 Functional dyspepsia is a condition where you experience symptoms of discomfort in the upper digestive tract even though there are no structural problems there. The symptoms need to be present for a month or longer, and can include:
Functional dyspepsia is a condition where you experience symptoms of discomfort in the upper digestive tract even though there are no structural problems there. The symptoms need to be present for a month or longer, and can include:
Because these symptoms can be present with other conditions, functional dyspepsia is sometimes misidentified. It is commonly confused with Irritable Bowel Syndrome (IBS), Peptic Ulcer Disease, Gastroesophageal Reflux Disease (GERD), Gastroparesis, and cancers of the upper abdomen.
In about 20-30% of people with dyspepsia, another condition is found to be the cause of the symptoms. And in many cases, dyspepsia occurs concomitantly with other conditions. IBS, anxiety, depression, and a previous history of peptic ulcer disease, for example, are often found in people with dyspepsia.
Issues that can cause or worsen it include:
Chronic stress, whether psychological (from job pressure, for example) or physical (from recurring infections, for example), is also the main culprit in Adrenal Fatigue Syndrome (AFS). AFS, like functional dyspepsia, is also a collection of symptoms without a structural or clear organic cause.
Symptoms of adrenal fatigue include tiredness, easily gaining weight and difficulty losing it, insomnia, brain fog, loss of libido, PMS, infertility, hair loss, an inability to tolerate stress, anxiety, mild depression, and hypoglycemia, among others.
Stress causes your adrenal glands to secrete cortisol, your body’s main anti-stress hormone. And although cortisol is essential for important functions like regulating blood sugar and blood pressure, neutralizing inflammation, suppressing the immune system, and maintaining the heart and blood vessels, too much or too little of it wreaks havoc on the system.
 In the beginning stages of AFS, cortisol levels are on the rise, while in the more advanced stages, when your adrenal glands are exhausted, cortisol levels drop, leaving your body to battle stress without its most important stress-fighter.
In the beginning stages of AFS, cortisol levels are on the rise, while in the more advanced stages, when your adrenal glands are exhausted, cortisol levels drop, leaving your body to battle stress without its most important stress-fighter.
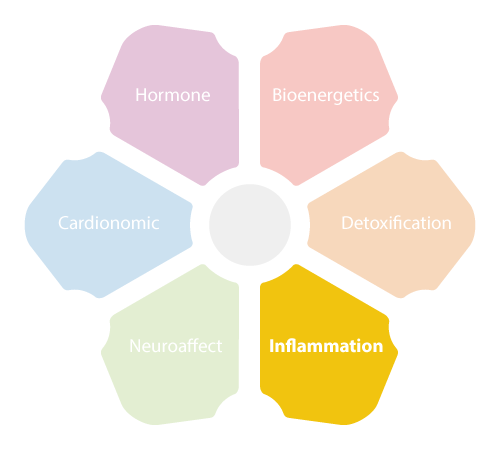
Adrenal fatigue will also affect your body’s entire NeuroEndoMetabolic (NEM) Stress Response, which is your body’s global response to stress. The NEM is composed of six circuits – the hormone, the bioenergetic, the cardionomic, the neuroaffect, the inflammation, and the detoxification circuits – all working together in sync. If one of these dysregulates, all the others are affected too.
Although it can be a little difficult to pinpoint the exact cause when dealing with dyspepsia, and though there are many different factors that can play a role in its onset and development, there are several links between it and adrenal fatigue that could help point the way to recovery.
First of all, as we’ve just seen, chronic stress is a culprit in both. But, it’s a little more complex than that. Chronic stress is also a cause of dysbiosis, an imbalance in the gut’s microbiome, which can create many problems within and without the gastrointestinal (GI) tract. Dysbiosis is a trigger for chronic inflammation – a very big stressor on the body and a cause of adrenal fatigue and functional dyspepsia.
When your gut’s microbiome is out of balance, the integrity of your gut’s lining can be compromised, creating small leaks that let toxins, pathogens, food particles, and other substances into your bloodstream that shouldn’t be there. Your immune system sees those as a threat and mounts an attack, creating a state of inflammation in your gut.
But because the leaks remain, this cycle continues and the inflammation becomes chronic, eventually spreading to other parts of the GI tract as well as the rest of the body. Inflammation that reaches your nervous system, for example, can create brain fog and mental health issues. Inflammation that reaches your joints can cause pain there. And inflammation that reaches your upper digestive tract can cause functional dyspepsia.
The inflammation circuit of the NEM, composed of the immune system, the gut, and the microbiome, is an essential part of your body’s stress response. Without inflammation, your body would not be able to fight off pathogens and get rid of dead or damaged cells and tissues. It is part and parcel of a healthy immune response. It is only when it gets out of control, or when it is suppressed completely, that you can get serious health problems.
Chronic inflammation will also make your adrenal glands work overtime to produce cortisol, as one of the functions of cortisol is to suppress the immune system and neutralize inflammation once the immune response is complete. But with chronic inflammation, there is a constant need for cortisol, and as such, there is an inevitable progression towards adrenal exhaustion if the cause of inflammation is not resolved.
One way to avoid that is to figure out what is creating dysbiosis in your microbiome and begin to take steps towards healing your gut. Some factors that are causing the dysbiosis may also be causing the dyspepsia and adrenal fatigue directly, so changing them can bring a lot of relief quickly. They include:
Inflammation in the gut may also be why you find those with dyspepsia and/or AFS also suffering from mental health issues, such as anxiety and depression. And, of course, having to deal with the symptoms of these two conditions significantly adds to mental distress. So it is always advisable to deal with the physical as well as psychological at the same time.
Reducing inflammation in the gut will have one of the biggest impacts on the health of your GI tract specifically, as well as your health generally. This is done by removing the causes of inflammation, sealing up the leaks that were created in the gut lining, and rebalancing your gut’s microbiome.
You begin with an elimination diet. This means you should cut out all possible allergenic foods and gut irritants, including sugar, alcohol, gluten, and dairy. Pay special attention to gluten, as it has been found to be a significant factor in many digestive disorders, including functional dyspepsia.
A screening done in 2018 of 200 patients with a GI tract disorder showed that around 4% of them had a food sensitivity, while a population-based study done in 2018 showed a strong link between wheat sensitivity and functional dyspepsia, even among those who did not have celiac disease, colorectal cancer, or inflammatory bowel disease (IBD).
This falls in line with the growing body of evidence pointing to gluten sensitivity as a major cause in gut inflammation and microbiome dysbiosis.
 Medication seems to be another big issue when dealing with dysbiosis and GI tract issues. Prolonged use of NSAIDs is implicated in the development of functional dyspepsia. So consult your doctor if you’ve been taking medications that have been affecting your digestion and gut health to see if you can wean off of them or find alternatives.
Medication seems to be another big issue when dealing with dysbiosis and GI tract issues. Prolonged use of NSAIDs is implicated in the development of functional dyspepsia. So consult your doctor if you’ve been taking medications that have been affecting your digestion and gut health to see if you can wean off of them or find alternatives.
This may be a little tricky in some cases. For example, since functional dyspepsia is caused by the Helicobacter pylori, the usual way to manage it is, of course, antibiotics. But antibiotics do affect the balance of the microbiome. What you can do, however, if you must take antibiotics, is make sure that you focus on rebuilding your microbiome afterward with gut-healing foods and probiotics, such as sauerkraut, kimchi, kefir, raw dairy, and bone broth.
Other medications your doctor may recommend include proton pump inhibitors that block acid, H2 receptor blockers that neutralize acid, prokinetic agents that strengthen the esophagus, medications that help with stomach emptying, and medications that help with gas relief. Again, it is up to you whether you decide to try these medications, but make sure you understand the side-effects, the exact reasons for the medication, interactions with anything else you are taking, and the length of time you will be taking it, so you can prepare yourself accordingly.
Diet is and should be your number one recovery tool, and it will give you the deepest and most sustainable results. If you’ve already eliminated allergenic foods, irritating medications, started to incorporate gut-healthy foods into your diet, do your best to eat as much of your food as whole and organic as possible, thereby reducing exposure to pesticides and artificial substances.
Taking up an adrenal fatigue diet can be very helpful for rebalancing the gut’s microbiome, strengthening the adrenals, and lowering inflammation all in one – thereby also helping with the dyspepsia. The adrenal fatigue diet is very anti-inflammatory, gentle on digestion, nutritionally dense, and timed so that your body is getting a constant supply of energy and nutrients while recovering.
Because with dyspepsia you might experience early satiation, you may not be eating enough, and so you’ll be losing weight, nutrients, and energy. You can remedy that by eating smaller meals more frequently throughout the day. This is actually also good for adrenal fatigue, since it’s important to keep blood sugar levels stable and get enough energy and nutrients to replenish the loss that comes with AFS. Try to not let more than three or four hours go between meals. Make sure you eat something as soon as you wake up.
You may want to avoid high-fat foods at first as they can slow down gastric emptying and cause discomfort. Caffeine, spicy food, and highly acidic foods, like tomatoes, should also be reduced or avoided, at least in the beginning until your health is robust again.
Since psychological stress can be a major factor in inflammation, AFS, and dyspepsia, finding ways to manage and reduce it is of paramount importance. Therapy, support groups, meditation, and taking time off are all options. If you are suffering from serious anxiety or depression, do not delay talking with your doctor about it.
Getting enough rest and sleep is one of the most important steps you can take to lower stress levels, strengthen your adrenals and improve general well being. With functional dyspepsia, sleeping with your head a little elevated may help with symptom relief as well.
And finally, do your best to improve your diet and lifestyle first before reaching for medication, so that the changes you make last and do not bring about harmful side-effects. Consider consulting with a health professional who is trained in nutrition, such as a functional medical doctor or holistic health practitioner.
 Be patient, and keep the long view. Although the symptoms of functional dyspepsia can be very uncomfortable, most people with GI tract issues fair very well with changes in diet and lifestyle, and barely ever need intervention with drugs. Supplements, here and there, do help but that’s as far as most people will need to go if they eat well and live a healthy lifestyle.
Be patient, and keep the long view. Although the symptoms of functional dyspepsia can be very uncomfortable, most people with GI tract issues fair very well with changes in diet and lifestyle, and barely ever need intervention with drugs. Supplements, here and there, do help but that’s as far as most people will need to go if they eat well and live a healthy lifestyle.
© Copyright 2019 Michael Lam, M.D. All Rights Reserved.
Functional dyspepsia is a common upper digestive tract condition that can be quite uncomfortable. The bloating, pain, burning, nausea, and inability to eat properly might make you reach for medications that have other side-effects. Here’s what to do about it instead.
