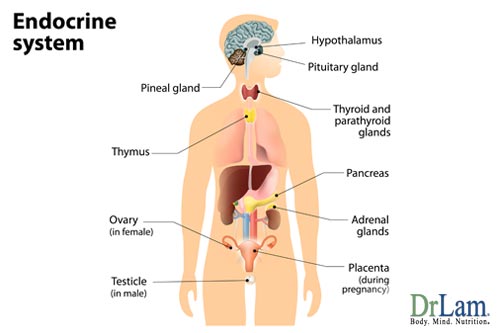
 The endocrine system is made up of eight different glands located strategically throughout the body. Three of the most important ones for females are the ovaries, adrenals, and the thyroid gland. Hormone imbalance symptoms often have a profound effect on the body.
The endocrine system is made up of eight different glands located strategically throughout the body. Three of the most important ones for females are the ovaries, adrenals, and the thyroid gland. Hormone imbalance symptoms often have a profound effect on the body.
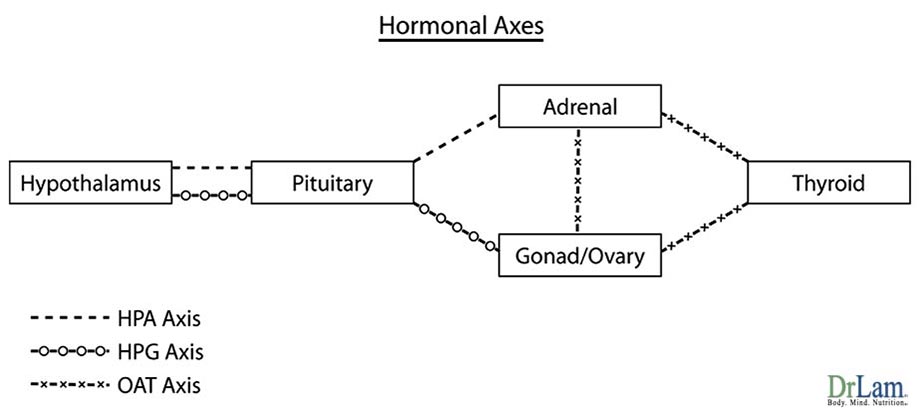
Control over the adrenal and ovarian systems starts at the hypothalamus. Specifically, the adrenal glands are regulated through the Hypothalamus-Pituitary-Adrenal (HPA) axis. Ovarian hormones are regulated through the Hypothalamus-Pituitary-Gonadal (HPG) axis. Each of the end organs (adrenals, thyroid, and ovaries) produces a variety of hormones that further exert their effects on the rest of the body. In addition, each of the end organs is tied into other organ systems hormonally via a series of networks or axes.
One such intricate hormonal axis ties in the adrenals, thyroid and the ovaries. This axis is called the Ovarian Adrenal Thyroid (OAT) axis. What happens to one organ will affect the other organs physiologically, clinically or sub-clinically. These three organs are therefore intimately co-dependent hormonally on each other for optimal function. If the adrenal glands are weak, there is often concurrent thyroid malfunction and menstrual cycle irregularity. Similarly, an under-active thyroid often makes adrenal fatigue worse off. Lastly, those who suffer from ovarian hormone imbalance symptoms such as estrogen dominance often have any pre-existing sub-clinical hypothyroidism exacerbated.
All three organs of this axis must be in a state of optimum balance for a woman to feel good. Like a three-legged stool, all three legs must be in perfect balance for the stool to be safe to sit on. Imbalance of the OAT axis leads to a myriad of conditions that are annoying in their mildest form and incapacitating when hormonal imbalance symptoms are severe.
Common complaints of those suffering from OAT Axis Imbalance include a mixture of hormone imbalance symptoms suggestive of concurrent decompensation of the adrenals, thyroid, and ovaries. Presenting hormone imbalance symptoms are often, but not always, suggestive of Adrenal Fatigue, estrogen dominance, and hypothyroidism. Commonly, hormone imbalance symptoms can include insomnia, fatigue, chronic fatigue, joint pain, exercise intolerance, brain fog, sugar intolerance, diabetes, dry skin, feeling cold, slow metabolism, inability to lose weight, PMS, endometriosis, irregular menstrual cycle, fibrocystic breast disease, anxiety, depression, and accumulation of fat at the waist line. These are just a few of the hormone imbalance symptoms and each woman is unique in how symptoms manifest and to what degree.
Those with ovaries removed can still have OAT Axis Imbalance because estrogen imbalances are involved and the ovaries are not the only place where estrogen is produced. The adrenal glands, as well as adipose tissue (fat cells), are also active production sites of estrogen.
OAT Axis Imbalance represents a state of hormonal axis irregularity yet to be recognized by conventional medicine. Its manifestation can be sub-clinical or clinical. Because its clinical presentation represents a convolution of multiple endocrine system imbalances, there is no definitive test that can isolate and precisely identify this imbalanced state with pinpoint accuracy. Formal and extensive research is sorely needed. Our current understanding of this state comes mainly from clinical experiences and case studies. As such, OAT Axis Imbalance should currently be viewed more appropriately as a clinical state and not as a disease state. This multi-organ clinical state that unifies common imbalances of the ovarian, adrenal, and thyroid systems into a triad should be considered only after conventional endocrine, diagnostic and therapeutic approaches have failed to bring relief and conventional investigative efforts have been exhausted.
Because of the myriad of hormone imbalance symptoms and the degree to which they vary from woman to woman, they often appear to be convoluted and diverse. Physicians, even those who are naturally oriented, can easily be overwhelmed.
In males, hormone imbalance symptoms are also prevalent with low libido and testosterone being a surrogate of ovarian imbalance. Low androgen levels also affect the thyroid and adrenal functions.
To understand this imbalance better, we have to examine each of these three organ systems and how they tie into the OAT axis.
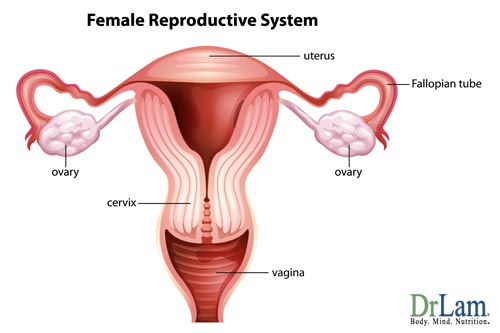
The ovaries normally maintain hormonal control in the female by self-regulation of the key hormones: estrogen and its opposing hormone, progesterone. Estrogen is produced by the ovaries, egg follicles, the adrenal glands and in fat cells. Progesterone is produced almost entirely by the corpus luteum: a little mass of fat cells left over from the follicle after the egg leaves it at ovulation.
Progesterone acts as the antagonist to estrogen. For example, estrogen stimulates breast cysts while progesterone protects against breast cysts. Estrogen enhances salt and water retention while progesterone is a natural diuretic. Estrogen has been associated with breast and endometrial cancers, while progesterone has a cancer preventive effect. Studies have shown that pre-menopausal women who were deficient in progesterone had 5.4 times the risk of breast cancer as compared to healthy women.
The following table clearly shows how progesterone and estrogen balances each other. It is very important to note that both hormones are necessary for optimum function. Progesterone will not work without some estrogen in the body to "prime the pump" as an example.
| Estrogen Effect | Progesterone Effect |
|---|---|
| Causes Endometrium to proliferate | Maintains secretory endometrium |
| Causes breast simulation that can lead to breast cancer | Protects against fibrocystic breast and prevents breast cancer |
| Increases body fat | Helps use fat for energy |
| Increases endometrial cancer risk | Prevents endometrial cancer |
| Restrains osteoclast function slightly | Promotes osteoblast function, leading to bone growth. |
| Reduces vascular tone | Restores vascular tone |
| Increases blood clot risk | Normalizes blood clot |
Estrogen and progesterone hormones work in synchronization with each other as checks and balances to achieve hormonal harmony in both sexes. It is not the absolute deficiency of estrogen or progesterone but rather the relative dominance of estrogen and relative deficiency of progesterone that is the main culprit behind its role in OAT Axis Imbalance.
Let us take a closer look. While sex hormones such as estrogen and progesterone decline with age gradually, there is a drastic change in the rate of decline for these two hormones during the perimenopausal and menopausal years for women. From age 35 to 50, there is a seventy-five percent reduction in production of progesterone in the body. Estrogen, during the same period, only declines about 35 percent. By menopause, the total amount of progesterone made in the body is extremely low, while estrogen is still present in the body at about half its pre-menopausal level. When ovulation ceases, progesterone is no longer produced except for a very small amount made by the adrenal glands.
 With the gradual drop in estrogen accompanied by a severe drop in progesterone, there is insufficient progesterone to counteract the amount of estrogen in our body. This state is called estrogen dominance. Many women in their mid-thirties, most women during peri-menopause (mid-forties), and essentially all women during menopause (age 50 and beyond) are overloaded with estrogen and at the same time suffering from progesterone deficiency because of the severe drop in physiological production during this period.
With the gradual drop in estrogen accompanied by a severe drop in progesterone, there is insufficient progesterone to counteract the amount of estrogen in our body. This state is called estrogen dominance. Many women in their mid-thirties, most women during peri-menopause (mid-forties), and essentially all women during menopause (age 50 and beyond) are overloaded with estrogen and at the same time suffering from progesterone deficiency because of the severe drop in physiological production during this period.
The primary causes include excessive environmental estrogen, obesity, stress, poor diet, lack of exercise, and unopposed estrogen given as part of a hormone replacement therapy. In addition, adrenal dysfunction and an underactive thyroid can worsen estrogen dominance and hormone imbalance symptoms.
Typical complaints from patients suffering with hormone imbalance symptoms include swollen breasts and ring fingers, impatience and irritability, stomach cramps before menstrual cycles, irregular periods, fluid retention, foggy thinking, depression, and fatigue. It is the underlying common denominator for a variety of illnesses and syndromes that were previously regarded as unrelated entities. They in fact represent different expressions of the same illness in different cell settings. The continuum is a state of excessive estrogen throughout one's lifetime, with different manifestations at different times, starting with endometriosis, PMS, fibrocystic breast disease, PCOS and progressing to fibroids and breast cancer.
Estrogen dominance may increase thyroid-binding proteins in the bloodstream. Thyroid blood test results may therefore be normal although there may be insufficient thyroid hormone in the tissues, resulting in a state of sub-clinical or clinical hypothyroidism.
When estrogen levels are high, the adrenal cortex fails to respond to signals from the brain. In other words, even though the brain is requesting more cortisol to be made, there is a blunted response from the adrenals in the face of this request. As a result, cortisol output is sub-optimal relative to the demand signal. In addition, estrogen impairs adrenal function by interfering with the release of cortisol from the adrenal cortex. High levels of estrogen can lead to a corresponding increase in the level of cortisol-binding globulin. In turn, the cortisol-binding globulin interferes with hormone functions and circulates in the bloodstream, binding to cortisol, and rendering it inactive. Thus, a woman with estrogen dominance may have adequate levels of total cortisol in her bloodstream. Her total cortisol level blood tests may be well within normal range but her free, available cortisol level may be low. Since only free cortisol can pass through cell membranes and activate receptors inside the cells, the effectiveness of cortisol is blunted at the cellular level.
Just as estrogen dominance can contribute to adrenal insufficiency, adrenal insufficiency can contribute to estrogen dominance. Cortisol is made in the adrenal cortex from progesterone. When the adrenals are weak, there is a tendency towards a lowered progesterone output in favor of cortisol. A low progesterone level is often the result, leading to a state of relative estrogen dominance with its many undesirable consequences mentioned above. This forms an adverse feedback loop and vicious cycle. Excessive estrogen affects both thyroid and adrenal function. In turn, dysfunctional thyroid and Adrenal Fatigue make estrogen dominance worse off.
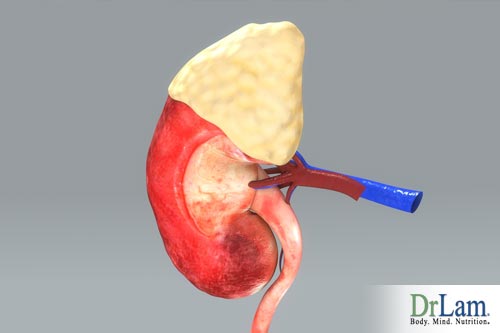 The adrenal glands are the main stress control system of the body. Adrenal Fatigue is a decrease in the adrenal glands' ability to carry out this normal function. It is commonly caused by chronic stress from any source (including emotional, physical, mental, or environmental) that exceeds the body's capacity to adjust appropriately to the demands placed on it. Adrenal Fatigue has a broad spectrum of non-specific yet often debilitating symptoms. The onset of this disease is often slow and insidious.
The adrenal glands are the main stress control system of the body. Adrenal Fatigue is a decrease in the adrenal glands' ability to carry out this normal function. It is commonly caused by chronic stress from any source (including emotional, physical, mental, or environmental) that exceeds the body's capacity to adjust appropriately to the demands placed on it. Adrenal Fatigue has a broad spectrum of non-specific yet often debilitating symptoms. The onset of this disease is often slow and insidious.
Stressors that can lead to Adrenal Fatigue include anger, chronic illness, depression, surgery, high sugar intake, over exercise, and sleep deprivation, just to mention a few. One of the most commonly overlooked causes of Adrenal Fatigue is chronic or severe infection. Such infections can occur sub-clinically with no obvious signs at all. Parasitic and bacterial infections including Giardia and H. pylori are often the main culprits. Often overlooked can be a tooth that has had root canal work done but still contains germs that secrete toxins chronically.
Signs and symptoms of Adrenal Fatigue include tendency to gain weight, especially around the waist, and inability to lose it; high frequency of the flu and other respiratory diseases where symptoms tend to last longer than usual; a tendency to tremble when under pressure; PMS, infertility, and hormone imbalance symptoms; reduced sex drive; lightheadedness when rising from a supine position; brain fog; lack of energy in the afternoon; reliance on coffee to get the day started; cravings for salty and fatty foods; chronic pain of unknown origin; and feeling better during a vacation. None of the signs or symptoms by themselves can definitively diagnose Adrenal Fatigue. When taken as a group, these signs and symptoms do form a picture of a person under stress with Adrenal Fatigue Syndrome.
Stage 1: Alarm Reaction (Flight or Fight Response). At this stage, the body is alarmed by stressors and mounts an aggressive anti-stress response to reduce stress levels. There are generally no outward symptoms of decompensation, as the anti-stress response mediated by an increased cortisol output from the adrenals is well within the body's output capacity. The person conducts life normally but does notice that coffee helps to get the day going, even though an ever-increasing amount may be needed.
Stage 2: Resistance Response. With chronic or severe stress, the adrenals eventually are unable to keep up with the body's demand for cortisol. Normal daily functions can be carried out, but the sense of fatigue is pronounced at the end of each day as the body needs more rest than usual to recover. Despite a full night's rest, the body does not feel refreshed in the morning. Anxiety starts to set in, and the person becomes easily irritable. Insomnia becomes more common, as it takes longer to fall asleep. There is also frequent awakening as well. Infections can become more recurrent. PMS, menstrual irregularities and other hormone imbalance symptoms surface, and symptoms suggestive of hypothyroidism (such as sensations of feeling cold and a sluggish metabolism) become prevalent.
 Stage 3: Exhaustion. As adrenal function weakens further, the body's need for adrenal hormones remains unabated if stress is not reduced. The adrenals are having tremendous difficulty and may no longer be able to keep up with the ever-increasing demand for cortisol production. Cortisol output may plateau and start to decline. This progression usually happens gradually over a long period of time, perhaps years.
Stage 3: Exhaustion. As adrenal function weakens further, the body's need for adrenal hormones remains unabated if stress is not reduced. The adrenals are having tremendous difficulty and may no longer be able to keep up with the ever-increasing demand for cortisol production. Cortisol output may plateau and start to decline. This progression usually happens gradually over a long period of time, perhaps years.
Because the variety of symptoms presented at this stage can be convoluted and overwhelming, it is helpful, from a clinical recognition perspective only, to further delineate this stage into four broad overlapping phases. The boundaries of each phase are decidedly indistinct. They do not represent an absolute sequential gradation process and should not be viewed as such. Most if not all suffering from adrenal exhaustion usually present signs and symptoms in various degrees of each phase concurrently. That is the norm. The more advanced the exhaustion, however, the more late phase manifestation is presented.
 Phase C - Disequilibrium State. As the body continues its downward path of impaired function, it gathers steam. The hormone imbalance symptoms become unmanageable. Gradually, the body becomes severely compromised in trying to maintain its fine control of homeostasis. Normal equilibrium is therefore lost. The body will try its hardest to maintain equilibrium through activation of various compensatory responses within the autonomous nervous system but its crude response and damaged receptor sites along with impaired metabolic and detoxification pathways give rise to paradoxical and exaggerated responses. The body's internal thermostat is "broken". Common hormone imbalance symptoms at this stage include heart palpitation, dizziness, orthostatic hypotension, anxiety, adrenaline rush, temperature intolerance and strong heartbeat.These crude and exaggerated responses will further undermine the existing weak adrenal function. Clinical manifestations of this include swings in blood sugar level, fragile blood pressure state, reactive hyper-adrenergic responses including heart palpitations, night sweats, and a state of hyper-anxiety followed by depression. Sufferers are usually frustrated and feel abandoned by their physicians. The body is literally "falling apart" internally. Sufferers at this stage are often incapacitated and frequently called the "living dead". It is imperative that healthcare at this point be totally put under a qualified specialist physician as this level of dysfunction is well beyond the expertise of even the most astute of naturally oriented health care providers.
Phase C - Disequilibrium State. As the body continues its downward path of impaired function, it gathers steam. The hormone imbalance symptoms become unmanageable. Gradually, the body becomes severely compromised in trying to maintain its fine control of homeostasis. Normal equilibrium is therefore lost. The body will try its hardest to maintain equilibrium through activation of various compensatory responses within the autonomous nervous system but its crude response and damaged receptor sites along with impaired metabolic and detoxification pathways give rise to paradoxical and exaggerated responses. The body's internal thermostat is "broken". Common hormone imbalance symptoms at this stage include heart palpitation, dizziness, orthostatic hypotension, anxiety, adrenaline rush, temperature intolerance and strong heartbeat.These crude and exaggerated responses will further undermine the existing weak adrenal function. Clinical manifestations of this include swings in blood sugar level, fragile blood pressure state, reactive hyper-adrenergic responses including heart palpitations, night sweats, and a state of hyper-anxiety followed by depression. Sufferers are usually frustrated and feel abandoned by their physicians. The body is literally "falling apart" internally. Sufferers at this stage are often incapacitated and frequently called the "living dead". It is imperative that healthcare at this point be totally put under a qualified specialist physician as this level of dysfunction is well beyond the expertise of even the most astute of naturally oriented health care providers.As this happens to one organ system, the rest of the body also down-regulates and reacts unfavorably. Digestion slows to conserve energy, clearance of metabolites slows to conserve energy, and basal metabolic rate drops to conserve energy. Weight loss is extremely difficult. At this phase, the adrenals have lost most of their ability to serve as the body's stress control center. It becomes hypersensitive and reacts negatively to any attempts to jump start it for reasons not well understood. The adrenals continue to exhibit frequent crashes through physiological mechanisms that defy conventional scientific logic. Current concepts point to the likelihood of pump failure, low-clearance state, positive feedback loops, receptor site dysfunction, and electron driven retoxifications as possible etiologies for the wide variety of extreme paradoxical reactions commonly seen in this phase. Basic nutrients critical to proper adrenal function, such as Vitamin C, become severely depleted.  Administration of Vitamin C, cortisol, DHEA, and pregnenolone, all of which are normally required and welcomed by the adrenals, cease to bring about any improvement in symptoms but may instead become ineffective and possibly toxic. The more the adrenals are exhausted, the less the adrenals can tolerate medication or nutrients, even in small doses. Nothing appears to work in this phase. Any attempted administration of nutrients by mouth or by intravenous injection in fact may make the condition worse. The brutal downward decompensatory cycle is well entrenched. Sufferers become desperate and try to overcome their physical and mental exhaustion on their own to no avail. Depression sets in and suicidal tendencies surface.
Administration of Vitamin C, cortisol, DHEA, and pregnenolone, all of which are normally required and welcomed by the adrenals, cease to bring about any improvement in symptoms but may instead become ineffective and possibly toxic. The more the adrenals are exhausted, the less the adrenals can tolerate medication or nutrients, even in small doses. Nothing appears to work in this phase. Any attempted administration of nutrients by mouth or by intravenous injection in fact may make the condition worse. The brutal downward decompensatory cycle is well entrenched. Sufferers become desperate and try to overcome their physical and mental exhaustion on their own to no avail. Depression sets in and suicidal tendencies surface.
This is not a state to be in for self-navigating. Expert professional guidance is absolutely needed. Unfortunately, qualified physicians in this area are extremely rare.
Stage 4: Failure. Eventually, the adrenals are totally exhausted. Patients at this stage have a high chance of cardiovascular collapse and death. When Adrenal Fatigue has advanced to this stage, the line between it and Addison's disease, also called adrenal insufficiency, can become blurry. Symptoms at this stage include sudden penetrating pain in the lower back, abdomen or legs, severe vomiting and diarrhea, dehydration, low blood pressure and loss of consciousness. Addisonian crisis is rare; in most cases the symptoms are severe enough that patients are quick to seek medical treatment before a crisis occurs. However, in about 25 percent of patients, the symptoms first appear during an Addisonian crisis. Left untreated, an Addisonian crisis can be fatal. While the etiology of the conditions may be different, the ultimate clinical presentations can be quite similar in both Addisonian crisis and Stage 4 Adrenal Fatigue as they represent a continuum of decompensation in adrenal functions.
As the body progresses through to the more advanced stages of Adrenal Fatigue, the overall array of symptoms generally become more pronounced and convoluted. Fatigue can become unbearable as the body's ability to deal with normal stresses of life weakens with each stage. In severe cases of Adrenal Fatigue, the body can often exhibit multiple unusual and paradoxical reactions that one does not normally expect. This is especially prevalent in Stage 3. This is reflective of deepening adrenal exhaustion, with disequilibrium, loss of homeostasis, multiple endocrine axis imbalance, pump failure, receptor site sensitivity or retoxification reaction of the body. Symptoms can include:
 Although sub-clinical adrenal dysfunction and its various stages were recognized as distinct clinical syndromes since the turn of the 20th-century, most conventional physicians are unfamiliar with this condition because it is difficult to diagnose correctly by traditional blood tests. Adrenal hormones may be low in the case of Adrenal Fatigue, but are still within the "normal" range and not low enough to warrant the diagnosis of Addison's disease by regular blood tests. Conventional physicians are not taught the significance of sub-clinical Adrenal Fatigue. They are misguided by the results of blood tests, which unfortunately, are not sensitive enough to detect sub-clinical Adrenal Fatigue. As a result, patients tested for adrenal functions are told they are "normal" but in reality, their adrenal glands are performing sub-optimally, with clear signs and symptoms coming from the body that are crying out for help and attention.
Although sub-clinical adrenal dysfunction and its various stages were recognized as distinct clinical syndromes since the turn of the 20th-century, most conventional physicians are unfamiliar with this condition because it is difficult to diagnose correctly by traditional blood tests. Adrenal hormones may be low in the case of Adrenal Fatigue, but are still within the "normal" range and not low enough to warrant the diagnosis of Addison's disease by regular blood tests. Conventional physicians are not taught the significance of sub-clinical Adrenal Fatigue. They are misguided by the results of blood tests, which unfortunately, are not sensitive enough to detect sub-clinical Adrenal Fatigue. As a result, patients tested for adrenal functions are told they are "normal" but in reality, their adrenal glands are performing sub-optimally, with clear signs and symptoms coming from the body that are crying out for help and attention.
The adrenal glands are usually the first in the order of endocrine functions to breakdown when stress has overwhelmed the body's normal compensatory response. Unfortunately, this is seldom recognized as a pathological state. Acceptable social compensatory actions such as coffee intake often mask the underlying problem as the adrenals are put in over-drive to cover up the early signs and symptoms of Adrenal Fatigue. The next endocrine gland to be affected is the insulin-producing portion of the pancreas. The body's blood sugar becomes imbalanced and this dysfunction is temporarily fixed by the intake of soda drinks, energy potions and donuts. After the pancreas comes the thyroid. Sluggishness, feeling cold and weight gain are the predominant symptoms that bring patients to their physicians, usually for the first time. This is often when hypothyroidism is first diagnosed. Thyroid replacement medication is routinely prescribed. However, over 70 percent of those patients taking thyroid medications still are symptomatic over time. Along with hypothyroid are symptoms of estrogen dominance, a state reflective of ovarian system dysfunction. Presenting symptoms include PMS, endometriosis, lumpy breasts, and irregular menstrual cycle. Hormone replacement medication may work short term, but unless the adrenals are first attended to, the patient's response is often blunted and ultimately fails. Finally, the parathyroid glands, the pineal gland, the autonomic nervous system, and the hypothalamus become affected. By this time, the OAT axis is severely imbalanced.
Adrenal Fatigue is often the last to be detected and only considered seriously when the patient is already severely decompensated, with concurrent severe ovarian and thyroid involvement. Even when detected, there is inadequate attention paid to the frequent concurrent ovarian and thyroid imbalance in what is now a full-blown state of Ovarian-Adrenal-Thyroid (OAT) axis imbalance.
The key to this imbalance lies in the adrenal glands, for it is there that cortisol is modulated. In Adrenal Fatigue, internal cortisol imbalance often creates a condition of multiple organ resistance, including the thyroid and ovaries. Adrenal Fatigue is an important common and often overlooked cause of secondary clinical or sub-clinical hypothyroidism. Classically, the patient presents himself to the doctor's office complaining of fatigue, dry skin, weight gain, low body temperature, and insomnia.  Thyroid laboratory test results show either normal or high TSH, normal or low T3 and free T3, normal or low T4 and free T4. The patient is normally prescribed a variety of thyroid replacement medications. Temporary improvement may be experienced by the patient but the improvement ultimately fails as recovery response is blunted and the symptoms continue to persist. Excessive thyroid medicine may be prescribed to normalize what may appear to be sub-optimal blood levels. The body is put on overdrive as the basal metabolic rate is raised. This can unmask pre-existing adrenal weakness; exacerbating existing Adrenal Fatigue and triggering adrenal exhaustion and adrenal crisis. Anti-depressants are often prescribed as a solution to control symptoms as the physicians run out of options to help the sufferer. This seldom works but will instead often make the OAT imbalance worse off.
Thyroid laboratory test results show either normal or high TSH, normal or low T3 and free T3, normal or low T4 and free T4. The patient is normally prescribed a variety of thyroid replacement medications. Temporary improvement may be experienced by the patient but the improvement ultimately fails as recovery response is blunted and the symptoms continue to persist. Excessive thyroid medicine may be prescribed to normalize what may appear to be sub-optimal blood levels. The body is put on overdrive as the basal metabolic rate is raised. This can unmask pre-existing adrenal weakness; exacerbating existing Adrenal Fatigue and triggering adrenal exhaustion and adrenal crisis. Anti-depressants are often prescribed as a solution to control symptoms as the physicians run out of options to help the sufferer. This seldom works but will instead often make the OAT imbalance worse off.
It is important to recognize that optimum adrenal function plays a key role in thi imbalance. When the adrenals are weak, cortisol induced organ resistance applies to nearly all other hormone regulated organs including the ovaries, the thyroid, and the pancreas. Few hormones are allowed to work at their optimal levels in the presence of Adrenal Fatigue. A multitude of hormones including insulin, progesterone, estrogen and testosterone become affected. The normal negative feedback loop can be blunted and binding carrier hormones in the blood can be disrupted. The ability of each hormone to regulate and fine-tune its target organ to achieve homeostasis is therefore often compromised. Blood pressure can become erratic, blood sugar levels may experience wide swings, bipolar and anxiety states come at will, reactive adrenaline rush becomes uncontrollable, brain fog becomes prevalent, metabolic function slows down and menstrual flow becomes irregular.
Due to their lack of clinical training on Adrenal Fatigue, clinicians often find themselves treating symptoms of weak thyroid and ovarian systems while ignoring adrenal dysfunction. Let us take a look at how this can have devastating effect. In early stages of Adrenal Fatigue, cortisol output is high as the body attempts to neutralize stress by producing more of it. However, when too much cortisol is produced, it will have multiple undesirable effects. For example, cortisol blocks the progesterone receptors, making them less responsive to progesterone. Progesterone normally produced by the adrenals comes to a halt in favor of cortisol production.
Insufficient progesterone production leads to an imbalance between estrogen and progesterone. With reduced progesterone to offset estrogen, the body may experience estrogen dominance and hormone imbalance symptoms. It is no coincidence that we see a proliferation of conditions associated with excessive estrogen such as PMS, fibroids, and pre-menopausal syndrome and other hormone imbalance symptoms when women reach their mid thirties and early forties.
Many chronically ill patients have both low adrenal and thyroid function. In such cases, it is important to begin the recovery process by supporting the adrenal glands before raising the thyroid hormone. Otherwise, increased circulation of the thyroid hormone may further strain the already weak adrenal glands, leading to adrenal crashes and further decompensation. Recovery plans focusing on single organ dysfunction without considering the axis imbalance often fail and may in fact make the condition worse off.
 Attempts to rebalance ovarian and thyroid hormones without careful attention to adrenal hormones often fail and may worsen hormone imbalance symptoms. Conversely, an approach focusing on adrenals first often leads to spectacular results as the ovarian hormones and the thyroid hormones will often rebalance themselves as the adrenal glands recover.
Attempts to rebalance ovarian and thyroid hormones without careful attention to adrenal hormones often fail and may worsen hormone imbalance symptoms. Conversely, an approach focusing on adrenals first often leads to spectacular results as the ovarian hormones and the thyroid hormones will often rebalance themselves as the adrenal glands recover.
The thyroid gland acts like the body's barometer. Its main function is to help cells convert oxygen and calories into energy. It regulates heart rate, blood pressure, body temperature, metabolism, and growth.
More than 10 million Americans have been diagnosed with thyroid disease and another 13 million people are estimated to have undiagnosed thyroid problems. About 10 percent of the adult population is afflicted with this frequently overlooked disease of epidemic proportions. A dysfunctional thyroid can affect almost every aspect of health. It is one of the most under-diagnosed hormonal imbalances of aging, along with estrogen dominance and Adrenal Fatigue. It is estimated by age 50, one out of every twelve women has some degree of hypothyroidism. By age 60, it is one out of six. In fact, among the elderly, hypothyroidism is sometimes misdiagnosed as dementia.
The thyroid gland, signaled by TSH, secretes two essential thyroid hormones: triiodothyronine (T3) and thyroxine (T4), which are responsible for regulating cell metabolism in every cell in your body. A healthy person secretes all of the circulating T4 (about 90 to 100 mcg daily) and about 20 percent of the circulating T3. The T4 made by the thyroid gland circulates throughout the body and is converted into approximately equal amounts of T3 and reverse T3 ( rT3). Most of the biological activity of thyroid hormones is due to T3. It has a higher affinity for thyroid receptors and is approximately four times more potent than T4. rT3 acts as a braking system to T3. Not only is it inactive (having only 1 percent of T3 activity), it binds to T3 receptors and blocks the action of T3. T4 should therefore be considered a pro-hormone and precursor to T3 and rT3. The normal physiological production ratio of T4 to T3 is 3.3:1. A properly functioning thyroid gland requires a perfect balance of T4, T3, and rT3. The T3/rT3 ratio is therefore one of the most useful markers for true tissue hypothyroidism and a crucial marker of diminished cellular function.
There are a variety of factors that can contribute to the development of thyroid problems: such as exposure to external radiation, over-consumption of soy products, taking drugs such as lithium that have anti-thyroid effects, over-consumption of uncooked "goitrogenic" foods - such as broccoli, turnips, radishes, cauliflower and Brussels sprouts - adrenal insufficiency or fatigue (commonly caused by chronic stress), mercury intoxication (amalgams are 50 percent mercury), auto-immune diseases and infection.
As one of the master regulators of body metabolism, low thyroid function elicits a global response. Symptoms include:

Hypothyroidism can be primary or secondary. Primary hypothyroidism can easily be cured with administration of thyroid replacement therapy. If hypothyroidism symptoms such as low body temperature, fatigue, dry skin and weight gain persist despite thyroid replacement therapy regardless of laboratory values, one must look elsewhere for the cause of low thyroid function.
Secondary hypothyroidism is low thyroid function caused by malfunction of another organ system. One of the most frequently overlooked causes is Adrenal Fatigue. Adrenal Fatigue is perhaps the most common cause of secondary hypothyroidism, both clinically and sub-clinically. Low adrenal function often leads to low thyroid function, classically evidenced by high thyroid binding globulin (TBG), low free T4, low free T3, high TSH, and low body temperature. Few physicians are trained to detect this connection. Fortunately, secondary hypothyroidism can be reversed when the underlying root problem (such as Adrenal Fatigue) is resolved.
Thyroid imbalance is perhaps the single most confusing, convoluted and difficult to manage of all endocrine disorders. Attempts to manage thyroid symptoms without a full understanding of the intricate underlying root cause - as it is tied to the ovarian and adrenal systems - often fails over time.
The thyroid is intricately related to the ovarian and adrenal systems. By its regulation of metabolism, it affects reproductive gland activities. The thyroid influences production of SHBG (sex hormone binding globulin), prolactin, and GnRH (gonadotropin releasing hormone), all of which affect the menstrual cycle and the ability to become pregnant. Thyroid hormones also stimulate progesterone production in the ovaries. Pregnancy is not possible unless there is sufficient progesterone to provide a supportive environment in the uterus for the egg. It is not unusual for women to overcome their infertility problems when their sub-clinical hypothyroidism is resolved. Iodine, a key supportive compound for the thyroid, is one of the best natural cures for fibrocystic breast diseases.
Thyroid abnormalities can create menstrual cycle problems in younger women as well as more mature women. Women with PCOS and infertility problems commonly have chronically low progesterone.  In premenstrual women, these problems are often exacerbated. Untreated thyroid problems can contribute to infertility, PMS, and menopause symptoms. In addition, thyroid hormones have similarities with certain metabolites of estrogen and progesterone, and receptor sites for thyroid uptake can be blocked or facilitated by estrogen and progesterone. Imbalances of thyroid hormones T3 and T4, combined with imbalances of estrogen and progesterone, can mimic symptoms of menopause, with adverse effects on mood, temperature regulation, fluid retention, energy and sleep. Women with normal TSH values may in fact be in a state of sub-clinical hypothyroidism and not know it.
In premenstrual women, these problems are often exacerbated. Untreated thyroid problems can contribute to infertility, PMS, and menopause symptoms. In addition, thyroid hormones have similarities with certain metabolites of estrogen and progesterone, and receptor sites for thyroid uptake can be blocked or facilitated by estrogen and progesterone. Imbalances of thyroid hormones T3 and T4, combined with imbalances of estrogen and progesterone, can mimic symptoms of menopause, with adverse effects on mood, temperature regulation, fluid retention, energy and sleep. Women with normal TSH values may in fact be in a state of sub-clinical hypothyroidism and not know it.
The thyroid is closely tied to the adrenal system as well. When the adrenals are exhausted, the ability of the adrenals to handle the stress associated with normal bodily functions and energy requirements is often compromised. To enhance survival, the adrenals force a downregulation of energy production. In other words, the body is being metabolically downregulated in order to conserve energy. The body needs to rest. Lower energy output reduces workload on the body. In times of stress, this is exactly what the body wants. As the thyroid down-regulates, T3 and thus T4 production is reduced. The down-regulation also leads to an increase in thyroid binding globulin (TBG). As a result of increased TBG, more thyroid hormones are bound on a relative basis and less is released to the cell where it works. This leads to reduced free T4 and free T3 levels as measured in the blood (while total T3 and T4 may be normal). Last but not least, cortisol itself can inhibit the conversion of T4 into T3, and may affect their entry into cells as well. In this downregulation process to enhance survival, the body also shunts some of the available T4 towards the production of the inactive reverse T3 (rT3). rT3 acts as a braking system and opposes the function of T3. This reduction in T3 combined with increase in rT3 may persist even after the stress passes and cortisol levels have returned to normal. Furthermore, rT3 itself may also inhibit the conversion of T4 to T3. This may perpetuate the production of the inactive rT3. If the proportion of rT3 dominates then it will antagonize T3, possibly leading to a state called rT3 dominance. This results in hypothyroidism symptoms despite sufficient circulating levels of T4 and T3. The body therefore has multiple pathways to down-regulate energy production to enhance survival under the direction of the adrenal glands.
Laboratory test results of T4 and T3 may be normal while classic symptoms of hypothyroidism are evident with persistent low body temperature and slow ankle reflex. Alternatively, laboratory test results of free T4 and free T3 may be low while TSH is normal or high. In both scenarios, thyroid replacement with T4 and T3 without first considering adrenal fortification is a common mistake and often leads to a worsening state of OAT axis imbalance. The reason is simple. Thyroid replacements tend to increase metabolic function.  Raising the basal metabolic rate is akin to putting all systems of the body into overdrive at a time when the body is trying to rest by downregulating through the many mechanisms described above. The body's survival mechanism is designed to achieve a reduction, not an increase in levels of T4 and T3. What the body wants (to slow down) and what the medications are designed to do (to speed up) are diametrically opposed to each other.
Raising the basal metabolic rate is akin to putting all systems of the body into overdrive at a time when the body is trying to rest by downregulating through the many mechanisms described above. The body's survival mechanism is designed to achieve a reduction, not an increase in levels of T4 and T3. What the body wants (to slow down) and what the medications are designed to do (to speed up) are diametrically opposed to each other.
Administering thyroid medication in the case of advanced Adrenal Fatigue without concurrent attention to adrenal recovery often fails as a result. In many cases, it is analogous to pouring oil onto a fire. An already weak adrenal system in a low energy state may not be able to carry the extra energy output burden. What the adrenals need is rest, not extra work.
Thyroid medication administered under such circumstances may lead to a temporary relief of symptoms and a slight boost in energy at first. This is often short lived. Ultimately, fatigue returns, as thyroid medication further undermines the pre-existing adrenal weakness and often precipitates adrenal crisis. The overall fatigue level continues to increase well beyond what the medication is trying to combat. Only by increasing the medication dosage or switching to more powerful thyroid medication can the worsening fatigue be avoided.
Let us look at this in more detail. While laboratory levels of T4, T3 and TSH may appear to be improved once thyroid replacement medication is administered, the patient clinically continues to show lack of improvement and often his condition gets worse over time. Physicians can be misled by "improving" laboratory results as being "on the right track" and not be attuned to the possible concurrent underlying adrenal dysfunction that remains the main culprit. Unless FT4, FT3, and rT3 values are factored into the clinical picture, the true cellular delivery of thyroid medication is not known. The body's persistent low body temperature is a cry for action that is not being attended to. The unsuspecting physician may continue to increase thyroid medication dosage in an attempt to relieve unpleasant and unresolved hypothyroidism symptoms. This approach seldom works long term as mentioned earlier and unknowingly subjects the patient to the medication's unintended negative effects on the adrenal glands that overshadow any of its benefit on the thyroid glands. As long as the adrenals are still functioning, they will continue to downregulate as much as they can, blunting the body's response to the thyroid medication. Over time, despite improving or stabilizing T4, T3, and TSH levels that may be considered within normal range, the patient still needs an ever larger dose of medication clinically in order to keep the symptoms at bay. The patient continues with unresolved symptoms and with low body temperature that refuses to normalize while classic signs of hypothyroidism persist despite medication.
 As mentioned earlier, the patients usually present themselves initially to the doctor's office with high or normal TSH, low or normal T3, free T3, T4, free T4, along with persistent low body temperature. They are then typically started on thyroid replacement for primary hypothyroidism as the adrenal component is overlooked. When the symptoms fail to improve, the tendency is to switch from one medication to another. Starting with synthetic T4, to T4/T3 blends, and ultimately, to potent T3, the patient is subjected to ongoing trial and error as one drug after another is tried. As this is going on, the body continues to decompensate as the medication dispensed becomes stronger and stronger. The patient's condition often continues to get worse despite the physician's best attempt to help. It comes as no surprise that as much as 70 percent of patients on thyroid replacement continue to complain of hypothyroidism symptoms over time. Ultimately, the patient's body is overloaded with thyroid medication while adverse side effects such as heart palpitation and tremors surface and the patient continues to feel fatigued and sluggish. This state is known as being "wired and tired."
As mentioned earlier, the patients usually present themselves initially to the doctor's office with high or normal TSH, low or normal T3, free T3, T4, free T4, along with persistent low body temperature. They are then typically started on thyroid replacement for primary hypothyroidism as the adrenal component is overlooked. When the symptoms fail to improve, the tendency is to switch from one medication to another. Starting with synthetic T4, to T4/T3 blends, and ultimately, to potent T3, the patient is subjected to ongoing trial and error as one drug after another is tried. As this is going on, the body continues to decompensate as the medication dispensed becomes stronger and stronger. The patient's condition often continues to get worse despite the physician's best attempt to help. It comes as no surprise that as much as 70 percent of patients on thyroid replacement continue to complain of hypothyroidism symptoms over time. Ultimately, the patient's body is overloaded with thyroid medication while adverse side effects such as heart palpitation and tremors surface and the patient continues to feel fatigued and sluggish. This state is known as being "wired and tired."
Those who have hypothyroidism but fail to improve after taking thyroid replacement medication should therefore always investigate Adrenal Fatigue as a possible etiology for their thyroid problem. Normalization of adrenal function in such cases is key and often leads to spontaneous resolution of hypothyroidism symptoms. The faster the patient with Adrenal Fatigue recovers, the faster the symptoms of hypothyroidism will be resolved. This can happen in a matter of weeks. Those who are on thyroid replacement will invariably find that less medication is needed as their adrenal function normalizes. In fact, one can become overmedicated and thus run the risk of hyperthyroidism if thyroid medication is not reduced as one recovers from Adrenal Fatigue. This is an important yardstick and a good gauge of improvement in adrenal function. The credit goes to the adrenal glands and not to the thyroid gland. As adrenal function improves, the need for downregulation subsides and thyroid function suppression is lifted, leading to normalization of thyroid function. For those pursuing thyroid recovery by way of adrenal fortification first, it comes as no surprise to see the body regaining energy without increasing thyroid medication after years of relying on such medication. In fact, thyroid replacement medication may not be necessary and can be tapered off totally over time as adrenal function normalizes.
It is important to note that laboratory tests of thyroid function during this adrenal focused thyroid recovery, will continue to show low thyroid function for some time due to a lagging effect. TSH may continue to be high and out of normal range, while free T3 and free T4 continue to be low. This lagging effect can last for months. However, as the adrenals recover, the patient will improve clinically, with rising body temperature returning to normal, increased energy, reduced need for thyroid medication, and improved weight management. Conventional physicians not trained to recognize this adrenal-thyroid connection are pleasantly surprised clinically to see their patients improving despite "abnormal" laboratory studies, but not knowing why. The key, of course, lies in their improved adrenal function.
 While it is important to factor in adrenal support as a primary focus in those with concurrent adrenal and thyroid dysfunction, it is important not to abruptly discontinue any thyroid medications (and other natural compounds that may have stimulatory effects such as herbs and glandulars) without professional guidance. Abrupt termination may lead to very unpleasant and intolerable withdrawal symptoms. In rare cases, adrenal crisis may be precipitated. The best clinical strategy is to focus on nurturing the adrenals and let the thyroid function improve on its own.
While it is important to factor in adrenal support as a primary focus in those with concurrent adrenal and thyroid dysfunction, it is important not to abruptly discontinue any thyroid medications (and other natural compounds that may have stimulatory effects such as herbs and glandulars) without professional guidance. Abrupt termination may lead to very unpleasant and intolerable withdrawal symptoms. In rare cases, adrenal crisis may be precipitated. The best clinical strategy is to focus on nurturing the adrenals and let the thyroid function improve on its own.
On the flip side, weak adrenals and thyroid, when present concurrently and not attended to properly, form an adverse reinforcing vicious downward spiral of dysfunction. Those who require an ever larger dose of thyroid medication to keep fatigue away may end up dependent on heavy and strong thyroid medication, but have to suffer symptoms of toxic thyroid (such as heart palpitation) as the dose is increased. They feel "wired and tired" as mentioned earlier, with constant fatigue, but are unable to fall asleep, and feel anxious throughout the day. Internally, the adrenals continue to weaken as the stimulatory properties of thyroid medications are negated by continued and overwhelming rejection by the adrenal glands, resulting in a body continuously downregulated to conserve energy. This is the worst of both worlds. It happens too frequently and goes unnoticed. Clinicians and patients alike are baffled by what seems to be clinical contradictions against improving laboratory TSH levels (as a result of increased medications) or high TSH levels that refuse to come down, the need for more thyroid medications to maintain energy, and worsening Adrenal Fatigue with continued low basal body temperature, metabolic imbalances, weight gain and increased sluggishness.
Lastly, it is important to note that regular weight loss protocols often fail when there is OAT axis imbalance due to the underlying metabolic derangement. The good news is that when this axis imbalance is resolved, natural weight loss often follows. Pushing weight loss as a top recovery priority is therefore usually a failed strategy.
 Of those taking thyroid replacement medications, 70 percent continue to complain of symptoms. Physicians often fail to take the necessary time to understand how Adrenal Fatigue can be a leading cause of secondary hypothyroidism, either clinical or sub-clinical. Relying too much on laboratory results as a gauge for thyroid replacement is very common. Thyroid function tests can remain within the normal range but the patient can still fail to improve. Physicians are misled into thinking that a higher dose of medicine may be required. In a setting of concurrent Adrenal Fatigue and hypothyroidism, this is often a failed strategy. Increased thyroid medication only serves to mask the underlying adrenal weakness. Over time, the patient continues to get worse despite ever larger doses of medicine. As the dose of thyroid medication gets larger, the patient may experience heart palpitations and anxiety. At the same time, reducing medication is a difficult option due to potential withdrawal problems.
Of those taking thyroid replacement medications, 70 percent continue to complain of symptoms. Physicians often fail to take the necessary time to understand how Adrenal Fatigue can be a leading cause of secondary hypothyroidism, either clinical or sub-clinical. Relying too much on laboratory results as a gauge for thyroid replacement is very common. Thyroid function tests can remain within the normal range but the patient can still fail to improve. Physicians are misled into thinking that a higher dose of medicine may be required. In a setting of concurrent Adrenal Fatigue and hypothyroidism, this is often a failed strategy. Increased thyroid medication only serves to mask the underlying adrenal weakness. Over time, the patient continues to get worse despite ever larger doses of medicine. As the dose of thyroid medication gets larger, the patient may experience heart palpitations and anxiety. At the same time, reducing medication is a difficult option due to potential withdrawal problems.
The following table outlines the key signs, symptoms and differences between Adrenal Fatigue and hypothyroidism.
| Characteristics | Adrenal Fatigue | Hypothyroidism |
|---|---|---|
| Weight | Early: weight gain; severe - cannot gain weight | Generalized weight gain |
| Body Temp | 97.8 or lower | Low 90s to 98.6 |
| Temperature regulation | Fluctuating and exaggerated | Steady |
| Mental Function | Brain Fog | Slow thinking |
| Depression | Sometimes | Frequent |
| Eyebrows | Full | Sparse outer 1/3 |
| Hair | Thin, sparse on extremities | Coarse and sparse |
| Hair Loss | Sometimes | Common |
| Nails | Thin, brittle | Normal to thick |
| Peri-orbital Tissue | Sunken | Puffy |
| Skin | Thin | Normal |
| Skin Tone | Dry | Oily or moist |
| Ligament Flexibility | Good | Poor |
| Fluid Retention | No | Yes |
| Pain | Headache, muscular, migraines | Joints, muscles |
| Reactivity | Heightened and hyper-reactive | Hypo-reactive |
| History of Infections | Common | Occasional |
| Chronic Fatigue | Yes | Yes |
| Orthostatic Hypotension | Frequent | No |
| Blood Sugar | Tendency toward hypoglycemia | Normal to hyperglycemia |
| Heart Palpitations | Frequent | No |
| GI Function | Irritable or hyperactive | Constipated and hypoactive |
| Malabsorption | Yes | No |
| Sensitive to Medications | Frequent | Normal |
| Personality Traits | Type A | Type A or B |
| Obsessive Compulsive | Frequent | Mixed |
| Sleep Pattern | Waking up between 2-4 am | Sleepy |
| Temperature Tolerance | Intolerance to cold | Intolerance to heat |
| Food Cravings | Cravings for sweet and salty foods | Cravings for fatty foods |
It is not unusual to present concurrent symptoms of both low adrenal and low thyroid function. In fact, this is the norm rather than the exception. Conventional medicine tends to miss this due to ignorance of Adrenal Fatigue. Those who were diagnosed with hypothyroidism after a traumatic and stressful event such as a pregnancy, accident, infection, or emotional trauma such as divorce or death of a loved one should be especially on alert if thyroid replacement alone is not helping.
Those who have poor body temperature regulation are more prone to have mixed presentation. Having symptoms of both adrenal fatigue and hypothyroidism serves to alert us that both adrenal fatigue and hypothyroid may be concurrently present. This is especially prevalent in those with OAT axis imbalance. This group of people may present a steady low body temperature from the low 90's to a little below 98.6. They may also present a slight exaggerated response to environmental temperature characterized by a sensation of feeling hot when it is warm and feeling cold when it is cool. They also suffer from fatigue, dry skin and weight gain.
Those who have mixed type presentations are the most challenging. Resolving the adrenal component should take precedence and is the key to a total healing process. Normalization of adrenal function will often lead to spontaneous and dramatic resolution of hypothyroid symptoms in such cases.
 In OAT axis imbalance, it is common that one component of the axis clinically presents itself to be more dominant and therefore more problematic. The imbalance amongst the thyroid, adrenals and ovaries is generally not equal. The clinically dominant part usually reflects the organ system that is constitutionally the weakest and thus most damaged. For example, symptoms of subclinical hypothyroidism may be more severe as compared to adrenal and ovarian dysfunction.
In OAT axis imbalance, it is common that one component of the axis clinically presents itself to be more dominant and therefore more problematic. The imbalance amongst the thyroid, adrenals and ovaries is generally not equal. The clinically dominant part usually reflects the organ system that is constitutionally the weakest and thus most damaged. For example, symptoms of subclinical hypothyroidism may be more severe as compared to adrenal and ovarian dysfunction.
Clinically, those who are thyroid dominant usually present themselves with severe low energy physically in addition to classical signs of hypothyroidism such as dry skin and inability to lose weight. Their clinical chief complaint is fatigue. They are "too fatigued" to worry about PMS or being depressed even though depression symptoms are present, for example. This is a clue to the health care provider. Unfortunately, most health professionals miss this unless they are trained in adrenal fatigue. Physicians are easily misled into thinking that the thyroid is the only problem without considering the others, leading to an incomplete diagnosis and ineffective therapy.
The adrenal dominant type usually presents with fragile emotional states such as anxiety and irritability. They are tired as well, but the fatigue is minor in comparison to the emotional roller coaster ride they experience due to easily triggered anger or rage. Finally, those who are ovarian dominant usually present themselves with significant brain fog and memory loss in addition to PMS and other estrogen dominance symptoms.
Recognizing which of the OAT axis components is dominant plays an important clinical role in designing a comprehensive recovery program because the nutritional support, dietary and lifestyle modifications are different for each. For example, the natural compound gaba is generally a good sleep aid for those who are adrenal dominant. It is, however, not as effective when compared to 5-HTP for those who are thyroid dominant. Each nutrient has its unique "best use" pathway and needs to be matched to the proper condition for maximum effectiveness.
In terms of diet, the thyroid dominant type benefits most from a vegetarian diet with increased fiber load to enhance gastric assimilation, while the ovarian type usually does better with a diet high in protein relative to carbohydrates. The adrenal dominant type usually does best on a balanced diet with bias towards more protein and fat, along with higher meal frequency to overcome hypoglycemia. Those with a mixed type require a combination of the above.
In terms of exercise, the thyroid dominant type does best with rhythmic exercises like running or swimming. The ovarian dominant type does best with more gentle and mentally focused exercises such as yoga. The adrenal dominant type is trickier, as they can be divided into two main categories, those with high adrenal function and those with low adrenal function. Strenuous exercise is often helpful for the high adrenal type to burn off the excess adrenaline.  Those with low adrenal function should often refrain from any exercise until the body regains its footing through proper nutritional and diet support. When the body's reserve increase, a gradual scaling up of isometric and isotonic exercises can be considered.
Those with low adrenal function should often refrain from any exercise until the body regains its footing through proper nutritional and diet support. When the body's reserve increase, a gradual scaling up of isometric and isotonic exercises can be considered.
Oftentimes, during the recovery process, the type of dominance can change as well. For example, one can be thyroid dominant and progresses to adrenal dominant. This can occur when thyroid function improves or if there is an acute adrenal crash that overwhelms the thyroid. Knowing which component is dominant during the recovery period allows the clinician to prioritize the recovery plan and use the proper natural support at the proper time. Common self guided or shotgun standardized approaches without careful consideration to the types of dominance and their ongoing progression often leads to delayed or failed recovery.
The ovaries, the adrenal and thyroid glands of the body form a physiologic equilateral triangle that must be in perfect balance in order for the body to function optimally. Any change in one organ system will affect the other two.
A weak ovarian system worsens adrenal function and will also weaken thyroid function, resulting in Adrenal Fatigue and hypothyroidism.
Imbalanced adrenal function compounds hypothyroidism and worsens estrogen dominance.
Hypothyroidism exacerbates adrenal weakness and blunts ovarian hormonal responses.
When the OAT axis becomes imbalanced, multiple organs are involved, and dysfunctions occur. If not attended to properly over time, the body's function is thrown into a vicious downward cycle of cascading decompensation. This is often made worse by medications and improper treatment protocols.
In addition to the major symptoms of OAT axis imbalance consisting of hypothyroidism, estrogen dominance and adrenal fatigue, other organ systems are also frequently involved, especially in more advanced stages of imbalance. For example, processing and assimilating nutrients is often compromised. Absorption of nutrients from the GI tract is reduced as leaky gut, irritable bowel, food sensitivity and internal dysbiosis overwhelm the normal flora. Liver function is reduced despite lab test results showing normal liver function. Good nutrients, if not processed and metabolized properly, become toxic. Toxic metabolites circulate in the body and if not properly cleared, can lead to brain fog, joint pain, skin rashes, allergies, muscle discomfort and multiple chemical sensitivities among many other symptoms. No organ system is spared dysfunction when this axis is not well balanced.
Women with OAT axis imbalance often find themselves consulting with various specialists who may not be mindful of the concurrent triad of ovarian, thyroid and adrenal dysfunctions. Hormonal replacement, whether natural or synthetic, is often prescribed. Those with OAT axis imbalance will often find a blunted response over time with this single focused approach. This strategy invariably leads to an often unrecognized change in the other two organs. For example, if thyroid medication is administered, it is not uncommon to see concurrent menstrual irregularities from ovarian hormones, and reduced ability to deal with stress and worsening fatigue from dysfunction of the adrenals. The physician is at a loss why recovery is blunted. Patients are discouraged and disappointed at the health professional. Ultimately, the patient gives up after ever increasing doses fail to reach therapeutic goals.
 Conventional physicians often resort to the use of anti-depressants, thyroid replacements, and ovarian hormones such as estrogen and progestin (or even natural hormones). Without careful consideration of the OAT axis imbalance, these medicines can worsen the imbalance. Many embark on a program of hormonal replacement only to find that such endeavors become ineffective over time. Symptoms of estrogen dominance or hormone imbalance symptoms like hot flashes, weight gain at the hips, water retention, and moodiness are commonly observed despite normal hormonal levels.
Conventional physicians often resort to the use of anti-depressants, thyroid replacements, and ovarian hormones such as estrogen and progestin (or even natural hormones). Without careful consideration of the OAT axis imbalance, these medicines can worsen the imbalance. Many embark on a program of hormonal replacement only to find that such endeavors become ineffective over time. Symptoms of estrogen dominance or hormone imbalance symptoms like hot flashes, weight gain at the hips, water retention, and moodiness are commonly observed despite normal hormonal levels.
In OAT axis imbalance, physicians and patients alike are often confused because the variety of symptoms span multiple organ systems with overlapping and paradoxical behaviors that defy conventional medical logic. Despite multiple referrals to specialists and extensive workups, the end result is often the same - frustrated clinicians and disappointed patients.
The abandoned patient is ultimately left to self-navigate. Due to the patient's lack of clinical experience, this is a futile effort at best. Jumping from one nutritional supplement to another without avail, this trial and error approach can invariably lead to further decompensation of all the involved organs, with frequent adverse adrenal crashes and adrenal exhaustion being the hallmark of severe and advanced OAT axis imbalance.
Any serious attempt to normalize this axis should consider adrenal recovery as the first step. Adrenal normalization should precede hormone modulation. But extra care should be taken to balance all three axes concurrently.
The adrenal glands deal with the daily stresses of life. A woman must normalize her adrenal glands in order to have total body hormonal balance. Without addressing the adrenals glands, she will continue to suffer with hormone imbalance symptoms. In fact, replacement of deficient hormones alone without addressing the overall health of the adrenal glands is a band-aid approach and often ineffective in the long run. The normalization process can begin with investigating and eliminating the stressors. Stressors are often chronic in nature and can be related to lifestyle, dietary, mental, and inflammatory causes. Women with heavy menstrual bleeding and adrenal exhaustion can normalize their adrenal functions with natural compounds to boost their internal cortisol production. Adequate sleep and proper diet along with other appropriate nutritional supplementation should be tried before considering progesterone therapy. Exogenous cortisol replacement and stimulatory nutrients (which may include various herbs and glandulars that under normal conditions are adaptogens) should only be considered as a last resort and on a temporary basis only as they may actually make the condition worse off.
The use of the proper amount of nutritional supplementation can certainly speed up the recovery process, if done properly. It is critically important to note that while there are many nutrients that can help the adrenals to recover, only a few are normally needed at any point in time, especially in OAT axis imbalance. Many use a shotgun approach of administering a battery of natural compounds but this places an extra burden on the already weak adrenals. More is not better unless the body is able to handle it. The more serious the OAT axis imbalance, the more careful the selection of nutrients need to be. One must be mindful of the frequent toxic effects that normal nutrients may exhibit in this setting along with the many paradoxical side effects which can make the condition worse off. Natural compounds including many adaptogens, herbs, pro-hormones and vitamins can often lead to undesirable addiction and withdrawal symptoms in many with severe OAT axis imbalance if used over a long time without proper supervision from a health professional.
OAT axis imbalance is a serious condition that can be very debilitating if not taken care of properly. Most self-guided recovery programs fail due to lack of experience navigating a clinical setting. Finding the right qualified physician is perhaps the single most important step. Your doctor cannot begin to help you if he or she does not have full comprehension of this intricate axis imbalance and its various clinical presentations and manifestations.  Unfortunately, not many physicians are qualified to handle OAT axis imbalance because they are simply not trained. Conventional physicians are often at a loss. Conventional medicine has yet to give proper recognition to adrenal fatigue, estrogen dominance or rT3 dominance, despite the presence of millions of sufferers with hormone imbalance symptoms closely tied to these imbalances. Physicians who are best qualified to handle this successfully invariably gain their knowledge and knowhow through extensive clinical experience after handling many such cases.
Unfortunately, not many physicians are qualified to handle OAT axis imbalance because they are simply not trained. Conventional physicians are often at a loss. Conventional medicine has yet to give proper recognition to adrenal fatigue, estrogen dominance or rT3 dominance, despite the presence of millions of sufferers with hormone imbalance symptoms closely tied to these imbalances. Physicians who are best qualified to handle this successfully invariably gain their knowledge and knowhow through extensive clinical experience after handling many such cases.
Because of multi-system involvement and the body's weak condition in those afflicted with OAT axis imbalance, the wrong recovery plan will not only fail but will make the condition worse off. This is perhaps the greatest danger for those who choose to self-navigate and expose themselves to the dangers unknowingly.
The older one gets, the higher the risk of self-navigation failure. With age, the body's reserve capacity to handle stress diminishes. It has a reduced ability to absorb and withstand the unavoidable setbacks that come from a self-navigation program errors due to the operator's inexperience. With each self-navigation mistake (often committed unknowingly or inadvertently), the body decompensates and never quite fully recovers, even though the clinical signs and symptoms may be stable. If this imbalance is allowed to continue and the body is not put on the right recovery track quickly, the clinical picture invariably gets worse and not better over time. The more advanced the imbalance, the more severe the hormone imbalance symptoms are, the harder it is to fully recover and the longer it takes. At the end, many with advanced OAT axis imbalance become physically incapacitated and emotionally crippled. They become a burden to their family and loved ones. They cannot be productive and in fact become a liability to the society at large and those around them.
Conversely, the hallmark of a physician's clinical excellence is the sufferer having a sustained gradual recovery over time without severe adverse crashes. Many have recovered fully from this state of imbalance. The body has a good self-repair system in place that works well if given the right nutrients and is carefully nurtured by the right and knowledgeable physician over time in most cases. It is not unusual to see significant improvements in a matter of weeks. The more experienced the clinician, the shorter the recovery time horizon and the faster the favorable outcome can be reached.
According to The American Thyroid Association: More than 12 percent of the U.S. population will develop a thyroid condition during their lifetime. An estimated 20 million Americans have some form of thyroid disease. Up to 60 percent of those with thyroid disease are unaware of their condition.
Yes, if the testosterone is low in women, they may have low libido. Women need testosterone like a male, but the amount is much smaller. Testosterone replacement for women can be considered, but it shouldn't be done without careful consideration as there are side effects, such as hair loss associated. Those with AFS can actually crash if they are already weak when starting testosterone therapy.
Low libido, enlarged prostate, and low energy are common signs of low testosterone. Loss of muscle mass, hair loss, and thyroid dysfunction are also common.