronal microenvironment.
Other factors can contribute to which state is the most dominant, including your age, genetics, diet, and lifestyle. This means that, to a large extent, you can influence your microglial and mitochondrial function, which can in turn influence the repair and reconnection of your neurons.
These states help describe how cells, mitochondria, and microglia come together to fight and heal from injuries. Their reactions depend on what state their Cell Danger Response is in.
The Cell Danger Response also goes through three main stages.
The different naming of the CDR, microglia, and mitochondria states can be a little confusing, so it might help to summarize it like this:
CDR1 is the defensive state the cell goes into when there is infection or trauma. This CDR1 state triggers innate immunity, and it uses M1 microglia and mitochondria. The microglia are taking pro-inflammatory action and the mitochondria are producing energy through anaerobic glycolysis. The cells leak ATP, so extracellular ATP increases.
CDR2 is the state of cell growth once the threat has been dealt with. It utilizes the microglial and mitochondrial M0 repair states, with energy production coming through aerobic glycolysis. This is the state that allows the rebuilding of cell tissues and stem cells.
CDR3 is the third stage of the cell danger response, and it utilizes the microglial and mitochondrial M2 patrolling states. The energy is produced using the process of oxidative phosphorylation. The purpose here is to help cells remodel their tissues and connect with neighboring cells.
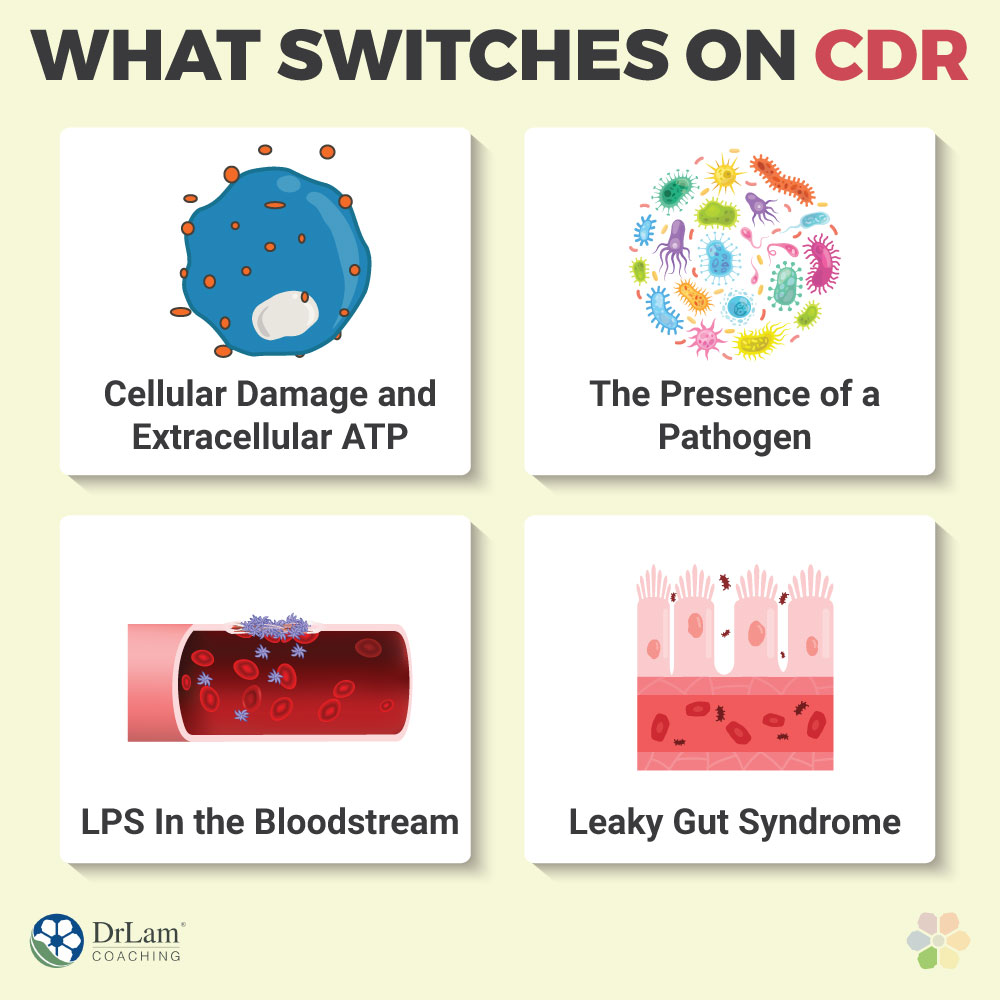
But how does a cell know to switch the CDR on in the first place? The major clues are in the neuronal microenvironment.
The health of a nervous system cell is determined by not only what’s inside of it, but also by the microenvironment it is exposed to – what’s outside the cell. The neuronal microenvironment is basically the immediate surroundings of a nervous system cell. That's true for both neurons and glia. It includes things like the extracellular matrix, the interstitial fluid, any substances in that fluid, and nearby cells.
 Several things in the cell’s internal and external environment can signal to it that something is wrong. That there is threat or danger to its health that merits the Cell Danger Response to be switched on. When the microglia and mitochondria need to shift to stage M1.
Several things in the cell’s internal and external environment can signal to it that something is wrong. That there is threat or danger to its health that merits the Cell Danger Response to be switched on. When the microglia and mitochondria need to shift to stage M1.
The following are three major signs cells can pick up on and that can turn the CDR on.
Protein fragments in the cell’s external environment that match the proteins that are supposed to be inside the cells are a sign of danger – they signal that there is cellular damage that caused these proteins to spill out.
The presence of extracellular ATP, in this case when the cells have released ATP into the neuronal microenvironment, is that kind of danger signal. It tells the cells that something has damaged them and their mitochondria and allowed the ATP to escape externally. So that leads them to switch their defenses on. In this case, the microglia’s pro-inflammatory cytokines will attack and dissolve the damaged cells.
If a pathogen is in a cell’s microenvironment, that is a clear sign of danger for obvious reasons. The way it works is that, if there are proteins or protein fragments in the neuronal microenvironment that match viral or bacterial proteins, the nervous system’s immunity will be triggered. In this case, the microglia’s pro-inflammatory cytokines will attack the pathogen.
LPS, or lipopolysaccharides, are protein fragments that turn on the danger signal. They can enter the bloodstream by way of a leaky gut. This means that the tight junctions in the gut’s lining have loosened (we'll explain how this happens later). They are allowing substances into the bloodstream that shouldn’t be there. That includes things like pathogens, toxins, food particles, and protein fragments.
In some cases, these substances can cross the blood-brain barrier. So, if LPS enters the CNS and the microglia sense their presence, they will go from the M0 state to the M1 state. This wouldn’t be a big problem if it was a one-off incident. But having a leaky gut can create a chronic issue by causing this to happen constantly. The LPS is constantly entering the bloodstream and triggering immune reactions over and over again.
Here’s the thing to understand about immune reactions. Sometimes they are acute, and sometimes they are chronic. And this means different things for your body.
Acute reactions will create acute inflammation. That means it’s a short-lived phase that goes away once the danger has been dealt with. That’s the natural and healthy form of inflammation, and it’s absolutely necessary for the survival of nervous system cells and the entire organism. In this case, you.
But when the immune system is constantly triggered and inflammation becomes chronic, then the reactive state is always on. The reactive state, M1, with its increased levels of pro-inflammatory cytokines, can damage the neurons, their synapses, and the oligodendrocytes that create myelin. This is one way to trigger or increase neurodegeneration. The most well-known myelin-related neurodegenerative condition is multiple sclerosis. But chronic inflammation is one of the most common root causes of neurodegeneration and of chronic conditions in general.
 Inflammation is also one of the six circuits of your NeuroEndoMetabolic (NEM) Stress Response, your body’s global response to stress. Your NEM is composed of a network of organs and systems that work together to fight off stress, whether physical or psychological in nature. Its six circuits are the Hormone, the Bioenergetics, the Cardionomic, the Neuroaffect, the Inflammation, and the Detoxification circuits.
Inflammation is also one of the six circuits of your NeuroEndoMetabolic (NEM) Stress Response, your body’s global response to stress. Your NEM is composed of a network of organs and systems that work together to fight off stress, whether physical or psychological in nature. Its six circuits are the Hormone, the Bioenergetics, the Cardionomic, the Neuroaffect, the Inflammation, and the Detoxification circuits.
Each of these circuits has three main components which are interlinked with other circuits and each other, and they work together to support certain aspects of your health. The three main components of your Inflammation Circuit are the gut, the microbiome, and the immune system.
Your microbiome is the combination of different bacteria that inhabit your gut. If they’re in balance, it means there are enough “good” bacteria to keep the harmful ones in check. But, due to different factors, your microbiome can become out of balance. This state is called dysbiosis, and it can lead to the junctions in your gut’s lining opening up and creating leaks. If this situation becomes chronic, you can then end up with leaky gut syndrome.
With a leaky gut, substances are constantly entering your bloodstream, causing an immune reaction. The immune reaction brings with it inflammation. Constant inflammation in the gut will eventually travel to other areas of the body, including the brain and nervous system. In fact, the three main components of the Neuroaffect Circuit are the microbiome, the brain, and the autonomic nervous system (ANS), which is the part of your nervous system that you don’t consciously direct.
That’s how inflammation and the nervous system are connected in our NEM model – via the microbiome. In fact, the health of your microbiome is a cornerstone of your overall health, whether you’re dealing with CNS dysfunction or hormonal imbalances or metabolic issues.
For these reasons, we look at whether our clients have a leaky gut anytime they complain of neuropsychiatric symptoms. Those include brain fog, anxiety, mild depression, cognitive decline, and insomnia, among others. If you’re not sure whether you have leaky gut syndrome or not, you can give us a call to discuss possible tests and options for recovery.
In both of the NEM circuits mentioned, and in the body overall, chronic inflammation becomes the major stressor, more so than the pathogen, injury, or food-related protein fragments that triggered it. And chronic stress usually leads to adrenal fatigue.
Adrenal Fatigue Syndrome (AFS) is a condition that results from chronic stress. Your adrenals are your NEM’s first responders. They are the glands that produce your body’s main anti-stress hormone, cortisol. And when the stressor is constantly there, they can become overworked and eventually exhausted.
 In the beginning stages of AFS, the adrenals increase their cortisol production. But in the more advanced stages, they are so exhausted that their cortisol output drops completely. And although cortisol naturally fluctuates throughout the day, beyond a certain level, it can cause a lot of issues. So anything above or below the healthy range is a problem. Too much cortisol will cause more inflammation, as will too little.
In the beginning stages of AFS, the adrenals increase their cortisol production. But in the more advanced stages, they are so exhausted that their cortisol output drops completely. And although cortisol naturally fluctuates throughout the day, beyond a certain level, it can cause a lot of issues. So anything above or below the healthy range is a problem. Too much cortisol will cause more inflammation, as will too little.
Symptoms of AFS include fatigue, weight gain, sleep disturbances, brain fog, anxiety, mild depression, an inability to handle stress, PMS, loss of libido, infertility, dry skin, brittle nails, hair loss, hypoglycemia, salt and sugar cravings, unstable blood pressure, lowered immunity, food and drug sensitivities, and digestive issues.
The reason the symptoms are so varied is because, when you have AFS, your entire NEM can dysregulate. And, as you can see, there are quite a few neuropsychiatric symptoms involved.
When you have AFS and NEM dysregulation, you are more susceptible to intestinal permeability and food and drug sensitivities, as well as blood-brain barrier permeability. This means that the neuronal microenvironment might end up having more LPS, pathogens, and toxins, which can then trigger CDR. Also, with AFS many people have a lack of sleep and difficulty exercising due to fatigue, which can also increase the reactivity of microglia and prolong their M1 phase.
Research is uncovering just how important the connection between your gut and brain is. How communication between them is bidirectional, and how involved your microbiome is in that crosstalk.
Your gut makes three-quarters of your neurotransmitters – the chemicals used by your nervous system to communicate. Your microbiome has an effect on these neurotransmitters and on the conditions that can lead to leaky gut and chronic inflammation. But that’s not all. Did you know that your gastrointestinal (GI) tract has its own nervous system? It’s called the enteric nervous system (ENS), and it is the biggest component of your ANS. It can function and regulate itself without the direct involvement of your CNS.
All of these connections between your gut, microbiome, ENS, and CNS mean that when one is affected, so are the others. We’ve already seen what happens when you have dysbiosis and leaky gut – the chronic inflammation that travels to your brain and nervous system and creates an unhealthy neuronal microenvironment. But psychological stressors can also trigger or worsen GI tract issues, like irritable bowel syndrome or acid reflux.
Also, psychological stress can dysregulate the adrenal glands just as much as physical stressors do. And that can lead to AFS and issues with cortisol, which can create more inflammation and dysbiosis. This is why we always approach health holistically with our clients. We look for root causes and devise programs that support you in changing your diet, lifestyle, mental health, and environment.
And when it comes to the neuronal microenvironment and neuroinflammation, there are a few specific things that we find are common causes for the CDR being switched on: mainly diet, exercise, sleep, stress, and exposure to toxins. And what’s helpful about looking at these five components is that they are the same ones we need to look at for AFS and NEM dysregulation.
The good news is that, if you work on these five areas, you have a good chance of improving your neuronal microenvironment.
 There are many ways that what you eat influences your neuronal microenvironment and the reactivity of your microglia.
There are many ways that what you eat influences your neuronal microenvironment and the reactivity of your microglia.
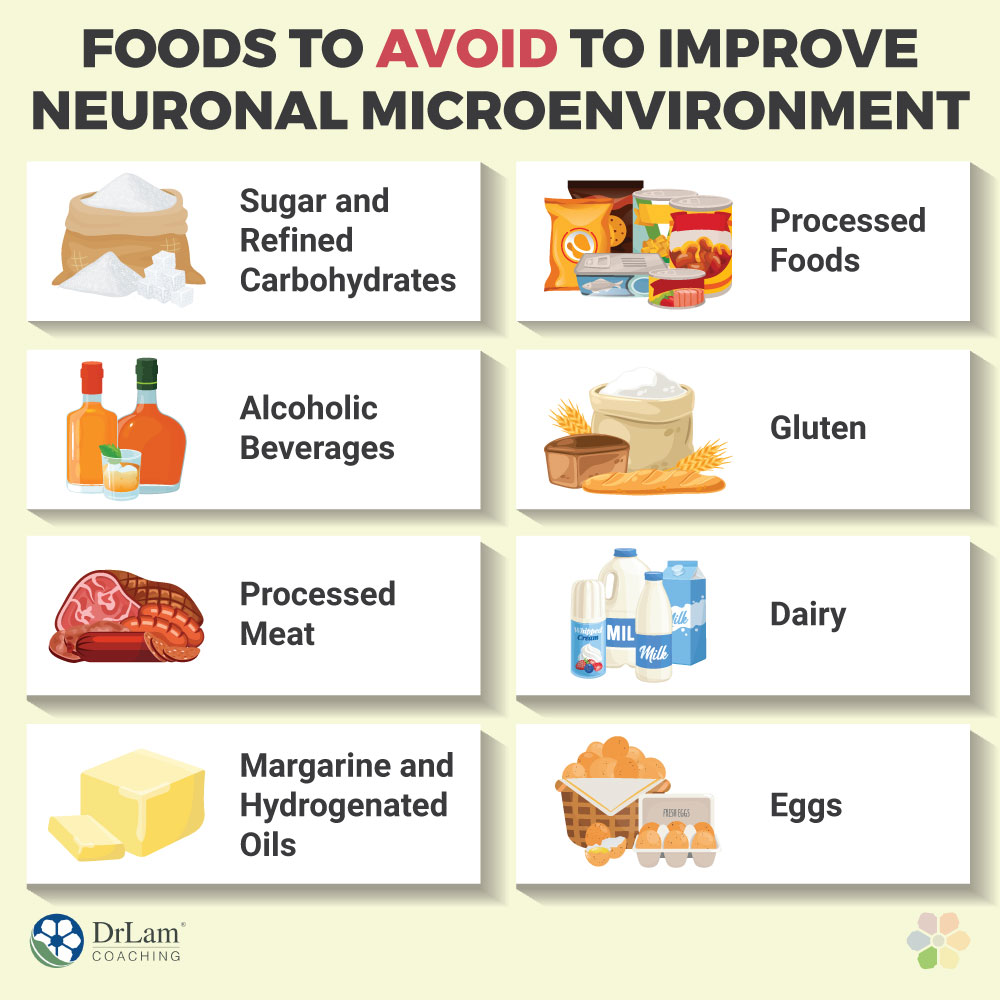
First of all, there are foods we can consider as generally inflammatory. They create inflammation in pretty much everyone to varying degrees. Then, there are foods that only some people are sensitive to or intolerant of. Meaning, not everyone shares that sensitivity. Then, there are foods that affect your blood sugar levels in a way that creates stress, such as by spiking them too quickly and leading to insulin flooding your system.
All of these can lead to higher levels of inflammation in your system and create problems in your neuronal microenvironment.
There are a few foods and beverages that create inflammation without you being specifically sensitive to them. They include the following:
Sugar and refined carbohydrates are foods that can quickly spike your blood sugar levels. They are very easy to digest, and they enter your bloodstream all of a sudden, causing your pancreas to flood your system with insulin. This excessive insulin will then drop your blood sugar levels too low, causing hypoglycemia. Then, when you have hypoglycemia, your body sends a danger signal that tells you to eat more sugar.
These cycles of spikes and crashes are extremely stressful on your body. Your adrenals secrete more cortisol and your whole body goes into overdrive. Also, hypoglycemia can be very damaging to your brain and nerve cells. Your brain needs glucose as fuel in a sustained manner, so when its supply is suddenly cut, brain cells may starve and die off. Hypoglycemia, unfortunately, is a common symptom in AFS.
The other big problem with simple carbs and sugars is that they feed the “bad” bacteria in the gut, causing dysbiosis. And what’s more, sugar seems to decrease the anti-inflammatory capabilities of omega-3 fatty acids. This is not to mention the problems with weight gain that it can lead to as well.
Fructose from fruits and carbohydrates from whole grains and vegetables are different. They release their sugars relatively slowly, because the digestive tract has to break down the fibers to release those sugars.
Although moderate alcohol use is fine for most people, and in fact, can even be beneficial, too much of it can wreak havoc on your health. First of all, there is the problem of dependency. Alcohol has inflammatory effects on the body as well.
Alcohol can erode the gut’s lining, as can sodas, which often accompany certain alcoholic beverages. This can then lead to a leaky gut and even allow the toxins released from the bacteria in the microbiome to enter the bloodstream.
A few years ago, the WHO classified processed meat as carcinogenic. More specifically, processed meat is associated with stomach and colon cancer. It’s also associated with an increased risk of other chronic conditions, such as diabetes and cardiovascular disease.
This includes sausage, pepperoni, bacon, and lunch meats, among others.
 When you cook processed meat, especially at high temperatures, they release substances called heterocyclic amines (HCAs) and polycyclic aromatic hydrocarbons (PAHs) that are inflammatory. These substances can also cause DNA changes that lead to cancer. And because many people cook their processed meats with trans fats, they become even more inflammatory.
When you cook processed meat, especially at high temperatures, they release substances called heterocyclic amines (HCAs) and polycyclic aromatic hydrocarbons (PAHs) that are inflammatory. These substances can also cause DNA changes that lead to cancer. And because many people cook their processed meats with trans fats, they become even more inflammatory.
Margarine and partially hydrogenated oils contain a type of trans fat that is artificially created. They are the result of a process that turns liquid unsaturated fats into solid fat by adding hydrogen to them. For example, this is how we get most types of margarine. But they’re also added to processed foods, usually under the label of "partially hydrogenated oil."
Natural trans fats, such as the ones you get from eating meat and dairy, are not as inflammatory as the artificial kind. They can affect your cholesterol levels, arterial function, and heart health.
Most types of processed foods are unhealthy because they contain some of the inflammatory foods mentioned here. Many contain a lot of added sugar and partially hydrogenated oils. They may also include synthetic chemicals, such as preservatives and artificial flavors or colorings, which are inflammatory as well.
Unfortunately, the Standard Western Diet contains a lot of processed foods, sugar, trans fats, artificial chemicals, and refined carbs. It’s also quite low on fiber and many important vitamins and minerals.
Other than consuming the generally inflammatory foods listed above, your inflammation may also be related to specific sensitivities. Many people are sensitive to certain foods and don’t even know it. Part of the problem is that not all food sensitivities manifest as GI tract issues. In fact, some of them might present only neuropsychiatric symptoms, prompting you to look for psychiatric solutions.
Recently, science is showing just how much depression is due to chronic low-grade inflammation. And this may extend to many other neurological and psychiatric conditions as well. That's why it's important to consider food sensitivities as a possible factor in neurological issues, even if you may not be experiencing the more common digestive issues.
Gluten is one of the foods most commonly involved in leaky gut syndrome. It can create symptoms like brain fog, headaches, anxiety, ADHD-like symptoms, seizures, tingling or numbness in the extremities, and depression. These are all neuropsychiatric symptoms brought about by the neurotoxicity gluten creates in the neuronal microenvironment.
Other non-GI symptoms include bone loss, arthritis, joint pain, liver issues, skin rashes, issues with menstruation, infertility, and anemia. Of course, like any food sensitivity, you may also experience GI issues like diarrhea, constipation, bloating, abdominal pain, acid reflux, nausea, and vomiting.
 The mechanism behind this is, when you ingest gluten, a specific type of enzyme is released by your gut to break it down. This is called the tissue transglutaminase (tTG) enzyme. The protein components of gluten that remain after tTG breaks it down then have to be checked by your gut’s immune system. If you’re not sensitive to gluten, then your gut’s immune system, which is called the gut-associated lymphoid tissue (GALT), does nothing. But if you are sensitive to it, then your GALT reacts.
The mechanism behind this is, when you ingest gluten, a specific type of enzyme is released by your gut to break it down. This is called the tissue transglutaminase (tTG) enzyme. The protein components of gluten that remain after tTG breaks it down then have to be checked by your gut’s immune system. If you’re not sensitive to gluten, then your gut’s immune system, which is called the gut-associated lymphoid tissue (GALT), does nothing. But if you are sensitive to it, then your GALT reacts.
As with any immune response, the GALT secretes antibodies to attack the proteins. Remember how microglia patrol your CNS for protein fragments that resemble pathogens or extracellular ATP? It’s a similar process. But these antibodies can also attack the tTG that broke down the gluten in the first place.
This attack on tTG compromises your gut’s lining, creating leaks, because tTG is one of the things that holds the tight junctions in place. The leaks will then allow the gluten’s protein fragments into the bloodstream, along with other substances like toxins or pathogens. These then can travel to the brain and create neurotoxicity and neuroinflammation there.
Dairy milk contains a type of protein called casein that has been associated with certain neurological and psychiatric symptoms. More specifically, one type of casein causes gut cells to have fewer antioxidants when it is metabolized. With fewer antioxidants, you get more oxidative stress.
When free radicals are roaming your system, especially in your CNS, they will switch the CDR on. And oxidative stress is one of the major factors in neurodegeneration and neuroinflammation.
Symptoms of dairy sensitivity are similar to those of gluten sensitivity, and they can include brain fog, fatigue, diarrhea, bloating, constipation, abdominal pain, arthritis, joint pain, acne, and eczema.
Eggs are generally healthy foods that are quite nutrient-dense. So, for healthy people, you wouldn’t normally consider cutting them out. But if you have chronic inflammation or inflammatory conditions, including digestive tract issues and neuropsychiatric problems, you may want to try eliminating them for a while to check if you get an improvement in your condition.
Then, you can reintroduce them back into your diet to see if your symptoms come back. If so, then it might be a good idea to cut them out for good and find other ways of getting the same kind of nutrients they provide.
The process above, of cutting eggs out of the diet to see if they cause problems and then slowly reintroducing them to see in the problems come back, is actually the gist of an elimination diet. This is generally the gold standard of testing for food sensitivity.
But if you prefer to get food sensitivity tests done, we offer those at our Lam Clinic, as well as many other functional tests that can help us determine the best nutrition plan for you.
 Gluten and dairy are foods we frequently suggest our clients eliminate. The adrenal fatigue diet is more focused on whole non-wheat grains, fruits, vegetables, and healthy sources of animal protein, like wild-caught fish.
Gluten and dairy are foods we frequently suggest our clients eliminate. The adrenal fatigue diet is more focused on whole non-wheat grains, fruits, vegetables, and healthy sources of animal protein, like wild-caught fish.
On top of an elimination diet, you should try to increase your fiber intake and eat fermented foods that can diversify your microbiome and bring back its balance. Certain other foods, like bone broth, might speed up the healing process of gut leaks as well.
There are many diets out there that can be quite beneficial for the health of your CNS and that can dramatically improve your neuropsychiatric symptoms. They include the Mediterranean diet, a pescatarian diet, a plant-based diet, and our adrenal fatigue diet. These diets are much better alternatives to the Standard Western Diet, but they still need to be planned out well, especially if you’re just starting out.
There are certain nutrients that you can focus on when planning your diet and supplement regime that can be very helpful. They can create a safer microenvironment, reduce inflammation, decrease oxidative stress, improve the health of your microbiome, and help your microglia and mitochondria to function more effectively.
Let’s start with your microbiome, because it is central to all the rest. As mentioned, it helps to incorporate more fiber, fermented foods, and bone broth into your diet. You can also consider taking a high-quality probiotic supplement. At least until your microbiome has had the chance to get into a strong and healthy state and your new diet is well-established.
For reducing neuroinflammation, some excellent supplement choices include omega-3 fatty acids, vitamin D, vitamin B12, and folate. To help with oxidative stress, vitamin C and glutathione are also good. To support the remyelination process, there’s vitamin K, lithium, melatonin, lipoic acid, niacin, and cholesterol.
Many spices have anti-inflammatory properties. Some have performed in remyelination studies with promising results. They include curcumin, thyme, rosemary, quercetin, licorice, resveratrol, and black cumin seeds.
This list can be confusing, and it is not meant for you to implement alone. It is a list you can take to your healthcare practitioner to discuss what you can safely incorporate into your cooking and supplement plans.
That brings us to a very important precaution: it may not be a good idea to create a supplement plan yourself. Please avoid the shotgun approach of taking a bunch of different supplements and spices hoping something works. The best-case scenario here is that you won’t know which helped and which are a waste of your money. The worst-case scenario is that they may actually make your condition worse.
If you have AFS, especially the more advanced stages, you are at risk of getting paradoxical reactions and even adrenal crashes. In this case, the body's systems are too weak and detoxification is congested, such that the metabolic byproducts of these supplements can actually add more stress on your body. You need the expert guidance of someone who knows the delicate balance of supplements, diet, and lifestyle factors to help you navigate your recovery.
When your neuronal microenvironment is not safe, and your CDR is switched on, your microglia are stuck in M1 and M2 activation. This is abnormal and is associated with a higher risk of Parkinson’s disease, ALS, Alzheimer’s disease, multiple sclerosis, and cognitive decline. Non-food-related lifestyle factors that can increase M1 and M2 activation include leading a sedentary lifestyle, sleep deprivation, and stress. Therefore, we need to look at each one and how to improve it.
 Sleep is the second most important thing to improve after diet. It is truly a cornerstone of health and proper recovery. It is important to create a good sleep hygiene routine to have the best chance of getting good quality sleep. That can include things like keeping your room cool and dark, turning off your phone, turning off screens at least two hours before bed, avoiding drinking liquids also two hours before bed, and using a nightlight instead of the big bathroom light if you need to use the toilet at night.
Sleep is the second most important thing to improve after diet. It is truly a cornerstone of health and proper recovery. It is important to create a good sleep hygiene routine to have the best chance of getting good quality sleep. That can include things like keeping your room cool and dark, turning off your phone, turning off screens at least two hours before bed, avoiding drinking liquids also two hours before bed, and using a nightlight instead of the big bathroom light if you need to use the toilet at night.
Exercise is a little trickier if you have AFS. Although physical activity is very important for your CNS’s health, it can actually worsen your AFS. Especially if you overdo it. With AFS recovery, we recommend gentle forms of exercise like adrenal breathing and adrenal yoga at first. Then, once your adrenals are strong again, you can intensify. In fact, exercise is also very helpful for stress management.
Stress comes in good and bad forms. Your body needs some amount of stress. Your cells need to go through cycles of mild to moderate stress and recovery to maintain their health. Exercising and then resting is one way to accomplish that.
But chronic stress is a different thing altogether. As we’ve seen, it can dysregulate your adrenals and your entire NEM, and also create an unsafe neuronal microenvironment. This is why stress management should be another top priority. Things like meditating, mindfulness, adrenal breathing, adrenal yoga, walks in nature, journaling, and going to therapy and support groups are all good options.
Your neuronal microenvironment is an important factor in your brain and nervous system’s health. Pathogens, toxins, and certain substances can pass through the blood-brain barrier and create issues there. Also, if your neurons are damaged and leak ATP extracellularly, that is another signal that there’s a problem.
When your microglia notice these threats, they switch states. They go from patrolling to reactivity, increasing the production of their inflammatory cytokines as part of the immune defense. Cells in the area will also go into the cell defense response. Once the threat has been dealt with, the microglia and mitochondria shift states and the cells can then repair themselves and reconnect to their neighbors.
If the CDR prolongs and the microglia are in a continuous M1 and M2 state, however, you’ll start to get neuropsychiatric issues. Your risk for neurodegeneration increases as well. So one of the most important preventative and recovery strategies you can take up is focusing on creating a safer neuronal microenvironment that will allow your CDR to switch off and your microglia and mitochondria to shift back to the M0 state.
You can improve your neuronal microenvironment naturally in several ways, including diet, supplements, sleep, stress management, and exercise. Cognitive training can also help reverse some of the decline you may have experienced. But the exact strategy needs to be customized to your specific goals and needs. If you’d like to see how we can help you, you can call us for a free initial consultation with one of our coaches.
The neuronal microenvironment is everything that surrounds a neuron. The extracellular matrix and the fluid there as well as substances in the fluid and neighboring cells. It’s crucial to maintain its health if you want to protect your brain and nervous system from inflammation and neurodegeneration.