 Healthy stomach bacteria– not many people think about these organisms in a positive way. Most think right away of something that invades your body and makes you sick. Immediately, the majority of people get a picture of bacteria causing stomach aches, nausea, and vomiting. Something to be killed by antibiotics. The truth is, healthy stomach bacteria actually keeps you healthy and slows down the aging process.
Healthy stomach bacteria– not many people think about these organisms in a positive way. Most think right away of something that invades your body and makes you sick. Immediately, the majority of people get a picture of bacteria causing stomach aches, nausea, and vomiting. Something to be killed by antibiotics. The truth is, healthy stomach bacteria actually keeps you healthy and slows down the aging process.
Bacteria gets into your body from whatever you eat or put in your mouth. And this process starts literally at birth. During the trek from womb to physical birth, you travel through the birth canal and pick up many of your initial stomach bacteria from your mother. You get both harmful and healthy stomach bacteria on this trip.
The more researchers study the bacteria in your stomach, the more the evidence stacks up that your stomach bacteria, along with the bacteria that populate your gut microbiota, strongly affect how you feel both physically and emotionally.
One of the ways bacteria in your stomach affect you physically is the connection between your gastrointestinal (GI) system and your immune system. Researchers suggest a great deal of your immune system is in your gut system. Others say up to 90 percent of diseases originate in your gut. This makes healthy stomach bacteria even more important.
Not only are healthy stomach bacteria vital in keeping you well, they also help you deal with illness conditions. This article will discuss both of these factors.
A human body contains over 10,000 microbes — or more than ten times the number of human cells! The genome of the microbiome, as an entity, is 100 times larger than the human genome, implying that the majority of genetic material inside your body is not actually yours, but the microbes’. These microbes include viruses, fungi, and bacteria that use the body as a habitat to form a balanced ecosystem. This ecosystem is called the microbiome, which is found in and on the bodies of humans and living things—in the mouth, on the skin, inside the gut. The human microbiome includes both harmful and beneficial organisms. The balance is shifting constantly and can affect the human host’s health. For the most part, the bacteria found in your body are valuable to your health and well-being and play a vital role in your survival. These bacteria are not only depended on for survival, they assist in the daily functions of digestion, vitamin creation, and protection against infections, as well as in a plethora of other roles. This article primarily deals with the gut flora, those microorganisms that live in the digestive tract.
AFS is a significant health condition that occurs when your adrenal glands, located on the tops of your kidneys, become depleted and unable to secrete cortisol, the hormone that helps your body handle the effects of stress. This health condition comes when stress attacks your body.
 Regardless of the origin of the stress, your body reacts the same way. An automatic response pathway is set in motion, beginning with the hypothalamic-pituitary-adrenal (HPA) axis. Various hormones and other chemicals begin the cascade of responses that end with your adrenals secreting cortisol to fight the effects of stress. Unfortunately, in this stress-filled world we inhabit, stress continues, overwhelming your system as your adrenals are depleted.
Regardless of the origin of the stress, your body reacts the same way. An automatic response pathway is set in motion, beginning with the hypothalamic-pituitary-adrenal (HPA) axis. Various hormones and other chemicals begin the cascade of responses that end with your adrenals secreting cortisol to fight the effects of stress. Unfortunately, in this stress-filled world we inhabit, stress continues, overwhelming your system as your adrenals are depleted.
AFS presents with a long list of physical and emotional symptoms, including insomnia, weight gain around your middle, lack of energy, inability to think clearly, feeling tired even after a good night’s sleep, depression, and poor memory. These symptoms and a lot of serious physical conditions can be triggered by stress resulting from not so healthy stomach bacteria and the changes they can bring due to inflammation and suppression of your immune system.
Because of the multitude of symptoms and their sometimes vague nature, physicians can have a difficult time making an accurate assessment of your condition. This leads to potentially ineffective remediation of your illness.
One reason physicians may have such trouble determining the root cause of your illness is due to their way of viewing the expression and remediation of disease. Most traditionally trained physicians look at your presentation of symptoms from an organ-specific viewpoint. This limits their choice of ways to handle your illness. In addition, many physicians are specialists and their outlook is limited to their specialty area.
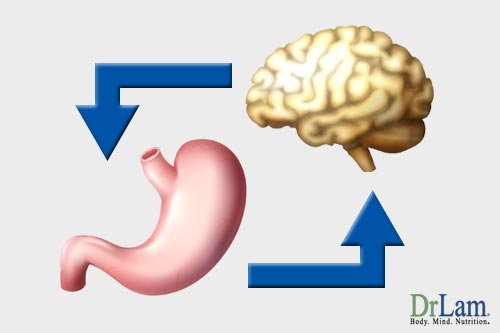
The NeuroEndoMetabolic (NEM) stress response is the body’s system of dealing with stress. There are six major components or circuits, each comprised of various organs and systems programmed to act on specific, targeted anti-stress responses. These components work synergistically to ensure that your body is well taken care of in the face of stressful situations. With regard to your stomach bacteria, the metabolic, immune, and hormone systems are the first to be affected. As your body reacts to the stress of unhealthy bacteria and their effects on inflammation, the other systems also begin to suffer. The neuroaffective and inflammatory responses are two circuits within NEM stress response that significantly alter mood, immune function, and cognition. These circuits involve three intricately interconnected components—the gut, brain, and microbiome—forming what is called the gut-brain axis. What happens to one component will affect the others. The neuroaffective circuit is made up of the autonomic nervous system, central nervous system, and gut. The inflammatory response circuit is composed of the gut, microbiome, and immune system. As you can see, the gut and its microbes are important to both circuits and link the two. Your body’s reaction to stress can lead to increased inflammation, just as an unhealthy gut biome will. Researchers have shown inflammation to be a factor in illness conditions as varied as depression, Parkinson’s disease, Alzheimer’s disease, and even autism. In order to most successfully deal with the symptoms of AFS and any symptoms of unhealthy stomach bacteria, your health professional should consider how all systems of your body interact as in the NEM model. The brain and gut seem so different and so far apart, so how does the connection work? Let’s take a look.
 Gut flora influence various brain functions, affecting your thoughts, emotions, and memory. Three quarters of the body’s neurotransmitters are actually made in the gut. That is why the signals that go between the brain and the gastrointestinal (GI) tract are vital to establishing and maintaining homeostasis, immune health, and hormonal levels. This connection is regulated by the central nervous system and the enteric nervous system. When there is a disturbance in either of these systems, it affects your ability to respond to stress and influences your overall behavior. As can be seen in those with inflammatory bowel disorder (IBD) and irritable bowel disorder (IBS), there is a strong correlation between anxiety and gastrointestinal disorders that demonstrates the significance of the connection axis between the brain and GI tract.
Gut flora influence various brain functions, affecting your thoughts, emotions, and memory. Three quarters of the body’s neurotransmitters are actually made in the gut. That is why the signals that go between the brain and the gastrointestinal (GI) tract are vital to establishing and maintaining homeostasis, immune health, and hormonal levels. This connection is regulated by the central nervous system and the enteric nervous system. When there is a disturbance in either of these systems, it affects your ability to respond to stress and influences your overall behavior. As can be seen in those with inflammatory bowel disorder (IBD) and irritable bowel disorder (IBS), there is a strong correlation between anxiety and gastrointestinal disorders that demonstrates the significance of the connection axis between the brain and GI tract.
There is also mounting evidence suggesting that the enteric microbiome (in the intestines) affects gut-brain communication, hence the naming of the microbiome-gut-brain axis.
An unbalanced collection of gut flora (dysbiosis), combined with stress, could lead to damage the gastrointestinal lining and increase the permeability of the blood-brain barrier. Thus, an unbalanced population of gut flora and healthy stomach bacteria can contribute to the inflammation of the whole body in addition to affecting the neuron signaling from the gut to the brain.
There is a wealth of evidence that demonstrates complex interactions between host and microbe. There are three particularly important methods by which the microbes in your gut interact with the brain: directly, via the vagus nerve and a network of nerves that wrap around the gut and transfer signals to the brain; through the circulation of primed immune cells that exist in the gut and move towards the brain; and through metabolite molecules, produced by gut microbes, that enter first the bloodstream and then the brain and eventually affect behavior. These metabolites have been shown to cause abnormalities associated with anxiety and autism when injected into healthy functioning mice. This could lend further support to the possibility of microbial molecules connecting the brain, gut, and neuroaffective circuit of the NEM stress response system.
That there is a complex interconnectedness among your gut system, your brain, and your immune system has been shown through research over and over. However, how they are interconnected and how they communicate is not as clear.
A tremendous amount of research has taken place recently providing information about how healthy stomach bacteria (that are a part of your gut microbiome) are crucial not only to your immune system, but also to the way your genetic makeup is expressed, to body health, to memory, to mental health, and to making you less susceptible to serious illness like cancer.
Some of this research has explored how communication happens between your two brains, the one in your head and the one in your enteric nervous system (ENS) that is embedded in the wall of your gut. This ENS is the part of you gives you that “gut feeling” when something is about to happen or isn’t right. It developed as the original nervous system in our distant ancestors and is made up of 500 million neurons. Scientists suggest it has so many because food can be dangerous.
 There is some research evidence that suggests your enteric nervous system and your brain develop from the same embryonic tissue.
There is some research evidence that suggests your enteric nervous system and your brain develop from the same embryonic tissue.
With the gut’s job of keeping out foreign “invaders” in the form of bacteria, there must be plenty of neurons to determine good from bad foods. In the case of ingesting bad food, this ENS signals your other brain to induce either diarrhea or vomiting to rid the body of the bad food.
How does it do this? About 90 percent of the communication between your gut brain and your head brain goes along the vagus nerve. Since vagus is Latin for wandering, this is a nerve that literally wanders through your body connecting many organs. The communication between your two brains is bidirectional. Information flows both ways between your brains.
This communication travels in the form of cytokines produced in your gut. They are intimately involved in cell communication having to do with immune functioning and inflammation. They are like hormones and serve the function of signaling cells where to go when an inflammatory response occurs.
Cytokines may travel from your gut to your brain and stimulate microglia, the immune cells in the brain, to produce neurochemicals. Some of these neurochemicals affect your mitochondria in a negative way, decreasing energy production and impacting the feedback loop that controls hormones, including cortisol.
This is just one way the unhealthy and healthy stomach bacteria in your gut system have far-reaching effects. They affect and have significant control over your entire bodily health.
The vagus nerve communication appears to be so important that researchers have found stimulation of this nerve to have a calming effect on the autonomic nervous system. When the vagus nerve is surgically cut (a vagotomy), the opposite effect occurs. When the vagus nerve is intact, it works to reduce inflammation and restore homeostasis.
Some research suggests pathogens can travel along the vagal pathway as well and, over a period of time, may give rise to an increased risk of Parkinson’s disease. On the other hand, full truncal vagotomy appears to decrease this risk. This finding highlights the importance of this vagal communication pathway between your ENS and your brain.
A significant number of researchers have found stress to have a strong effect on your health. The activation of the HPA axis begins a cascade of responses to stress that clearly have an impact in your stomach and gut.
Scientists are convinced your gut bacteria are continually influenced by lifestyle choices, diet, and environment. It’s nearly impossible today to stay away from stressors in the environment. Some of these stress producers come from choices you make, some come from toxins in the environment, and some are the result of poor diets filled with fast foods.
 Stress from any source can lead to increased inflammation and decreased immune functioning. Inflammation wreaks havoc on your healthy stomach bacteria and your gut system. When your gut is thrown out of balance (dysbiosis), your body is opened up to all kinds of illness conditions.
Stress from any source can lead to increased inflammation and decreased immune functioning. Inflammation wreaks havoc on your healthy stomach bacteria and your gut system. When your gut is thrown out of balance (dysbiosis), your body is opened up to all kinds of illness conditions.
With increased inflammation, the healthy stomach bacteria begin dying off from increased toxins in your system and those that aren’t as healthy seem to thrive. This can lead to a condition known as “leaky gut” where those toxins actually penetrate your gut lining and travel throughout your body.
Not only do these toxins prime your body for significant health problems, your stomach and gut are no longer able to extract sufficient nutrients from the food you eat to energize your body. These systems and the bacteria that live there also contribute to fat storage. When the balance of bacteria in your stomach and gut is disturbed, changes in body fat can also take place.
One study showed germ-free mice to gain weight and increase fat storage without increasing food intake when injected with gut bacteria from overweight mice. Apparently, the receiving mice’s gut system stimulated the production of hormones like insulin and increased fat storage, leading them to gain significant weight. The apparent stress of getting “foreign” bacteria led to this weight gain.
 There is currently no perfect standard for a healthy stomach bacteria. Due to environmental and genetic considerations, there are considerable differences in people’s “normal” gut flora. Generally, microbes that are healthy and diverse help to promote gut health and to maintain metabolic, structural, and signaling functionality. However, the gut can become imbalanced in a variety of ways; in particular, the term dysbiosis involves a change away from the normal diversity and stability found in the healthy stomach bacteria. This presents with an unstable gut that is unable to function normally and may eventually lead or contribute to neurological, metabolic, or autoimmune disorders. Causes of dysbiosis include environmental toxins, alcohol intake, excess stress, and overgrowth of yeast and bacteria.
There is currently no perfect standard for a healthy stomach bacteria. Due to environmental and genetic considerations, there are considerable differences in people’s “normal” gut flora. Generally, microbes that are healthy and diverse help to promote gut health and to maintain metabolic, structural, and signaling functionality. However, the gut can become imbalanced in a variety of ways; in particular, the term dysbiosis involves a change away from the normal diversity and stability found in the healthy stomach bacteria. This presents with an unstable gut that is unable to function normally and may eventually lead or contribute to neurological, metabolic, or autoimmune disorders. Causes of dysbiosis include environmental toxins, alcohol intake, excess stress, and overgrowth of yeast and bacteria.
For those with Adrenal Fatigue, high stress levels can often lead to dysbiosis. In addition, since your body is in a low energy state, the gut (and other bodily functions) often slows down in an effort to conserve energy. As your gut slows down, food stays in your stomach longer, resulting in reduced assimilation, longer transit times, and increased inflammation, as allergens have more time to seep into the body through the gut. If the food stays in the gut for a prolonged period of time, it can even start to rot in the stomach, releasing toxic compounds into the stomach. This may be another cause for gut dysbiosis.
When the mucosal lining of the gut fails in its role as a barrier to protect against potentially damaging molecules that can enter the blood flow, the resulting condition is known as leaky gut. Lipopolysaccharides on the outer membrane of gram-negative bacteria can then be found entering the bloodstream, prompting an inflammatory response. Inflammation influences the brain in several ways and is thought to be a major contributing factor to depression. In fact, selective serotonin reuptake inhibitors (SSRIs)—one of the main classes of drugs used in depression treatment—has been found to reduce inflammation in the brain. This anti-inflammatory effect may be an important part of why the drugs are effective. Thus, it is easy to see how your gut can have a major affect on the neuroaffective circuit and your mood simply through an elevation or reduction of inflammation.
Increased permeability of the intestinal lining can also lead to food allergies, malabsorption, and toxic overload. There is a saying that a leaky gut leads to a leaky brain, as the buildup of toxins can cause changes in mood, depression, fatigue, poor memory, confusion, and anxiety.
Unfortunately, the details of these connections are difficult to study because every individual’s gut microbiome is unique, and the terms healthy and unhealthy are in reference to an individual’s specific state of normality.
 Disturbances in the gut — such as an alteration in the composition of healthy stomach bacteria have been linked to neurological disorders such as multiple sclerosis (MS), Parkinson’s disease, and autism spectrum disorders. A Parkinson’s patient’s first symptom is usually constipation; the second is often the loss of taste and smell. These gastrointestinal disturbances are present long before the symptoms of motor neuron dysfunction, such as tremors or a shuffling gait, appear.
Disturbances in the gut — such as an alteration in the composition of healthy stomach bacteria have been linked to neurological disorders such as multiple sclerosis (MS), Parkinson’s disease, and autism spectrum disorders. A Parkinson’s patient’s first symptom is usually constipation; the second is often the loss of taste and smell. These gastrointestinal disturbances are present long before the symptoms of motor neuron dysfunction, such as tremors or a shuffling gait, appear.
Multiple environmental risk factors for neurological conditions have been found to promote an immuno-inflammatory response. In particular, improper folding and aggregation of proteins within the brain is a possible etiology for several neurodegenerative disorders. This could be caused by inflammation in the gut triggering inflammatory effects in the brain that cause misfolding of proteins and degeneration of neural cells.
Gut dysbiosis, healthy stomach bacteria, and inflammation have also been linked to autoimmune disorders. Western nations present with higher rates of multiple sclerosis and also tend to share similar dietary habits. These diets are thought to cause inflammation and disruptions in the optimal functioning of gut microbes. Patients with Parkinson’s disease and MS both have increased numbers of antibodies to a variety of antigens and lipopolysaccharides due to a more permeable intestinal lining. Taken together, the evidence indicates that a dysregulated inflammatory response circuit can be the result of prolonged stress, among other factors.
Alzheimer’s disease and general cognitive decline are marked by changes in the brain, disruptions in immune function, and increasing oxidative stress. These factors are all shaped by diet and gut flora in animal experimental models. One important link involves a neurotrophin, a type of protein that is responsible for the protection and the encouragement of healthy neurons. The production of this neurotrophin is dependent on the gut bacteria, and declines in individuals with Alzheimer’s. Changes to the microbiome occur with age and can be linked to neurodegeneration.
Among the disease states that can be brought on by an imbalance of healthy to unhealthy stomach and gut bacteria are two that seem to be increasing in frequency in our country. Research appears to suggest the huge role of inflammation in both Parkinson’s disease (PD) and Alzheimer’s disease (AD). With inflammation originating in your stomach and gut system with dysbiosis, the connection between bacteria imbalance and these serious illness conditions seems strong.
Some promising research conducted with fecal transplants has suggested improvement in PD symptoms as well as in chronic fatigue conditions. A decade of this type of intervention for patients with Clostridium difficile to alleviate constipation has also led to beneficial changes in patients with PD and chronic fatigue.
 Evidence is surfacing that points to AD as being closely related to a possible Type 3 diabetes condition. A significant increase in the research literature suggests insulin deficiency and insulin resistance, both found in AFS as well, to be present in the neurodegeneration that comes with AD. There appears to be a definite connection between large disturbances in brain insulin and insulin-like growth factor and the progressive abnormalities and lesions seen in AD. This Type 3 diabetic condition posed as a factor in AD appears to be selective for brain involvement only and seems to overlap with both Type 1 diabetes mellitus and Type 2 diabetes.
Evidence is surfacing that points to AD as being closely related to a possible Type 3 diabetes condition. A significant increase in the research literature suggests insulin deficiency and insulin resistance, both found in AFS as well, to be present in the neurodegeneration that comes with AD. There appears to be a definite connection between large disturbances in brain insulin and insulin-like growth factor and the progressive abnormalities and lesions seen in AD. This Type 3 diabetic condition posed as a factor in AD appears to be selective for brain involvement only and seems to overlap with both Type 1 diabetes mellitus and Type 2 diabetes.
Currently, one in 68 children born in the U.S. has a condition somewhere along the autism spectrum. This very serious condition affects multiple systems in the body. Prior to the last 10 years, autism spectrum disorder (ASD) was viewed as a neurological disorder primarily. But research now indicates these children suffer from numerous abnormalities in the endocrine, GI, immune, and detox systems among others. The various biological systems involved in ASD have not been clearly delineated. If all of these systems could be shown to be interrelated as in the NEM stress response, new avenues of successful remediation could be initiated.
Interestingly, a few studies have shown oxidative stress to play a role in the pathophysiology of ASD. However, not a lot of scientific attention has been directed at this aspect of the causes ASD. This increased oxidative stress in the brains of ASD children may be connected to chronic inflammation and DNA damage.
A relatively new direction for research into causative factors in ASD shows the use of acetaminophen to possibly be a factor in the development of ASD. Lately, there has been a lot of discussion regarding vaccinations leading to autism symptoms. This trend in thinking started at exactly the same time physicians began giving children acetaminophen rather than aspirin for the fevers associated with vaccinations.
Physicians thought acetaminophen was safer than aspirin for this purpose. But acetaminophen has a high incidence of immune system problems as well as metabolic issues. These metabolic issues include liver failure.
The link between acetaminophen and ASD lies in the fact that acetaminophen also depletes glutathione levels. Especially in children and infants. Glutathione is necessary for your body to have sufficient levels of antioxidants and for good brain function.
Young children can develop toxic overload with depleted glutathione levels. The current thinking among some scientists is the build-up of toxins can trigger changes in the brains of children who are genetically susceptible to autism.
 This high load of toxins can occur when a person has taken acetaminophen over a period of several days. Like with children who either have or may develop fever associated with vaccinations. Well-meaning pediatricians may recommend parents give their children acetaminophen for several days prior to vaccinations as a preventative against fevers.
This high load of toxins can occur when a person has taken acetaminophen over a period of several days. Like with children who either have or may develop fever associated with vaccinations. Well-meaning pediatricians may recommend parents give their children acetaminophen for several days prior to vaccinations as a preventative against fevers.
Mothers’ stress during pregnancy may also be implicated in development of ASD. The hypothesis is when mothers undergo stress while pregnant their stomach and healthy stomach bacteria changes. Their healthy stomach and gut bacteria are replaced by unhealthy bacteria. The byproducts of unhealthy bacteria have been shown to cause impaired brain development in the fetus. Animal studies have shown offspring to have ASD-like symptoms when their mothers experienced stress during pregnancy. Some researchers hypothesize one pathway from mothers’ stress to their babies’ brains may be through healthy stomach bacteria and the gut microbiome.
Stress during pregnancy leads to changes in the mothers’ vaginal regions. During the passage through the birth canal, their babies gut biome is affected significantly by these changes. These changes then lead to long-term developmental problems.
Researchers also suggest that some types of gut bacteria present in children with ASD produce waste products that appear to affect brain activity.
While many bacteria in the stomach and gut are healthy stomach bacteria, carrying out their processes of digestion, protecting the body against harmful bacteria, and producing vitamins, there are those bacteria that are harmful. If the harmful bacteria are not reduced and controlled, they begin producing metabolites that are detrimental to the gut and the brain.
Previous studies have shown children with ASD to have abnormal colonies of digestive bacteria in their stomachs and gut systems. Studies have also linked these bacteria with the more severe symptoms of ASD.
Other studies suggest microbes in the gut may change levels of neurotransmitter-related metabolites leading to altered brain function. This indicates significant cross-talk between the gut systems of children with ASD and their brains.
The connection between the gut and mental health has garnered increasing attention in recent years. Various psychological disorders, especially depression, may actually be disorders of inflammation, with the gut being a crucial mediator. Several animal studies have demonstrated that transplantation of microbes from anxious or depressed mice to germ-free mice could induce the same behaviors in the previously healthy mice.
Anxiety and depression are also common symptoms of Adrenal Fatigue. It is therefore vital for those suffering from Adrenal Fatigue Syndrome to keep the microbiome healthy. This will help to restore balance to the neuroaffective circuit, calming the body down and enabling a speedier recovery.
One issue that occurs when there is dysbiosis in your stomach and gut is oxidative stress. Oxidative stress occurs when free radicals are released into your system and the system can’t repair the damage they cause or detoxify your body and rid it of these free radicals.
 In conditions of dysbiosis, your metabolism, hormone, and immune systems are hampered significantly in their efforts to detox your body. Enzymes needed by the liver to carry out the detox process are lowered in dysbiosis.
In conditions of dysbiosis, your metabolism, hormone, and immune systems are hampered significantly in their efforts to detox your body. Enzymes needed by the liver to carry out the detox process are lowered in dysbiosis.
Research is beginning to show the role played by oxidative stress, inflammation, and lack of immune response in psychiatric conditions. The brain, where psychiatric behaviors begin, is particularly susceptible to oxidative stress. Any causative role of oxidative stress in psychiatric disorders isn’t clear as yet.
One factor that is clearer is that psychiatric disorders, especially depression in its various types, are highly influenced by inflammation. Inflammation is common in AFS and is brought on by an imbalance in healthy stomach bacteria and unhealthy stomach and gut bacteria.
Major depression is one of the more common forms of depression. Research shows the close relationship between increased inflammation and major depression. Possibly this relationship has to do with elevations in proinflammatory cytokines that have been found in patients with major depression. This elevation continues even after the depressive episode has been remediated and may predict future episodes of major depression. Antidepressants will lower levels of proinflammatory cytokines in major depression. Research of this nature helps with understanding of how nonsteroidalantiinflammatory (NSAID) drugs interfere with antidepressants.
These proinflammatory cytokines, which are the type of “messenger” chemicals used by the ENS to communicate via the vagus nerve, also bring on what is called “sickness behavior” as a normal response. This behavior adds to recovery from trauma and infection by conserving energy. It has been connected to depression due to the similarities in symptoms such as anhedonia, anorexia, anxiety, and cognitive symptoms.
The relationship between sickness behavior and depression appears to be one of two sides to the response to proinflammatory cytokines. The sickness behavior side is more positive, leading to recovery of your body from trauma and infection. The depressive side leads to lifelong problems with neuroinflammation and neurodegeneration.
These cytokines appear to start a cascade of reactions resulting in lowered serotonin levels and increased glutamatergic actions that lead to an increase in depressive symptoms.
Research has shown depression to be present when several illnesses brought on by inflammation are present. Inflammatory biomarkers are found whenever a person is experiencing major depressive disorder. Depression risk increases in the presence of immunomodulating agents. Stress activates proinflammatory pathways; antidepressants decrease inflammation. When inflammation is decreased, depression symptoms improve.
Since inflammation is increased with a decrease in healthy stomach bacteria, it is very important for people with depressive disorders, either present or past, to maintain healthy stomach and gut bacteria. Considering the interactive nature of all body systems, improving the neuroaffective system will lead to improvement in other systems.
 Everyone ages. But not everyone ages at the same rate. As people age, they are more likely to develop chronic illnesses of one kind or another. With these conditions, recovery in advanced age takes longer. The higher incidence of these kinds of illnesses and more difficulty in recovering is problematic for older people. And many of the illnesses contracted by older people have in common a high incidence of immune system suppression.
Everyone ages. But not everyone ages at the same rate. As people age, they are more likely to develop chronic illnesses of one kind or another. With these conditions, recovery in advanced age takes longer. The higher incidence of these kinds of illnesses and more difficulty in recovering is problematic for older people. And many of the illnesses contracted by older people have in common a high incidence of immune system suppression.
The term immunosenescence has been coined to describe the loss of immune function in these older people. If these elderly have adrenal fatigue, their immune system is already compromised. Aging will increase the loss of immune function in this condition.
The elderly also have increased incidence of Alzheimer’s and Parkinson’s diseases. Studies have shown a clear connection between these two conditions and the stomach and gut system. A commonality between these illnesses and the gut system lies in their contact and susceptibility to environmental issues.
Changes in healthy stomach bacteria of older people also play a role in aging. An animal study using groups of mice in youth, middle age, and old age showed changes in healthy stomach bacteria of the old mice. The old mice had sufficient bacteria in their microbiomes to break down simple sugars, but insufficient bacteria to handle complex sugars, as well as lactate. The importance of this has to do with increased lactose in the stool being connected to development of ulcerative colitis and other inflammatory bowel diseases in elderly people.
The old mice in this study also showed a lack of bacteria that produce vitamins B12 and B7. Lower levels of B7 have been shown to be connected to colon cancer. In addition, the old mice contained bacteria that would break down creatinine. Creatinine builds muscle, so the lack of it would appear to explain at least some of the loss of muscle so common in the elderly.
 Evidence continues to grow regarding the beneficial effects of healthy stomach bacteria. And it has become very clear how unhealthy bacteria in this part of your body has a tremendous impact on your overall health.
Evidence continues to grow regarding the beneficial effects of healthy stomach bacteria. And it has become very clear how unhealthy bacteria in this part of your body has a tremendous impact on your overall health.
That makes it imperative for you to put into your life those food products and other strategies for building or repairing your stomach and gut bacteria. Taking charge of your diet and lifestyle choices will enable you to improve your health status considerably. Your stomach and gut bacteria are significantly influenced by the foods you eat and the choices you make about how you live your life.
In those with psychiatric or neurological conditions, it is difficult to determine which came first, the disorder or the unhealthy gut. Dysbiosis of the gut could account for both, but so could stress. It is also important to consider the environmental risk factors—such as an unhealthy diet and lifestyle—that may upset healthy stomach bacteria, gut flora, and the brain. Promote healthy stomach bacteria with a microbiome diet.
It is clear that neurological/neurodegenerative and psychiatric disorders share similar causes and symptomatology, as well as a common underlying pathophysiology of an unhealthy gut that influences numerous intersecting pathways on the microbiome-gut-brain axis. However, it is difficult to determine the function of these individual systems separately. The entire microbiome-gut-brain axis is therefore still poorly understood. For brain conditions, the gut could prove to be the missing piece of the puzzle, providing new understanding of the etiology in ways that might support the introduction of new public health and clinical interventions.
The composition of the gut microbiome is quite resilient and adaptable. The key factors that are essential to its stability and diversity are all components of lifestyle. Several strategies for healthy stomach bacteria, and in turn brain health, are given below.
Some of the foods and other substances you ingest that have the most significant negative impact on your healthy stomach bacteria include the following:
These simple sugars tend to raise blood sugar levels significantly, pushing your pancreas to release more insulin to control them. In people with AFS, insulin levels are already unbalanced and depleted; insulin resistance is a major issue with this condition. Consuming these refined sugars (and there is a tendency to crave sugars with AFS) will only lead to more significant problems. Sugars fuel pathogenic yeasts and fungi in your gut.
Note: You must be certain to wash vegetables and fruits very well to remove as much of the residue from these chemicals as possible.
 Ingesting these medications may help in some cases of infections, but the use of antibiotics seems to be reaching epic proportions. They are exactly what their name implies: killers of bacteria. All bacteria. There is no antibiotic that can differentiate beneficial bacteria from harmful ones. Overuse of antibiotics simply kills off the healthy stomach bacteria. When you have AFS, you already have problems with your gut flora. Don’t add to them by taking an overabundance of antibiotics.
Ingesting these medications may help in some cases of infections, but the use of antibiotics seems to be reaching epic proportions. They are exactly what their name implies: killers of bacteria. All bacteria. There is no antibiotic that can differentiate beneficial bacteria from harmful ones. Overuse of antibiotics simply kills off the healthy stomach bacteria. When you have AFS, you already have problems with your gut flora. Don’t add to them by taking an overabundance of antibiotics.
These medications damage cell membranes and inhibit energy production by mitochondria.
Make changes in your lifestyle to reduce or eliminate as much stress as possible. Already, you understand the impact stress has on your life, often leading to adrenal failure and its detrimental symptoms. Stress also impacts the healthy stomach bacteria that keep you working at your best.
Knowing the types of foods to avoid is the first step toward healthy stomach bacteria again. Stay away from processed foods, farm-raised animal products that contain antibiotics and growth hormones, sugars, and gluten products.
Diet plays an important part in determining the amount of each type of bacteria and the phylogenetic diversity of gut flora. A healthy diet of vegetables, fruits, and a variety of whole grains, will help the population of Bacteroidetes. Bacteroidetes are particularly useful in the production of short chain fatty acids (SCFAs), which assist in the regulation of gut inflammation. Large amounts of SCFAs tend to decrease intestinal pH and prevent growth of some pathogenic bacteria such as E.coli and Enterobacteriaceae. SCFAs also help curb appetite; they attach to the receptors in the gut and regulate the hormones for appetite control. Thus, the microbiome and its production of SCFAs may play important roles in dietary intake, rate of fat deposition, utilization of fat, insulin resistance, and diabetic inflammation. Vegan and vegetarian diets also increase phylogenetic diversity of the gut flora compared to diets that include meat.
Body weight in mice can be affected by the transplantation of microbes in the cecum (the beginning of the large intestine). In one study, genetically obese mice had significantly less Bacteroidetes and more Firmicutes relative to their lean counterparts; but in another, when the gut microbes of a lean mouse that had undergone gastric bypass surgery were transferred to germ-free mice, those mice experienced weight and fat loss. These studies showed that dietary patterns that favorably alter the gut microbiome—specifically those that emphasize plant-based foods—might have significant benefits to human health and confer greater resilience and adaptability to change.
There are three food components that are largely thought to promote gut health:
Probiotics, living microorganisms that can be found in consumer goods such as yogurt and kimchi,
 Non-digestible carbohydrates, such as fiber commonly found in vegetables, whole grains, and fruits,
Non-digestible carbohydrates, such as fiber commonly found in vegetables, whole grains, and fruits,
Secondary plant metabolites, especially flavonoids found in red wine and brightly colored fruits.
Individuals who adopt what’s known as the Standard American Diet (SAD) experience fewer benefits of plant foods, while simultaneously provoking disruptions of other metabolic functions by eating large quantities of processed sugar and fat. These two aspects of the SAD both contribute to the development of gut inflammation and dysbiosis.
Prebiotics fibers that are not digestible by your gut enzymes. They are usually fermented in the GI tract by bacteria and selectively stimulate certain intestinal flora and metabolic activities. Probiotics are foods that contain helpful microbes that are able to survive stomach acid and bile; they enter the intestines and adhere to the lining, growing and establishing temporary residence in the intestines.
There is evidence to suggest that prebiotic and probiotic supplements and fermented foods are beneficial for the gut. The digestion of fermented fibers has natural anti-inflammatory effects. Fermentation of food makes it more digestible, turning polyphenols into an active state. It also produces more vitamins, enzymes, and amino acids while breaking down phytates, tannins, and oxalic acid. An additional benefit of fermented food is, of course, the lengthened shelf life.
Since 90% of neurotransmitters are made in the gut, it makes sense that gastrointestinal conditions can influence mood and behavior. Irritable Bowel Syndrome (IBS) is found in 10-20% of adults in the US, and they have much higher rates of anxiety and depression than the background population. Studies have shown that probiotics are beneficial in the treatment of both the GI symptoms and anxiety and depression, in those affected. There is mounting clinical evidence for probiotics reducing stress and anxiety responses, as well as for improving the general mood of IBS patients who suffer from chronic fatigue. Studies have assessed the effect of a mixture of Bifidobacterium longum and Lactobacillus helveticus on human subjects and rats showing that anxiety was reduced . Although the mechanism of action is still to be determined, some probiotics seem to lower inflammation, decrease stress from oxidation, and improve general nutrition.
Specific probiotic strains can assist in the modulation of various facets of the microbiome-gut-brain axis. However, it is important to note that these effects vary from organism to organism and individual to individual. Nevertheless, the data strongly suggests that probiotic strains have great potential to bolster the gut flora and thus regulate behavior and the brain.
Probiotics and prebiotics are a good first choice. Significant research shows adding these supplemental foods to your diet increases the good bacteria you need. Do what your mother always told you:

Especially green vegetables. These foods break down in your system, giving your healthy stomach bacteria the nutrients they need to thrive. So eat your carrots, broccoli, spinach, onions, and peas, among others.
Grapes contain resveratrol and flavonoids that will feed not only your gut but also your brain. Apples, blackberries, blueberries, and cherries are also good for you.
They are beneficial and higher in Omega 3 fatty acids than farm-raised fish or chicken. And you don’t have to worry about added antibiotics or other substances that you don’t want in your body.
Co-enzyme Q10, selenium, antioxidants like vitamins C, D, and E and Omega 3 fish oil are good for your stomach and gut system. Dietary supplementation of this kind will enable your stomach and gut bacteria to grow.
There are other enzymes that can be added as supplements or through foods you eat. These enzymes all have significant beneficial effects on healthy stomach and gut bacteria and in digesting foods.
Probiotics are especially important for rebuilding healthy stomach bacteria. Foods that are probiotic in nature build up your healthy stomach bacteria in your gut microbiome. These fermented foods increase the nutrient and phytochemical value of the foods. Consuming probiotic foods will improve your brain health. Probiotics that contain 20-50 billion live organisms per dose and have combinations of Lactobacillus and Bifidobacteria are best.
These foods should be taken with meals once or twice a day. At this time, the field of study of probiotics is in its infancy, but more and more studies are being conducted on a regular basis. From this will come more science-based probiotics available for consumer use. Gas and bloating may be the common side effects of probiotics. Uncommon side effects include overstimulation of the immune system.
Digestion begins when food enters your mouth. Salivary amylase begins breaking down larger polysaccharides into smaller disaccharide molecules like maltose and dextrin. Farther into your gut, pancreatic amylase further breaks these starches into monosaccharides like glucose. It’s also involved in anti-inflammatory reactions. If you’re low in amylase, you have an increased risk for abscesses since amylase also digests dead white blood cells or pus. One form of this enzyme, beta-amylase is contained in some plant seeds, bacteria, and yeasts. Amylase is the enzyme that furnishes energy for the body to use. If you have low levels of amylase, both diabetes and metabolic syndrome are possible. Side effects may include abdominal cramps, diarrhea, and nausea. Severe abdominal cramps or painful urination are uncommon and may need attention from your healthcare provider.
 Released mostly by the pancreas, lipase aids in digesting and absorbing fats. With low levels of lipase, there may be associated high levels of cholesterol and fat in the blood. Sufficient levels of lipase enable your body to absorb vitamins and minerals appropriately. If you have gallbladder issues, a supplement with lipase may help. High doses of lipase supplement may lead to nausea and stomach upset. Some digestive enzymes can destroy lipase.
Released mostly by the pancreas, lipase aids in digesting and absorbing fats. With low levels of lipase, there may be associated high levels of cholesterol and fat in the blood. Sufficient levels of lipase enable your body to absorb vitamins and minerals appropriately. If you have gallbladder issues, a supplement with lipase may help. High doses of lipase supplement may lead to nausea and stomach upset. Some digestive enzymes can destroy lipase.
Fats must have extra digestion before being absorbed because their end products are carried through the body in a water medium in which fats are not soluble. Lipase is one of those enzymes that aids in this process. Mild side effects such as nausea, cramping, and diarrhea may occur. If you’re pregnant or breastfeeding, it’s best to avoid lipase.
Lactase is an enzyme that aids in digesting lactose. Many people have too little lactase and thus can’t digest lactose. This may lead to a lack of calcium if people can’t digest dairy products. Stomach cramps, diarrhea, and gas may also result from lactose intolerance. Milk is a good source of nutrients for people.
Being able to digest and utilize this source of nutrition is very important. This enzyme is produced by fungi and bacteria. Lactase reactions take place along the tissue walls of the small intestine. Lactase is most prevalent during infancy when milk is the main nutrient. After weaning, lactase becomes less available until in adulthood, some people have so little they become lactose intolerant. There are very few side effects of lactase. Rarely, severe allergic reactions may occur. If this happens, consult your physician immediately.
The major function of this digestive enzyme is to break down proteins. In this digestive process, amino acids needed by the body are released as protease breaks the peptide bonds in proteins. Protease has benefits in immune regulation and inflammation. A lack of protease possibly leads to calcium deficient conditions because protein bound calcium requires protein to be carried around the body in the blood.
One source of glucose for the body is the conversion of protein. With a lack of protease, there is an increased risk of hypoglycemia. Protease is also an aid to breaking down toxins in the blood, thereby aiding the immune system. Possible side effects of protease include diarrhea, constipation, headache, dizziness, nausea, and vomiting. If any of these become severe, your healthcare professional should be consulted immediately.
Pepsin requires a strongly acidic environment in which to break down protein into peptides. It’s produced in the stomach lining. It’s one of three enzymes that break down protein, the other two being chymotrypsin and trypsin. In the stomach, it breaks down protein into polypeptides. It works to sever links between some types of amino acids and helps break protein into amino acids and peptides which can then be absorbed by the intestinal lining. Pepsin also stimulates the liver to produce bile that helps the body get rid of toxins and plays a role in the production of antibodies and collagen.
 Papain is a digestive enzyme extracted from papaya fruit and involved in breaking down tough to digest proteins. It breaks down larger protein molecules into smaller molecules or amino acids. It does this by cutting the bonds on the interior protein chains in a process called endopeptidase or by cutting bonds on the ends of protein chains (exopeptidase). By doing either of these processes, papain increases the absorption of the nutrients in proteins. Additionally, papain works as an antioxidant, supports the immune system and healthy stomach bacteria.
Papain is a digestive enzyme extracted from papaya fruit and involved in breaking down tough to digest proteins. It breaks down larger protein molecules into smaller molecules or amino acids. It does this by cutting the bonds on the interior protein chains in a process called endopeptidase or by cutting bonds on the ends of protein chains (exopeptidase). By doing either of these processes, papain increases the absorption of the nutrients in proteins. Additionally, papain works as an antioxidant, supports the immune system and healthy stomach bacteria.
It may have use as an alternative to other chemicals in increasing the survival of probiotic bacteria in yogurt. There is little research into the long-term effects of papain. Some irritation of the stomach and throat have been reported. Pregnant and breastfeeding women should avoid papain.
A mixture of enzymes, bromelain is found in pineapples. It may have some effect on inflammation from infections. It’s a protein digesting enzyme with many other possible health benefits. It enables the body to absorb nutrients, especially from protein, more effectively and is exceptionally effective at healing gastrointestinal ailments. It has also been shown to have some benefit in treating sinus infections and various joint pains.
Eating the core, not just the fruit, of pineapples will supply this enzyme. It’s best to let the pineapple ripen a little more than typical so the core is softer. If taken to improve digestion, bromelain is best taken with meals. Due to its anti-clotting properties, consult your healthcare professional before taking a supplement if you’re on blood-thinning medications.
A flavonoid antioxidant, quercetin is found in foods like leafy greens, tomatoes, and broccoli. It fights free radical damage, aging, and inflammation. It has strong effects on immunity and inflammation and is one of the most diffused nature-derived flavonols. It lessens the effects of oxidative stress on the body, thus decreasing the effects of this stress on the aging process. As an anti-inflammatory, it has a beneficial effect on chronic fatigue. It also supports heart health through its anti-inflammatory properties.
Adding apples, peppers, and cherries to your diet will increase the amount of quercetin in your system. In reasonable levels, there appear to be no side effects of quercetin. In very high levels, there may be headaches and tingling of the extremities. It may interact with antibiotics, chemotherapy, and blood thinners. For this reason, and if you’re pregnant or breastfeeding, consult your healthcare professional before taking supplements.
Exercise may diversify the gut flora. Athletes had increased bacterial diversity in the gut and fewer indications of inflammation compared to non-athletes. Researchers found that individuals who participated in moderate exercise more than 30 times a month presented with escalated levels of brain-derived neurotrophic factor (BDNF), compared to individuals who either didn’t exercise at all or exercised at an extreme level. BDNF promotes anti-inflammatory pathways and leads to the promotion of both brain and healthy stomach bacteria.
 The above strategies will work well for most healthy people. You should be more cautious, however, if you suffer from certain conditions such as:
The above strategies will work well for most healthy people. You should be more cautious, however, if you suffer from certain conditions such as:
If you have Small Intestine Bacterial Overgrowth (SIBO) or a systemic infection, such as Lyme Disease and Candida, fermented foods or supplements may actually makes the overgrowth worse, leading to bloating, flatulence, and pain.
If you have Inflammatory Bowel Disease (IBD), enzymes supplements may trigger inflammation in certain people.
If you have Irritable Bowel Syndrome (IBS), excessive exercise can trigger constipation and fatigue.
Excessive enzyme supplementation may lead to diarrhea. The proper blend of digestive pancreatic enzymes should be considered for the clinical setting.
Excessive probiotics may lead to constipation. The largest number of beneficial bacteria is not always the best. In fact, it can often lead to brain fog, bloating, fatigue, and anxiety. The primary focus should be finding the proper amount to match the body’s ability to assimilate the metabolites and promote healthy stomach bacteria.
Excessive fermented food in a body that is already congested can lead to brain fog, anxiety, and depression.
Co-enzyme Q10 can lead to insomnia if you’re taking 100 mg or more per day. At 300 mg per day, an increase in liver enzymes has been reported. Rashes, nausea, dizziness, and fatigue have been also reported in some people. If you suffer from AFS, you may see an increase in those symptoms you already deal with if you take this supplement.
Selenium can have significant side effects when taking high doses or for long-term use. An increased risk of developing diabetes has been shown when long-term use is involved. Nausea, vomiting, loss of energy, and irritability have been reported. Lightheadedness and tremor are possible side effects, as well. Selenium can stimulate the immune system and may increase the risk of autoimmune diseases, in theory. Hypothyroidism can be made worse with selenium unless you take iodine along with it.
Vitamin C may cause diarrhea initially, but this should go away with continued use. However, vitamin C also increases the absorption of iron, so caution should be taken if you are also taking iron supplements.
Vitamin E has blood thinning qualities, so it may interfere with any other blood thinning medications you may be taking. Of greater concern is the fact that vitamin E may enhance your body’s sensitivity to your own insulin if you’re an adult with adult onset diabetes. Other studies have shown vitamin E to increase blood pressure in people with diabetes.
The weaker your health is, the more careful planning you will need to use with these rebalancing strategies due to other conditions that are often preexisting, such as liver congestion, extracellular matrix pollution, receptor site damages, and hypersensitivities. This includes most Adrenal Fatigue, chronic fatigue, and those struggling with advancing cancer. Always consult a knowledgeable and experienced healthcare professional, because the wrong approach can worsen your condition quickly.
 Since the microbiome plays a major role in the gut-brain connection, gut flora can be used to alter the neuroaffective and inflammatory circuits of the NEM stress response system. The connections are so complex and numerous that much more research needs to be done to explore these mechanisms and individual variations. In the meantime, however, consider using prebiotics or probiotics in your recovery plan to promote healthy stomach bacteria and mental health.
Since the microbiome plays a major role in the gut-brain connection, gut flora can be used to alter the neuroaffective and inflammatory circuits of the NEM stress response system. The connections are so complex and numerous that much more research needs to be done to explore these mechanisms and individual variations. In the meantime, however, consider using prebiotics or probiotics in your recovery plan to promote healthy stomach bacteria and mental health.