 The benefits of ketamine, whether through its NMDA receptor blocking, or through the metabolites it creates in the body when it is broken down, are partly due to its ability to affect the neuroaffect circuit of the NEM. As stress accumulates, it begins to limit the brain’s functioning and overwhelms the brain and nervous system with excitatory signals. Certain areas of the brain are over-activated, and because the stress is constant, they don’t get enough “rest and repair” time.
The benefits of ketamine, whether through its NMDA receptor blocking, or through the metabolites it creates in the body when it is broken down, are partly due to its ability to affect the neuroaffect circuit of the NEM. As stress accumulates, it begins to limit the brain’s functioning and overwhelms the brain and nervous system with excitatory signals. Certain areas of the brain are over-activated, and because the stress is constant, they don’t get enough “rest and repair” time.
Some genetic vulnerabilities also make for a greater susceptibility to mental health issues, including depression, as well as for a NEM neuroaffect circuit that dysregulates more quickly and easily than in non-genetically prone individuals. These vulnerabilities can create deficiencies in the rest and repair neurotransmitters, or create a higher-than-normal level of excitatory ions in cell membranes.
And so therapy should be tailored accordingly. A therapy plan needs to consist of decreasing excitotoxicity (the neurotoxic activation of excitatory pathways), increasing the rest and repair time for the brain and nervous system by increasing the levels of the neurotransmitters responsible for it, and, of course, by eliminating or reducing the original stressor.
Glutamate is one of the brain’s main excitatory neurotransmitters, and the NMDA receptor is turned on when glutamate is secreted. These receptors become over-activated by the presence of too much glutamate, which then creates a state of excitotoxicity. One of the benefits of ketamine is that it can block these NMDA receptors, interrupting this excitotoxicity in a very short period of time.
Esketamine, which is used for anesthesia in nasal spray form across Europe, was given the title “breakthrough therapy” for the treatment of depression by the FDA in 2016. It has fewer side effects than ketamine and studies on its affinity for NMDA receptors and its antidepressant effects have been ongoing, with the most recent study published in April 2018.
In this study, patients with suicidal depression were given the first esketamine administration and then monitored for five days in an inpatient setting. Then, they were given it twice a week for four more weeks. They were also given the standard treatment for depression alongside this trial. In addition, there was also a placebo group.
The difference between those given esketamine and those given placeboes was significant. Those given placeboes had 68 suicide attempts and half of the group needed extra suicide prevention precautions during their inpatient time. However, these differences only lasted up until day 25, showing that although the benefits of ketamine can be very effective short-term, there is a need for long-term solutions.
That’s why more testing and trials should be done to see how the benefits of ketamine can become sustainable, and what kind of holistic therapy plans can be put in place during the period of its effectiveness, so once its effects begin to dissipate, the patient is not left without options.
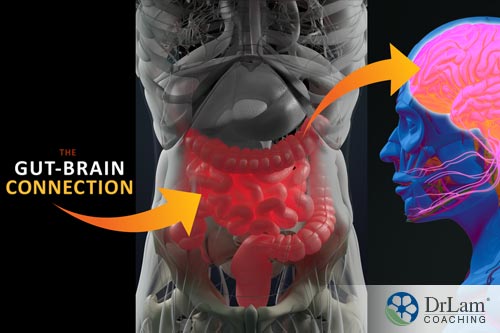 One of the body’s most important regulator pathways for your neurotransmitter pool is the microbiome-gut-brain axis. Disruption in this pathway, from chronic low-grade inflammation in the gut that is caused by cell-mediated immunity, can lead to depression.
One of the body’s most important regulator pathways for your neurotransmitter pool is the microbiome-gut-brain axis. Disruption in this pathway, from chronic low-grade inflammation in the gut that is caused by cell-mediated immunity, can lead to depression.
The gut contains two-thirds of your immune system cells, and an imbalance in gut flora, which is called dysbiosis, is one of the most common causes of inflammation in the gut. That’s because dysbiosis can leave the gut lining vulnerable to leaks. The gut lining is responsible for keeping harmful substances out of the bloodstream while letting in the nutrients that have been released by the process of digestion. The gut lining is made of epithelial cells that are tightly connected. When these connections are compromised, leaks begin to form, which then let substances such as toxins, food particles, and pathogens into the bloodstream.
When this happens, the immune system reacts immediately to eliminate these intruders. Part of the immune response is inflammation, and since the site of this process is the gut, inflammation begins and is mostly concentrated there. But the inflammation in the gut can actually travel to other areas of the body, such as the joints, causing pain there, or the brain and nervous system, causing anxiety, depression, insomnia, and brain fog.
If you have a food allergy, such as gluten intolerance, you probably know exactly what it feels like. You eat something with gluten, you feel bloated and achy, and a little while later, you start to get the brain fog, irritable mood, and other neurological symptoms.
 Inflammation affects the brain’s ability to respond to a stressor. One of the markers of inflammation that is prevalent in depression, as well as autism, Alzheimer’s disease, and Lou Gehrig’s disease, is called Lipopolysaccharide (LPS). LPS is a bacterial toxin that is usually housed in the gut, but with a leaky gut, infections, or high-fat meals, it can enter the bloodstream, where it becomes toxic and creates a lot of problems for the body and brain.
Inflammation affects the brain’s ability to respond to a stressor. One of the markers of inflammation that is prevalent in depression, as well as autism, Alzheimer’s disease, and Lou Gehrig’s disease, is called Lipopolysaccharide (LPS). LPS is a bacterial toxin that is usually housed in the gut, but with a leaky gut, infections, or high-fat meals, it can enter the bloodstream, where it becomes toxic and creates a lot of problems for the body and brain.
Because LPS is found on the outer membranes of gram-negative bacteria – the “bad” bacteria that begin to proliferate when there is a state of dysbiosis - it can be kept in check through the presence of gram-positive bacteria, or the “good” bacteria, by balancing the microbiome.
This is why one of the best things you can do for your brain, mood, and nervous system is to eat an anti-inflammatory diet that helps balance your microbiome and seal up any leaks in the gut. Actually, one of the reasons that SSRIs, which are the most commonly used antidepressant drugs, are effective is because they have strong anti-inflammatory capabilities.
Chronic inflammation is very common, and many medical health professionals view it as the primary cause of chronic diseases, but its early symptoms are sometimes too subtle to notice, and it is only when it becomes very disruptive is it given the attention it deserves. So, it is highly recommended that you adopt an anti-inflammatory diet if you have depression, even if you are not noticing other symptoms of inflammation.
Drugs can either have a positive or negative interaction with the inflammation response, while some can have a dual interaction, meaning they can be both anti-inflammatory and pro-inflammatory under different circumstances. Benefits of ketamine have been shown to have both, depending on the way it is used.
Because ketamine is sometimes abused as a recreational drug, it is taken without proper precautions, in the wrong doses, for the wrong duration, and sometimes on a consistent basis without regard for its negative effects. In one study, chronic ketamine administration of 60 mg/kg increased the levels of IL-6 and IL-1 Beta inflammatory cytokines, which signifies an increase in neuroinflammation. Neuroinflammation is indicated in neurodegenerative diseases.
On the other hand, some studies show that one of the benefits of ketamine, if taken correctly, is that it seems to have a positive influence on the regulation of inflammation at different levels – it affects cytokine production, recruitment of inflammatory cells, and the regulation of inflammatory mediators. It seems to be able to do this without blocking healing.
At this point, however, the reduction of inflammation as being one of the benefits of ketamine has not yet been studied enough. But with inflammation that begins in the gut, which is where most cases of inflammation begin, the focus should be about removing the causal factors of the inflammation and then working towards creating an anti-inflammatory state in the body, not about taking a drug to temporarily inhibit the spread of inflammation.
This should be done with diet and lifestyle changes, such as reducing stress, which is a causal factor in inflammation and AFS, eliminating any inflammatory foods from your diet, such as gluten and dairy, reducing or stopping the use of drugs and substances that create or exacerbate leaks in the gut lining, such as alcohol and antibiotics, and eating foods that help seal the leaks and reverse dysbiosis, such as bone broth and fermented vegetables.
 Ensuring your detoxification circuit is running smoothly is another very important puzzle piece in reducing inflammation and managing depression. A lot of times, especially if you’ve been in a state of low-grade inflammation for a long period of time, your system has accumulated a lot of toxins and metabolic byproducts that clog up your liver, extracellular matrix, and immune system.
Ensuring your detoxification circuit is running smoothly is another very important puzzle piece in reducing inflammation and managing depression. A lot of times, especially if you’ve been in a state of low-grade inflammation for a long period of time, your system has accumulated a lot of toxins and metabolic byproducts that clog up your liver, extracellular matrix, and immune system.
When your body’s detoxification burden is high, your body’s toxicity levels increase as well, and some of that toxicity can reach your brain and nervous system, which can cause or contribute to depression. Other symptoms of toxicity in the system include paradoxical reactions, intolerance to certain foods and drugs, and chemical sensitivity.
This can also make you resistant to certain therapies for depression, including the usual SSRIs, or aggravate the side effects of these medications. Many doctors who work with patients that suffer from treatment-resistant depression are now turning to ketamine as an option, making one of the benefits of ketamine its ability to work more quickly and effectively in some resistant cases.
And one of the ways it seems to work is through the metabolic byproducts it creates in the body, as mentioned above.
First of all, if you ever get suicidal thoughts, reach out for help as soon as possible. Ask if you have a plan for suicide. If the danger is immediate, as in you or someone you know is about to act on the suicidal thoughts, the first thing to do is call 911 or your local emergency number.
If you or someone you know is experiencing suicidal thoughts, but there is no immediate danger, then call your local suicide hotline. There are two numbers in the US that you can use:
Although the benefits of ketamine can be very handy in these cases, it’s not certain that your doctor or hospital will administer it, so ask about it as an option when you call or visit.
If you’re reading this, however, you’re most likely not experiencing suicidal ideation at this moment, but perhaps still a debilitating depression nonetheless. And even if you are on antidepressant medications and they seem to be working, you may feel you need an extra boost or a more natural alternative for the long run.
Thankfully, there are a lot of things you can do to improve your mood and mental/emotional health through diet, exercise, and lifestyle changes. If you have AFS, which is quite probable if you suffer from depression, as depression is a big stressor on the system, then strengthening your adrenal glands and balancing your NEM, especially your neuroaffect response, can help you a great deal.
With strong adrenal glands, your ability to handle stress and recover more quickly will increase. Cortisol levels will be more regulated, and the pressure will be taken off your nervous system to compensate. Adrenal fatigue recovery consists of taking up an adrenal fatigue diet, reducing or managing stress, getting enough rest and sleep, and doing mild forms of exercise that do not over excite the adrenal glands.
When you have depression, you may not be very motivated to do any of these things, and the benefits of ketamine may help give a short-term push to implement these changes. But even if you can’t get ketamine, it is very important that you still do your best to change your diet and lifestyle. Start small and work your way up. It is our recommendation that the first step you take when you have depression is to change your diet.
 First of all, it requires less energy or work to do than exercising or learning new stress-management skills, and it will give you the energy and nutrients you need to then take on the next task.
First of all, it requires less energy or work to do than exercising or learning new stress-management skills, and it will give you the energy and nutrients you need to then take on the next task.
The adrenal fatigue diet is also highly anti-inflammatory, which is very helpful for those with depression. Reducing inflammation may end up being all you need to do to counteract the excitotoxicity and toxic build-up in the system. The adrenal fatigue diet consists of 30-40% vegetables (half raw, half cooked), 20-30% animal protein, 20-30% healthy fats, like nuts and seeds, 10-20% legumes and beans, 10-20% whole grains, and 10-15% whole fruits. Try to eat organic as much as possible.
Also, the adrenal fatigue diet is not just about what you eat, but when you eat. You need to have regular meal times so that you avoid blood sugar spikes and crashes. Blood sugar spikes and crashes are a major source of stress on the body, and can actually induce anxiety. So, make sure you eat as soon as possible after waking up, preferably between 6:00 to 8:00 a.m., then have a snack at 10:00 a.m., lunch at 12:00 p.m., another snack at 3:00 p.m., dinner between 5:00 to 6:00 p.m., then a final small snack (such as nuts) before bed.
Once you have a good diet going, you can start to fill in any nutritional gaps using supplements. Some supplements are particularly effective in depression recovery, such as vitamin D3, B6, B12, folate, methylfolate, SAMe, and omega-3 fatty acids (from fish oil).
Adaptogens can also be useful as they help your body adapt to and cope with stress better. They include ashwagandha and Rhodiola. St. John’s wort is another commonly used herb for depression.
It’s vital to remember that with supplements, you shouldn’t try them out without proper supervision or support. What could be helpful with one condition or for one person could be harmful for another. This is especially the case with herbal remedies since they are potent and medicinal in nature. In some cases, some supplements can block the action of SSRIs and other medications.
With a robust diet and some high-quality supplements, you will begin to feel better, and at that time, you can look into doing some kind of physical activity. Exercise has been shown to increase your “feel good” brain chemicals and sometimes works just as effectively as antidepressant medications.
 If you have AFS, however, or any other debilitating chronic condition, you will need to start slowly and do very mild and gentle forms of exercise, so that you do not add stress to your system. Adrenal breathing exercises are good if you have more advanced stages of AFS, and then you can work your way up to adrenal yoga exercises, and then other forms of mild exercise.
If you have AFS, however, or any other debilitating chronic condition, you will need to start slowly and do very mild and gentle forms of exercise, so that you do not add stress to your system. Adrenal breathing exercises are good if you have more advanced stages of AFS, and then you can work your way up to adrenal yoga exercises, and then other forms of mild exercise.
Throughout all of these changes, you can begin to test out different stress management and stress reduction techniques. Going to therapy is something you should consider from the start, but joining group support programs, meditating, doing breathing exercises, journaling, reading self-help books, and engaging in activities that you enjoy can all lift your mood and provide you with a support structure that you can rely on.
Recovering from AFS and depression takes a while, and you need a lot of rest and good quality sleep to undertake this healing journey, so create a bedtime ritual that can help you relax and wind down. Make sure your room is cool and dark, don’t use your electronic devices before bed, and do your best to wake up at the same time each day.
Depression can wreak havoc on your life and make everything seem difficult and uncertain. Implementing a healthy daily routine may be challenging due to the lack of motivation you feel, but it is also what will return that sense of motivation to you. So take one step at a time and build a healthy day-to-day structure. Your body and mind will reap the rewards. And if you do have the chance to try out the benefits of ketamine, just make sure you do so under supervision and that your doctor understands your full health picture, including if you have AFS, first.
