 Low stomach acid, also called hypochlorhydria, is a condition that a lot of people have. It’s when your stomach doesn’t produce enough hydrochloric acid (HCl), which is needed to break down food and kill pathogens that enter the stomach. As you can imagine, food that is not properly digested can create a lot of issues in the gastrointestinal (GI) tract, as can viruses and bacteria that enter the body through the stomach.
Low stomach acid, also called hypochlorhydria, is a condition that a lot of people have. It’s when your stomach doesn’t produce enough hydrochloric acid (HCl), which is needed to break down food and kill pathogens that enter the stomach. As you can imagine, food that is not properly digested can create a lot of issues in the gastrointestinal (GI) tract, as can viruses and bacteria that enter the body through the stomach.
This is why it’s important to ensure your stomach HCl levels are in the right range - not too high and not too low - as both extremes can be stressful on the body. In fact, there are several conditions that have been associated with a reduction in stomach acid, such as allergies, thyroid problems, gastritis, osteoporosis, acne, eczema, psoriasis, pernicious anemia, asthma, lupus, and other autoimmune disorders.
Symptoms of low stomach acid include:
A lot of these symptoms are shared with other GI tract disorders, and because GI tract disorders are so common, not everyone who experiences these symptoms will go get them checked out by a doctor. Many people simply endure the symptoms or take over-the-counter medications, such as acid blockers, thinking this will help. Unfortunately, this will only let the condition progress, since it doesn’t address the root causes, and it may even aggravate it.
 When left untreated, low stomach acid can trigger or worsen some of the conditions mentioned above, but one of its main risks is that it can trigger inflammation in the GI tract, which can lead to dysregulation your NeuroEndoMetabolic (NEM) Stress Response and cause Adrenal Fatigue Syndrome (AFS).
When left untreated, low stomach acid can trigger or worsen some of the conditions mentioned above, but one of its main risks is that it can trigger inflammation in the GI tract, which can lead to dysregulation your NeuroEndoMetabolic (NEM) Stress Response and cause Adrenal Fatigue Syndrome (AFS).
Your NEM stress response is the collection of organs and systems that fight stress, and it’s made up of six circuits: the Hormone, Bioenergetics, Cardionomic, Neuroaffect, Inflammation, and Detoxification circuits. The adrenal glands are part of the Hormone circuit, and they produce your body’s primary anti-stress hormone, cortisol.
Cortisol is responsible for things like maintaining your heart and blood vessels, regulating blood pressure and blood sugar levels, suppressing your immune system and neutralizing inflammation. When you have low stomach acid, pathogens and undigested food pass through to your GI tract and create inflammation as they are not supposed to be there. In turn, your adrenal glands secrete cortisol in order to help with the inflammation and stress.
Symptoms of AFS include fatigue, insomnia, easily gaining weight and difficulty losing it, hair loss, brittle nails, hypoglycemia, food and drug sensitivities, GI tract issues, anxiety, mild depression, salt and sugar cravings, PMS, low libido, infertility, lowered immunity, and brain fog.
The Inflammation circuit of your NEM is composed of the gut, microbiome, and immune cells. Inflammation is a natural and necessary part of immunity, helping to rid your body of the original insult that damaged the cells as well as the dead and damaged cells themselves. It relies heavily on a smooth Detoxification circuit and a healthy gut and microbiome.
So how does having reduced stomach acid trigger inflammation?
The immune system is responsible for defending your body against any foreign invaders - substances that spread to parts of the body they shouldn’t be in. As we’ve seen, low stomach acid allows undigested or partially undigested food to pass through the stomach and enter the rest of the digestive tract. Bacteria and viruses that enter the stomach also have a higher chance of surviving, since the hydrochloric acid (HCl) there is not strong enough to kill them off.
The rest of the digestive tract doesn’t have that acid to help it defend itself. Likewise, it can’t break down food as well as HCl can. So it is vulnerable to the damage that the undigested food and pathogens that enter it can cause. As bacteria and viruses build up in the gut, they begin to create an imbalance in the gut’s microbiome, a condition called dysbiosis. In essence, the “bad bacteria” begin to overwhelm the “good bacteria.” The undigested food particles can also ferment and feed the bad bacteria, worsening the dysbiosis.
Dysbiosis has far-reaching consequences, and one of them is a leaky gut. As leaks form in the gut’s lining, they allow particles to enter the bloodstream that shouldn’t be there. This triggers an immune response, with immune cells rushing to the area to fight off these foreign invaders so they do not spread through the bloodstream to other parts of the body.
 When the immune system launches an attack, inflammation is the result. And although inflammation is indeed necessary to help get rid of the pathogens and dead cells, if it becomes chronic, which is what happens when a leaky gut is not addressed promptly, it forms the basis of many challenging health issues. This is a slow creeping problem that people don’t notice until it is too late. And eating inflammatory foods such as sugar, dairy products, and processed foods can make it worse.
When the immune system launches an attack, inflammation is the result. And although inflammation is indeed necessary to help get rid of the pathogens and dead cells, if it becomes chronic, which is what happens when a leaky gut is not addressed promptly, it forms the basis of many challenging health issues. This is a slow creeping problem that people don’t notice until it is too late. And eating inflammatory foods such as sugar, dairy products, and processed foods can make it worse.
And that’s exactly what can happen when low stomach acid is left untreated. The dysbiosis and leaky gut continue, causing an immune response and inflammation every time you eat. Inflammation that spreads from the gut to the joints will cause joint pain; inflammation that spreads from the gut to the central nervous system will cause anxiety, depression, and brain fog; and systemic inflammation left untreated is at the root of autoimmunity.
The interesting thing is that the relationship between low stomach acid and inflammation goes both ways. Inflammation can also cause hypochlorhydria because it increases the levels of stress hormones in the body. And actually, stress is a common link between inflammation and hypochlorhydria.
Acute stress is something your body can adapt to through its “fight or flight” response. Your NEM is flexible enough to deal with stress and then return to homeostasis in order to allow your body to enter the “rest and digest” state. And that’s the key: the return to the “rest and digest” state is what gives your GI tract a chance to digest food.
But if stress becomes chronic, and your “fight or flight” response is frequently or constantly switched on, digestion takes a back seat, just like many other important bodily functions. That’s why with AFS, where your energy levels are so low your body goes into energy conservation mode, there is a slowing down in many organs and systems.
For example, AFS energy conservation leads to a decrease in reproductive functions, an increase in food and drug sensitivities because the Detoxification circuit slows down, frequent colds and flu because the immune system is weaker, and a general slowing down of physical and cognitive functions.
You need strong adrenal glands to be able to handle stress, and also to tackle inflammation. You also need to manage stress and inflammation in order to give the adrenal glands a break. And one way to do that is to fix any issues with low stomach acid.
It’s important to note at this point that over half the worldwide population has or has had H. pylori bacterial infections, and those are a major cause for a decrease in stomach acid. Unfortunately, this will require antibiotic treatment, which puts the microbiome at risk for further imbalance, since antibiotics affect the gut flora.
 But if that’s your situation, don’t worry, because there are ways to support your gut and microbiome in rebalancing after antibiotics. You can take prebiotic and probiotic supplements and eat fermented foods such as kimchi, sauerkraut, kefir, and organic yogurt. And you can reduce the consumption of things that harm your microbiome, such as eating sugar and drinking alcohol.
But if that’s your situation, don’t worry, because there are ways to support your gut and microbiome in rebalancing after antibiotics. You can take prebiotic and probiotic supplements and eat fermented foods such as kimchi, sauerkraut, kefir, and organic yogurt. And you can reduce the consumption of things that harm your microbiome, such as eating sugar and drinking alcohol.
If you don’t have H. pylori, eating a healthy diet that includes probiotic-rich foods is still a good idea. And if you have AFS, you should be following the adrenal fatigue diet. Because it is an anti-inflammatory diet, it will help reduce any inflammation and dysbiosis in the gut.
Other than H. pylori infections, antibiotics, inflammation, and stress, there are several risk factors and underlying causes you should be aware of. Those include zinc deficiency, taking antacids, being over 65 years of age, and stomach surgery.
Zinc deficiency is actually quite common, and if you eat a vegan diet you should pay special attention to getting enough zinc. Also, if you have malabsorption or you don’t eat a healthy diet in general, you may also need to deliberately add zinc-rich foods to your diet. These include oysters, pumpkin seeds, veal liver, lamb, roasted beef, chicken, roasted cashews, cacao, tahini, almonds, Alaskan king crab, and pork shoulder. Taking a zinc supplement for a while until you configure your diet can also be useful.
Prolonged use of medications that block stomach acid production, such as proton pump inhibitors and H2 blockers, are another cause of hypochlorhydria. Unfortunately, because many of the symptoms of low stomach acid mimic those of high stomach acid, and because some antacids are very easy to get over the counter, many people mistakenly take them when they are actually lacking in stomach acid. This, of course, makes things worse.
The good news is that you can address this issue without these medications by making some diet and lifestyle changes.
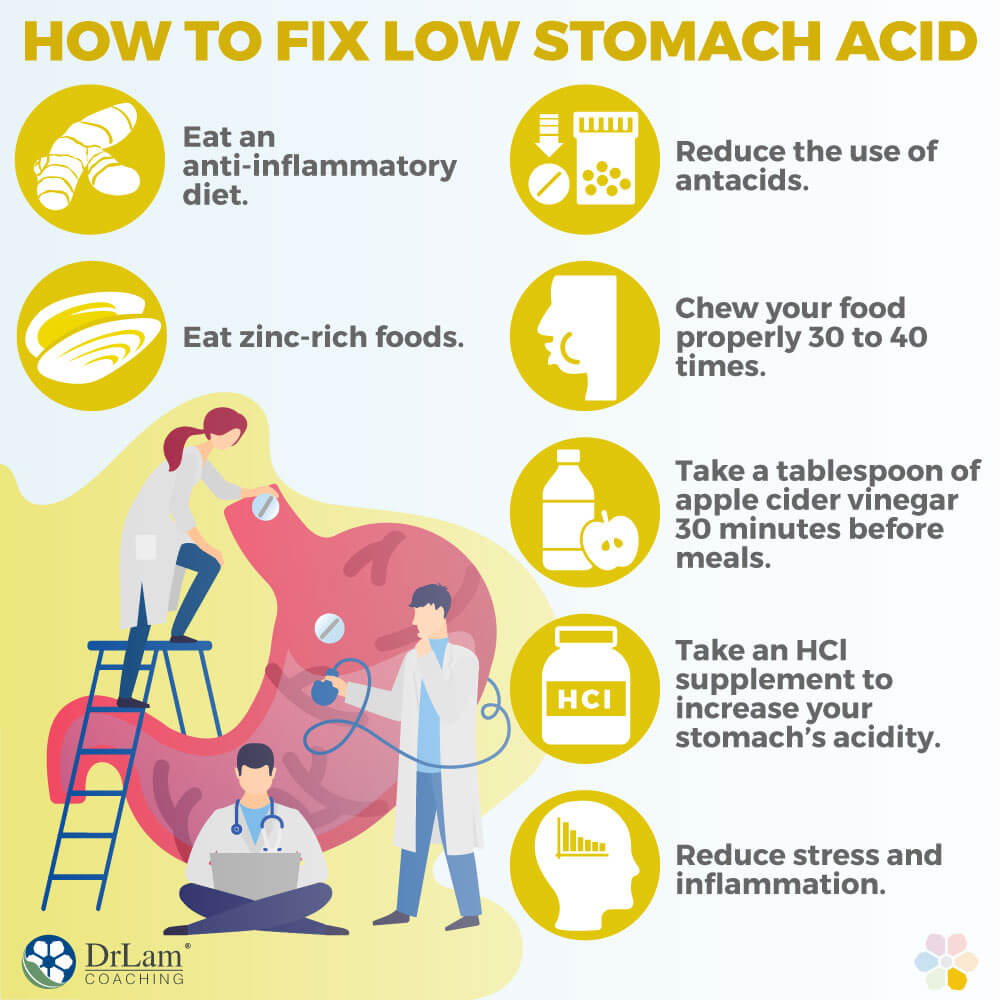
We’ve already covered many tips, such as eating an anti-inflammatory diet, eating zinc-rich foods, and reducing the use of antacids. But first, you should make sure you go to a doctor and rule out H. pylori infection, as that needs specific treatment.
There are a few other tips that can really help, and all of them are natural and easy to implement.
The first tip is to make sure you are chewing your food properly, about 30 to 40 times. There are enzymes in your saliva that help break down the food before it even enters the stomach, taking some of the workload off of it.
Speaking of enzymes, it can really help is to take digestive enzymes once or twice a day before your heaviest meals. Digestive enzymes are naturally made by different organs, such as the pancreas and stomach, which secrete them in order to help break down food. Proteases break down proteins, lipases break down fats, and amylases break down carbohydrates. But for many with digestive issues, taking a digestive enzyme supplement can really help with digestion and symptom relief. A few digestive enzymes to try are: Diazyme, Adrezyme and Stomazyme. You won’t have to take them forever, only until your digestion has regained its strength, and you have adopted a diet that contains enough raw fruits and vegetables, which contain digestive enzymes of their own.
 Next, you can take a tablespoon of apple cider vinegar about 30 minutes before meals to enhance stomach acid production. You can dilute it in a few tablespoons of water. Make sure you get raw, organic apple cider vinegar that is unfiltered so it still contains “the mother”. Although it does have a strong smell and taste, you will get used to it, and you may only need to use it for one to three months. Some people add a little honey to make apple cider vinegar “lemonade”.
Next, you can take a tablespoon of apple cider vinegar about 30 minutes before meals to enhance stomach acid production. You can dilute it in a few tablespoons of water. Make sure you get raw, organic apple cider vinegar that is unfiltered so it still contains “the mother”. Although it does have a strong smell and taste, you will get used to it, and you may only need to use it for one to three months. Some people add a little honey to make apple cider vinegar “lemonade”.
Finally, you can try taking an HCl supplement so that you increase your stomach’s acidity. However, taking supplements while you have AFS can be a little risky if you don’t know what you’re doing. Depending on how advanced your adrenal fatigue is, you may end up experiencing paradoxical reactions and supplement sensitivity. That’s why we strongly advise you to follow the guidance of an experienced medical professional. The same goes for those over 65 or who have had stomach surgery.
One thing to remember, however, is that all of these supplements and remedies are only temporary aids. Changing your diet and lifestyle are the tools for a permanent fix. You need to eat healthily, reduce stress and inflammation, allow your body to relax and recover, and adjust your medications so they do not affect your stomach acid production. These are all foundations that you must build in order to have lasting relief from low stomach acid.
© Copyright 2020 Michael Lam, M.D. All Rights Reserved.
Low stomach acid is a common condition that many have without knowing it. And some even confuse it with stomach acidity and end up taking the wrong treatment for it. And unless you address the root causes, such as inflammation and stress, you will be at risk for serious health conditions.
