Atopic dermatitis, i.e., eczema, is an autoimmune disease that has become relatively widespread over the last 50 years. At least 10 percent of American adults and up to a quarter of children across the globe suffer from this condition. Together with hay fever, instances of atopic dermatitis have more than doubled since the 1970s. And generally speaking, the healthcare community is baffled as to why.
Atopic dermatitis, i.e., eczema, is an autoimmune disease that has become relatively widespread over the last 50 years. At least 10 percent of American adults and up to a quarter of children across the globe suffer from this condition. Together with hay fever, instances of atopic dermatitis have more than doubled since the 1970s. And generally speaking, the healthcare community is baffled as to why.
The period seems too short for such a drastic increase in the number of people suffering from atopic dermatitis to completely be ascribed to evolution. Therefore, environmental, lifestyle, and dietary issues are more likely the sources of this increase.
In terms of environment, we are more exposed to toxins in the air we breathe, the food we eat, and even the products we use to clean our homes compared to 50 years ago. Our lifestyles have also changed quite significantly. Many people are less active, and children play outside less often than their grandparents did as children. But the biggest change that may be playing a role when it comes to the incidence of atopic dermatitis may be diet. As a population, we consume much more fast food than ever before. And highly processed foods tend to contain a lot more salt than homemade foods made from scratch.
According to recent studies, salt consumption may be linked to inflammation and an increase in the incidence of atopic dermatitis.
Atopic dermatitis is an autoimmune condition that causes itchy, red, inflamed skin. The chronic condition occurs as periodic flare-ups that usually begin during childhood and is often accompanied by allergies or asthma. Avoiding harsh soaps and regularly moisturizing may relieve the symptoms of atopic dermatitis.
Common symptoms associated with atopic dermatitis include:
In many cases, atopic dermatitis starts before the age of five and carries on into adulthood. Most people suffer from periodic flare-ups, although the condition may be absent for several years at a time.
 As an autoimmune disorder, atopic dermatitis is linked to inflammation, whereas inflammation, on the other hand, is your body’s response to stress. While many people think stress is a psychological issue, other factors like what you eat can, in fact, also put stress on the body. And this results in the same type of response as, for example, when you’re anxious. Actually, physiological factors may even have a more negative effect on inflammation than psychological stress.
As an autoimmune disorder, atopic dermatitis is linked to inflammation, whereas inflammation, on the other hand, is your body’s response to stress. While many people think stress is a psychological issue, other factors like what you eat can, in fact, also put stress on the body. And this results in the same type of response as, for example, when you’re anxious. Actually, physiological factors may even have a more negative effect on inflammation than psychological stress.
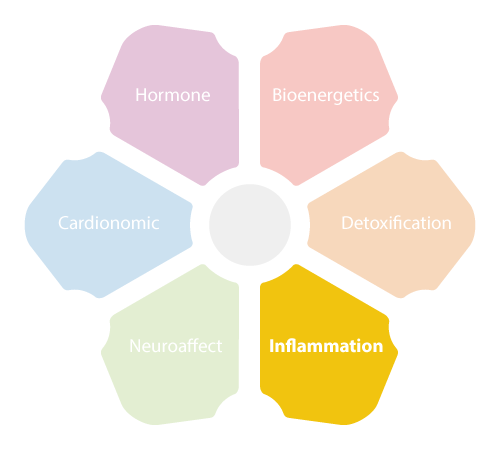
The NeuroEndoMetabolic (NEM) Stress Response is part of your body’s immune response to stress and is controlled by the Hypothalamic-Pituitary-Adrenal (HPA) axis. Activation of the NEM Stress Response leads to increased cortisol levels and at the same time, inflammation sets in and white blood cells rush to the sites of ‘injury’. Cortisol works as an inflammatory mediator and keeps inflammation in check.
However, imbalances in the circuits that control your body’s inflammatory response can occur at times, especially when stress is chronic. And sustained high levels of cortisol can negatively affect your immune and inflammatory responses.
Causes of this so-called Inflammation Circuit dysfunction include:
With inflammation and certain autoimmune conditions, such as atopic dermatitis, your immune system becomes overactive. Here, the immune cells that normally protect you from foreign invaders essentially becomes ‘confused’. And instead of only targeting pathogens, they also attack your body’s own cells. In other words, your immune system starts to indiscriminately attack its own tissues, resulting in the flare-ups associated with many autoimmune conditions.
 A recent study strongly suggests that salt contributes to the development of allergies and autoimmune conditions like atopic dermatitis. According to the experiments, high salt concentrations can affect T helper cells, which are the immune cells responsible for allergies. High levels of salt were often present in areas of the skin with atopic dermatitis. This could support the fast-food hypothesis, since eating fast foods can dramatically increases your salt consumption since process foods typically contain more salt than whole foods.
A recent study strongly suggests that salt contributes to the development of allergies and autoimmune conditions like atopic dermatitis. According to the experiments, high salt concentrations can affect T helper cells, which are the immune cells responsible for allergies. High levels of salt were often present in areas of the skin with atopic dermatitis. This could support the fast-food hypothesis, since eating fast foods can dramatically increases your salt consumption since process foods typically contain more salt than whole foods.
One experiment observed increased salt concentrations in the surrounding liquid medium used to grow two different types of immune cells, called CD4-positive memory T cells and naïve T cells. Both cells play an active role in the immune system but the CD4-positive have been previously exposed to antigens— foreign substances that can cause harm your body—whereas naïve T cells have not.
The results showed that both cell type boost cytokine production. Cytokines are substances secreted by immune cells during an inflammatory response and play an important role in regulating immunity, inflammation, and hematopoiesis (the production of the different cellular components found in blood and blood plasma). Salt was also found to enhance two types of salt-sensitive transcription factors, i.e., salt is involved in ‘switching on’ or ‘switching off’ certain genes.
 The researchers also examined salt levels in the skin of adults suffering from atopic dermatitis and found salt concentrations up to a 30 times higher in areas affected by the condition compared unaffected areas of skin or on people without the autoimmune condition.
The researchers also examined salt levels in the skin of adults suffering from atopic dermatitis and found salt concentrations up to a 30 times higher in areas affected by the condition compared unaffected areas of skin or on people without the autoimmune condition.
The same tests were conducted on people suffering from psoriasis, another autoimmune condition. However, psoriasis is mediated by different T helper cells. Interestingly, in this case, no differences in salt concentrations were found with between the skin of areas affected by psoriasis and the areas unaffected by the condition.
The studies described above seem to suggest that while salt intake may play a role in the development of atopic dermatitis, it does not seem to affect the development of psoriasis. However, more research is still needed to determine whether higher salt consumption could also contribute to allergies.
Nonetheless, based on the existing results, the researchers think the skin microbiome—as well as epidermal and dermal cells—could be involved in atopic dermatitis. In many cases, they discovered high concentrations of a particular salt-loving microbe, Staphylococcus aureus, on the skin of participants with atopic dermatitis. Moreover, the gut microbiome could also be a potential factor since a diet that high in salt can influence gut bacteria and may lead to inflammation elsewhere in the body.
The bottom line is that these conclusions are still highly speculative, and more research is needed determine the ‘how’ and the ‘why’.
At present, there is no medical ‘cure’ for atopic dermatitis. Therefore, the current focus is on addressing the symptoms. What we do know is that certain factors such as diet, lifestyle, exercise, and environment may play a role in the onset of atopic dermatitis. So, by addressing these issues, you may be able to mitigate the development of this condition or improve your symptoms. For starters, limiting your salt intake by making certain dietary changes could lead to improvements. You could also help manage the condition with natural remedies.
Several natural remedies can be used to help manage the varied symptoms associated with atopic dermatitis.


As with all autoimmune disorders, the focus tends to be on addressing the symptoms. While you can effectively mitigate the symptoms of atopic dermatitis, you’re not really addressing the root cause – inflammation. Indeed, Atopic dermatitis and other immune disorders may very well be symptoms of a bigger problem. Since inflammation is a systemic issue, reducing inflammation is a step-by-step process and it may take some time before you actually reap the benefits.
According to research, atopic dermatitis is indeed an autoimmune condition. And it may be the result of imbalances in your immune system and Inflammation Circuit, and could also possibly be related to higher salt consumption. So, diet could be one of the major contributors to the condition.