The term endotoxemia refers to a high concentration of toxins in your blood cells. In other words, a toxic overload in your cells. And the root cause of endotoxemia, and many other health conditions for that matter, lies in the gut.
 Optimal gut health—and indeed, your overall health—depends on microbial diversity, which helps to create a more resilient environment. The diverse microbial community in your intestines enables your body to deal with stressors more effectively, including opportunistic pathogens as well as stressors caused by diet. In most cases, poor health—for whatever reason—is linked to an altered gut microbiome.
Optimal gut health—and indeed, your overall health—depends on microbial diversity, which helps to create a more resilient environment. The diverse microbial community in your intestines enables your body to deal with stressors more effectively, including opportunistic pathogens as well as stressors caused by diet. In most cases, poor health—for whatever reason—is linked to an altered gut microbiome.
The diverse gut microbiome is established at birth and numerous factors can affect the health of this initial microbiota. Among these, the type of birth (natural childbirth versus cesarean delivery or C-section), whether a baby is breastfed or given formula, and if the pregnancy reached full-term or the baby was born premature.
For example, in natural childbirth, an infant receives their microbiota from their mother during the delivery. Although, the downside is that if a mother’s microbiome is unhealthy for whatever reason, the unhealthy bacteria is also passed along to the child. On the other hand, the microbiota of a baby born via C-section comes from bacteria found on the skin of the delivery doctor or nurse that brings the baby into the world. Therefore, a baby may miss out on bacteria that children born naturally inherit from the mother. Other factors that influence microbiome diversity at this early stage in life include environmental factors and whether the baby’s mother has taken antibiotics shortly before the birth.
A stable gut microbiome is usually established between the ages of two and four. But your microbiome is never static, and many factors can contribute to or detract from healthy gut flora.
Studies indicate that infants with reduced microbial diversity in their intestines may be at a higher risk of developing allergies and other sensitivities.
A higher percentage of body fat and inflammation are also associated with poor microbial diversity. Being overweight or obese not only affects the richness of your lower gut microbiome but may also put you at a higher risk of metabolic syndrome and associated health conditions, as well as its accompanying symptoms.
To a large extent, diet can help prevent this. For example, consuming foods high in fiber, such as fruits and vegetables, is known to increase gut microbiota diversity.
The above is supported by research linking diet to the composition of the gut microbiome populations, suggesting that changing your diet can permanently change your gut microbiome for the better. In other words, a healthy diet could provide you with a diverse composition of good gut microbes.
While many people think simply taking a probiotic can balance your gut microbiome, this is not necessarily true. In general, probiotics cannot ensure a large enough diversity of gut microbes which may be needed to address the root cause of your issue – either in the short or the long term.
Studies suggest short-term consumption of a high-fat diet, derived from either animals or plants, can strongly influence your gut flora, by modifying its composition. A high-fat diet may help certain microbes flourish and have a negative impact on others.
In one illuminating study, mice were initially placed on a low-fat, plant-based diet and then switched to a western-type diet mainly consisting of fats and sugars. After just one day on the new diet, the gut microbiomes of the mice had changed – and not for the better.
Artificial sweeteners may also have a detrimental effect on gut health. Non-caloric sweeteners are a dietary staple for many trying to lose weight or suffering from diabetes. But they have also been linked to metabolic abnormalities and imbalances in the gut microbiome, and even prediabetes.
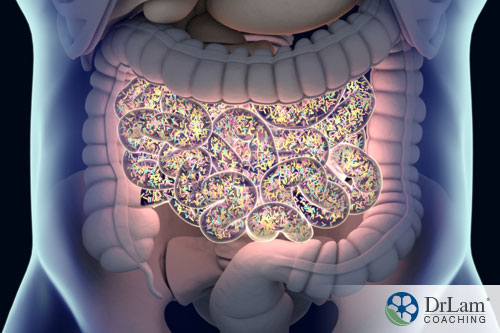
 Gut flora can be divided into two main groups: Firmicutes and Bacteroides. Together, these two bacterial phyla make up 99% of your gut bacteria. The ratio of Firmicutes to Bacteroides tends to decrease as you get older.
Gut flora can be divided into two main groups: Firmicutes and Bacteroides. Together, these two bacterial phyla make up 99% of your gut bacteria. The ratio of Firmicutes to Bacteroides tends to decrease as you get older.
Firmicutes are the main bacterial phylum in your gut microbiome and produce short-chain fatty acids. Thus, they are the main source of energy for the cells lining your colon and are produced from fiber as it ferments.
Bacteroides are mostly found in the lower part of your gastrointestinal (GI) tract and make up a significant portion of your feces. This type of bacteria plays an important role in sensing and adapting nutrients for use, getting rid of toxins, and helping the immune system control pathogens. Moreover, a compromised gut lining can lead to irritable bowel syndrome (IBS) or leaky gut syndrome. This allows members of the Bacteroides family to move through the gut lining and enter your bloodstream, potentially causing serious harm, i.e., metabolic endotoxemia.
If you are obese, consuming coffee can reduce your Firmicutes to Bacteroides ratio, and may also increase your body’s short-chain fatty acid stores while lowering branched-chain amino acid levels.
Branched-chain amino acids are derived from protein sources like legumes and meat. They support the transmission of information between neurons in the brain and throughout the body, stimulate muscle growth, and help reduce muscle breakdown, and are particularly important if you’re suffering from certain health conditions.
It’s not all bad news for coffee drinkers, though. Coffee and chocolate are rich in flavonoids, antioxidants that are also found in fruits and vegetables. Flavonoids help fight free radicals, may offer antimicrobial and mood-enhancing properties, and can provide antihistamine action.
Certain ‘good’ bacteria benefit from dark, unsweetened chocolate, and may produce anti-inflammatory compounds that help combat inflammation associated with metabolic endotoxemia.
Although there are some benefits, you should still be careful with your caffeine intake. Reducing your consumption or cutting caffeine out of your diet altogether may be of more benefit in the long run. This is especially true if you’re struggling with a leaky gut and/or Adrenal Fatigue.
Leaky gut syndrome and Adrenal Fatigue Syndrome (AFS) are closely related. Both conditions tend to feed off each other. Coffee can worsen the fatigue associated with Adrenal Fatigue and you may find yourself needing more and more coffee to get the same stimulatory effects day after day. But it’s important that you don’t suddenly quit drinking coffee. This can cause you to crash. Instead, it’s best to seek the guidance of a knowledgeable AFS specialist who can help guide you through your AFS recovery and find the appropriate time for you to give up coffee.
Inflammation is essentially the main cause of IBS. And many other health conditions are also the result of or have an element of inflammation, including cardiovascular diseases, diabetes, Alzheimer’s, celiac disease, fibromyalgia, asthma, and even autism, to name just a few. Yet inflammation is your body’s direct response to stress. The stress could be psychological, physiological, or environmental in nature, from the air you breathe to the food you eat.
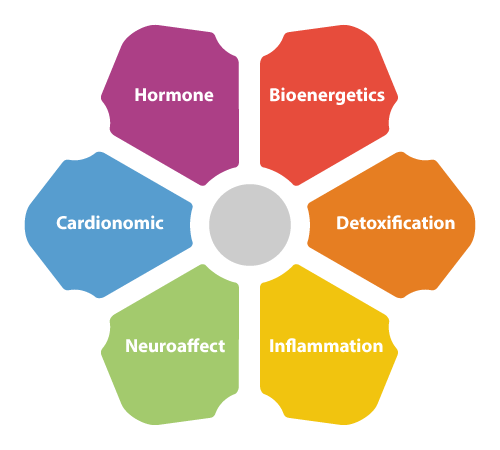 Whatever the stressor, your hypothalamus is where stress is first perceived. From here, chemical messengers are sent to the pituitary gland, which in turn sends its own set of chemical messengers to the adrenal glands to trigger the appropriate response. Collectively, these three crucial components of the body are referred to as the HPA axis. The response is usually the release of cortisol and adrenaline which trigger the fight-or-flight response. The entire process is part of the NeuroEndoMetabolic (NEM) Stress Response, a chain reaction that is activated by stress and impacts every part of the body. Once the stress has passed, everything in your body should go back to normal. However, prolonged stress constantly triggers the NEM Stress Response and therefore, can lead to potentially devastating consequences on your health.
Whatever the stressor, your hypothalamus is where stress is first perceived. From here, chemical messengers are sent to the pituitary gland, which in turn sends its own set of chemical messengers to the adrenal glands to trigger the appropriate response. Collectively, these three crucial components of the body are referred to as the HPA axis. The response is usually the release of cortisol and adrenaline which trigger the fight-or-flight response. The entire process is part of the NeuroEndoMetabolic (NEM) Stress Response, a chain reaction that is activated by stress and impacts every part of the body. Once the stress has passed, everything in your body should go back to normal. However, prolonged stress constantly triggers the NEM Stress Response and therefore, can lead to potentially devastating consequences on your health.
One of these consequences is inflammation. The NEM Stress Response triggers inflammatory processes to help your body fight off pathogens. Your inflammation circuit is comprised of the immune system, GI tract, and microbiome.
The lining of the GI tract lining is permeable, which allows certain nutrients to pass into your bloodstream. However, constant inflammation can widen the spaces between individual cells lining the GI tract, allowing foreign pathogens to pass through. This triggers your immune system and causes even more inflammation, resulting in a vicious cycle.
Your immune response and inflammation are linked to the adrenal glands, since the cortisol produced by the adrenals plays a significant role in the immune response. If you’re suffering from Adrenal Fatigue, your immune cells may be insensitive to the effects of cortisol, which could lead to—or may have already led to—chronic inflammation and numerous other health issues. One of them is IBS.
Both IBS and Adrenal Fatigue can be the root cause or trigger various autoimmune conditions. Interestingly, psychological stress is one of the major causes of IBS and endotoxemia.
Besides adrenal insufficiency, the causes of IBS include:
One potential consequence of IBS is toxic overload, when pathogens enter the bloodstream overburden your body. Severe toxic overload can lead to systemic diseases, such as metabolic endotoxemia.
Toxins from your GI tract can leak through the gut lining and enter your bloodstream, often as a result of IBS, and cause metabolic endotoxemia.
One common group of toxins are called lipopolysaccharides (LPS), which are derived from gram-negative bacteria like Bacteroides.
Metabolic endotoxemia is essentially an immune response that causes persistent, low-grade inflammation as a result of circulating toxins, mainly LPS.
 It is estimated that at least one-third of the people in Western countries have some degree of metabolic endotoxemia.
It is estimated that at least one-third of the people in Western countries have some degree of metabolic endotoxemia.
One of the characteristics of endotoxemia is an increase in LPS within five hours after eating a meal. High-calorie meals tend to have a much greater impact than low-fat meals with fewer calories. High LPS concentrations can exacerbate inflammation.
If you’re suffering from chronic metabolic endotoxemia, you may run the risk of developing one or more chronic conditions such as cardiovascular diseases, hypoglycemia, diabetes, mood disorders, and obesity. Other symptoms associated with endotoxemia include constipation, chronic pain, low testosterone levels, cancer, polycystic ovarian syndrome, autoimmune conditions, anxiety, depression, hypertension, Type 2 diabetes, sleeping disorders, Alzheimer’s, dementia, bipolar disorder, and even eating disorders. Note that the conditions and symptoms associated with endotoxemia are similar to those of Adrenal Fatigue.
The damage caused by LPS is due to the production of ‘bad’ cytokines that trigger a chronic inflammatory reaction.
Studies on endotoxemia in lean, overweight, and obese people provide some interesting insights into the condition.
The adverse effects of endotoxemia after a meal seem to be more prominent in obese, prediabetic, or diabetic people. Whereas, mildly overweight and lean people experienced fewer symptoms.
The findings suggest you may want to think twice about eating a high-fat diet if you are obese or suffering from diabetes. This may put more strain on your already compromised gut lining. Furthermore, if Adrenal Fatigue is one of your associated conditions, a high-fat diet could contribute to adrenal insufficiency. So, if you’re obese or diabetic, you should address your adrenal and gut health before adopting a high-fat diet.
People with endotoxemia often report feeling worse after a meal and get some relief from fasting.
A number of studies have attempted to establish a link between metabolic endotoxemia and obesity and/or diabetes. The conclusions of these studies strongly suggest:
The key takeaway from various studies is that microbial diversity in your gut may be beneficial, by increasing your body’s resilience and staving off health conditions.
Elevated LPS is one of the hallmarks of endotoxemia and is also linked to various other health conditions. And many of these conditions are also related to Adrenal Fatigue.

Most health conditions are the result of metabolic endotoxemia, which is a root cause of many conditions related to cardiovascular health, cancer, mood disorders, and autoimmune disease. All of these disorders can also be connected to the various stages of Adrenal Fatigue. Thus, it may safe to speculate that endotoxemia and Adrenal Fatigue are closely related, with each one feeding the other and vice versa.
The different health conditions mentioned above are all, essentially, symptoms of a greater underlying problem, endotoxemia – and to an even large extent, adrenal issues. Conventional health care approaches typically address health issues, such as asthma, chronic pain, or Alzheimer’s, individually without ever considering the root cause. However, the key to a successful recovery is to address the underlying issues at work while providing adrenal support. With most health issues, diet plays a major role.
However, with diet, you may need to change your way of thinking. This means cutting back on (or totally abstaining from) takeout, processed foods, and sugar. It also involves being mindful of what you eat and making better dietary choices.
Fat is necessary for metabolic health. But not all fats are equal. Saturated fats and trans fats are considered the bad guys; whereas monounsaturated fats, such as those found in olive oil, and polyunsaturated fats are healthy options. Monounsaturated fats can help reduce endotoxicity and improve heart health by lowering ‘bad’ cholesterol levels. Polyunsaturated fats, e.g., omega-3 and omega-6 fatty acids, can reduce triglyceride levels in your blood, slow down plaque buildup on the walls of your arteries, and help lower blood pressure. Omega-6 fatty acids may also reduce your risk of developing diabetes and lower blood pressure.
Good sources of omega-3 and omega-6 fatty acids include:

Another dietary essential for battling endotoxemia is to increase your intake of fresh organic fruits and vegetables. Most commercial farming practices use chemicals, fungicides, and herbicides that may still be on or in the fruit and vegetables you purchase. Then, when you ingest them, this adds to your toxic load. Organic fruits and vegetables are not exposed to these toxins.
In addition to providing the essential vitamins and minerals your body needs to function optimally, fruits and vegetables are also high in fiber and prebiotics. Prebiotics are dietary fibers found in food that feed gut-friendly bacteria. A diet rich in fiber may also help reduce insulin sensitivity in both lean and obese diabetics.
Common fiber-rich foods with a high prebiotic content include:
Quercetin has many benefit for the immune system. Since it inhibits LPS function, this natural flavonoid helps downregulate inflammatory responses and promotes cardiovascular health.
Foods rich in quercetin include leafy green vegetables, black tea, green tea, peppers, red onions, apples, grapes, and broccoli.
 Studies suggest exercise may actually change the composition of your gut microbiome. Research shows that those with a sedentary lifestyle experienced remarkable, positive changes in their gut microbiome following six weeks of exercise; most notably, increased production of short-chain fatty acids which can reduce your risk of inflammatory diseases, heart conditions, obesity, and even Type 2 diabetes. Exercise may also reduce insulin sensitivity and improve insulin signaling.
Studies suggest exercise may actually change the composition of your gut microbiome. Research shows that those with a sedentary lifestyle experienced remarkable, positive changes in their gut microbiome following six weeks of exercise; most notably, increased production of short-chain fatty acids which can reduce your risk of inflammatory diseases, heart conditions, obesity, and even Type 2 diabetes. Exercise may also reduce insulin sensitivity and improve insulin signaling.
As mentioned, conventional farming methods in the U.S. make extensive use of chemicals. One of these, glyphosate—a known carcinogen—is banned in Europe. Yet the chemical is still sprayed on wheat crops in the U.S. The herbicide may cause gut dysbiosis and play a role in the development of celiac disease. It weakens the tight junctions between the cells lining your gut and may alter your gut microbiome.
Glyphosate is also a component in mixed crop sprays. This may pose an even greater health threat because toxic reactions can occur when glyphosate is mixed with other chemicals.
If glyphosate is playing a role in your endotoxemia, you’ll need to get it out of your system by performing a detox. This can be done by:
Most people experience endotoxemia, regardless of age or dress size. While it can give rise to a myriad of health conditions, there are a number of things you can do to prevent it. And it all starts with taking care of yourself.
First, it’s necessary to address the IBS issue. This will require supporting your adrenal glands, addressing any stressors that are contributing to the condition, taking supplements, if needed, and making dietary changes.
Which brings us to the second point, diet. A rich and varied diet will supply your body with all the vitamins and minerals it needs to function at its best. At the same time, you should increase your fiber intake to help ensure good microbial diversity in your gut. This will allow your body to start the healing. You may also want to consider intermittent fasting.
Next, you could take supplements for extra support, such as fatty acids, vitamin C, and zinc. But before you start taking any new supplement, it’s best to speak with someone knowledgeable in the healthcare field. Depending on the cause of your endotoxemia and the current state of your adrenals, some supplements could end up doing more harm than good.
Finally, identify the psychological stressors affecting you and try to get rid of them. You may not be able to quit your stressful job, but you can do things that help you relax. For instance, take the dog for a walk, hang out with friends, read a book, do some yoga, or practice meditation.
If you’re suffering from AFS and digestive issues, such as a leaky gut, chronic constipation or diarrhea, or just loose stools, it’s important to address your gut as part of your AFS recovery. This essential step is often overlooked in Adrenal Fatigue recovery programs. Having a good microbiota and a healthy gut are imperative for a successful recovery. That’s why it’s so important to seek guidance from an Adrenal Fatigue specialist who can put you on the right path to recovery.
© Copyright 2020 Michael Lam, M.D. All Rights Reserved.
Surprisingly, yes! Endotoxemia and Adrenal Fatigue are related. Importantly, gut dysbiosis is one of the symptoms of Adrenal Fatigue. But unfortunately, the conditions tend to feed off each other, creating a continuous cycle that’s hard to break.
