
 In the past 40 years, we have seen a dramatic rise in female-related illnesses never seen before in history. Today, we see the age of puberty (menarche) dropping precipitously to as low as 10 years of age, endometriosis afflicting 10% of all perimenopausal women; Premenstrual Syndrome (PMS), rising and afflicting close to 30% of perimenopausal women, uterine fibroids affecting close to 25% of women from age 35 to 50, and breast cancer afflicting close to 10% of all women. Being a woman in the 21st century is certainly a high risk profession. Navigating through this hazardous profession is not easy. Imagine having endometriosis, PMS and fibrocystic breasts when you were young, progressing to uterine fibroids, hysterectomy, misguided hormone replacement and ultimately breast cancer as your menopause approaches. The very thought of this journey can send chills up through anyone's spine. Fortunately, scientific evidence is mounting that hormone disruptions like estrogen dominance are the key cause of all these seemingly separate but related diseases.
In the past 40 years, we have seen a dramatic rise in female-related illnesses never seen before in history. Today, we see the age of puberty (menarche) dropping precipitously to as low as 10 years of age, endometriosis afflicting 10% of all perimenopausal women; Premenstrual Syndrome (PMS), rising and afflicting close to 30% of perimenopausal women, uterine fibroids affecting close to 25% of women from age 35 to 50, and breast cancer afflicting close to 10% of all women. Being a woman in the 21st century is certainly a high risk profession. Navigating through this hazardous profession is not easy. Imagine having endometriosis, PMS and fibrocystic breasts when you were young, progressing to uterine fibroids, hysterectomy, misguided hormone replacement and ultimately breast cancer as your menopause approaches. The very thought of this journey can send chills up through anyone's spine. Fortunately, scientific evidence is mounting that hormone disruptions like estrogen dominance are the key cause of all these seemingly separate but related diseases.
For too long, we have ignored the importance of hormonal balance. For too long, physicians have been misguided on the real truth about hormonal balance. Now, we know that the common thread in many female hormone diseases such as those mentioned above is a little known condition known as estrogen dominance. The underlying problem is a relative excess of estrogen and an absolute deficiency in progesterone. In the west, the prevalence of estrogen dominance syndrome approaches 50% in women over 35 years old.
Here are some typical complaints from patients having estrogen dominance:
Before we look at estrogen dominance in more detail, let us first review the basic menstrual cycle and the key female hormones.
One hundred years ago, the average woman started her menses at age 16. She got pregnant earlier and more frequently. She often spent more time lactating. In total, women back then experienced the menstrual cycle about 100 to 200 times in their lifetime. Today, the average modern women starts puberty at age 12, seldom lactates, has less children, and menstruates about 350 to 400 times during a lifetime.  Incessant menstruation has been associated with the increased occurrence of a myriad of pathological conditions including infertility, cancer, fibroids, anemia, migraines, mood shifts, abdominal pain, fluid retention, and endometriosis. What a difference a century makes!
Incessant menstruation has been associated with the increased occurrence of a myriad of pathological conditions including infertility, cancer, fibroids, anemia, migraines, mood shifts, abdominal pain, fluid retention, and endometriosis. What a difference a century makes!
It is apparent that modern woman goes through a lot more than her counterpart just a century ago. Could this have any bearing on the epidemic of female related illness plaguing our society? To answer that question, let us take a closer look at the hormones responsible for regulating the female menstrual cycle.
The two primary female hormones secreted by the ovaries are estrogen and progesterone. The properties of one offsets the other and together they are maintained in optimal balance in our body at all times. Too much of one hormone or the other can lead to significant medical problems.
Estrogen is produced in the ovaries. It regulates the menstrual cycle, promotes cell division and is largely responsible for the development of secondary female characteristics during puberty, including the growth and development of the breast and pubic hair. Estrogen therefore affects all female sexual organs, including the ovaries, cervix, fallopian tubes, vagina, and breast. As a general rule, estrogen promotes cell growth, including signaling the growth of the blood-rich tissue of the uterus during the first part of the menstrual cycle and stimulates the maturation of the egg-containing follicle in the ovary. It softens the cervix and produces the right quality of vaginal secretion to allow the sperm to swim and to lubricate during intercourse. Furthermore, it lifts our mood and gives a feeling of well-being.
In non-pregnant, pre-menopausal women, only 100-200 micrograms (mcg) of estrogen are secreted daily. However, during pregnancy, much more is secreted.
Estrogen in our body actually is not a single hormone but a trio of hormones working together. The three components of estrogen are: estrone (E1), estradiol (E2), and estriol (E3). In addition, there are at least 24 other identified types of estrogen produced in the woman's body, and more will be discovered. In healthy young women, the typical mix approximates 15/70 percent respectively. This is the combination worked out by Mother Nature as optimum for human females. Today, we use the word estrogen loosely to include also a family of hormones, including animal estrogens, synthetic estrogens, phytoestrogens (plant estrogens), and xenoestrogens (environmental estrogens, usually from toxins such as pesticides).
Estrogen is a pro-growth hormone. Since too much of anything is generally not good, the body has another hormone to offset and counterbalance the effects of estrogen. It is called progesterone.
 As its name implies, progesterone is a pro-gestation hormone. In other words, it favors the growth and well-being of the fetus. Without a proper amount of progesterone, there can be no successful pregnancy. It protects us against the "growth effect" of estrogen. When progesterone is secreted, further ovulation is prevented from taking place in the second half of the menstrual cycle, and a thick mucous that is hostile to sperm is produced that prevents its passage into the womb.
As its name implies, progesterone is a pro-gestation hormone. In other words, it favors the growth and well-being of the fetus. Without a proper amount of progesterone, there can be no successful pregnancy. It protects us against the "growth effect" of estrogen. When progesterone is secreted, further ovulation is prevented from taking place in the second half of the menstrual cycle, and a thick mucous that is hostile to sperm is produced that prevents its passage into the womb.
Progesterone is made from pregnenolone, which in turn comes from cholesterol. Production occurs at several places. In women, it is primarily made in the ovaries just before ovulation and increasing rapidly after ovulation. It is also made in the adrenal glands in both sexes and in the testes in males. In women, its level is highest during the luteal period (especially from day 19 to 22 of the menstrual cycle). If fertilization does not take place, the secretion of progesterone decreases and menstruation occurs 12 to 14 days later under normal conditions. If fertilization does occur, progesterone is secreted during pregnancy by the placenta and acts to prevent spontaneous abortion. About 20-25 mg of progesterone is produced per day during a woman's monthly cycle. Up to 300-400 mg are produced daily during pregnancy.
As mentioned earlier, progesterone acts as an antagonist to estrogen. For example, estrogen stimulates breast cysts while progesterone protects against breast cysts. Estrogen enhances salt and water retention while progesterone is a natural diuretic. Estrogen has been associated with breast and endometrial cancers, while progesterone has a cancer preventive effect. Studies have shown that pre-menopausal women deficient in progesterone had 5.4 times the risk of breast cancer compared to healthy women.
The following table clearly shows how progesterone and estrogen balance each other. It is very important to note that both hormones are necessary for optimum function. Progesterone will not work without some estrogen in the body to "prime the pump", for example.
| Estrogen Effect | Progesterone Effect |
|---|---|
| Causes endometrium to proliferate | Maintains secretory endometrium |
| Causes breast stimulation that can lead to breast cancer | Protects against fibrocystic breast and prevents breast cancer |
| Increases body fat | Helps use fat for energy |
| Increase endometrial cancer risk | Prevents endometrial cancer |
| Increase gallbladder disease risk | |
| Restrains osteoclast function slightly | Promote osteoblast function, leading to bone growth |
| Reduces vascular tone | Restores vascular tone |
| Increase blood clot risk | Normalize blood clot |
Estrogen and progesterone work in synchronization with each other as checks and balances to achieve hormonal harmony in both sexes. It is not the absolute deficiency of estrogen or progesterone but rather the relative dominance of estrogen and relative deficiency of progesterone that is the main cause of health problems when they are off balance.
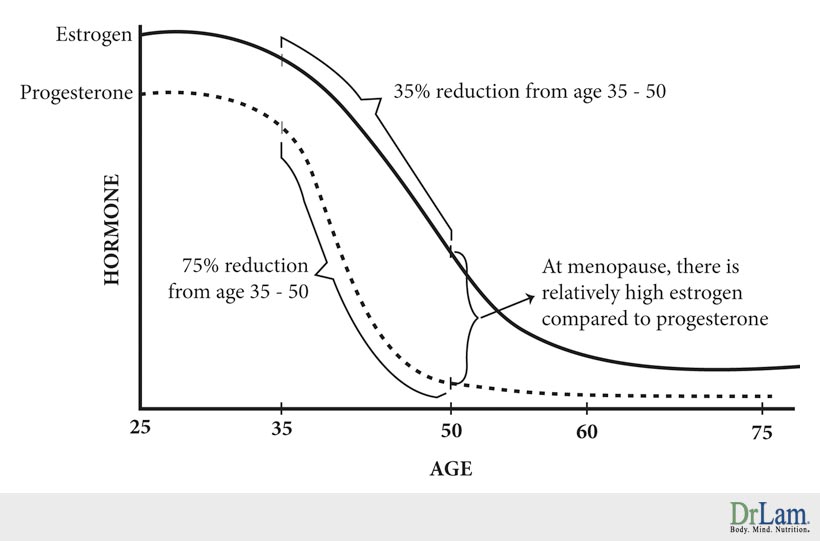
 While sex hormones such as estrogen and progesterone decline with age gradually, there is a drastic change in the rate of decline during the perimenopausal and menopausal years for women in these two hormones as mentioned earlier.
While sex hormones such as estrogen and progesterone decline with age gradually, there is a drastic change in the rate of decline during the perimenopausal and menopausal years for women in these two hormones as mentioned earlier.
From age 35 to 50, there is a 75% reduction in production of progesterone in the body. Estrogen, during the same period, only declines about 35%. By menopause, the total amount of progesterone made is extremely low, while estrogen is still present in the body at about half its pre-menopausal level.
With the gradual drop in estrogen but severe drop in progesterone, there is insufficient progesterone to counteract the amount of estrogen in our body. This state is called estrogen dominance. Many women in their mid-thirties, most women during peri-menopause (mid-forties), and essentially all women during menopause (age 50 and beyond) are overloaded with estrogen and at the same time suffering from progesterone deficiency because of the severe drop in physiological production during this period. The end result - excessive estrogen relative to progesterone, a condition we call estrogen dominance.
According to the late Dr. John Lee, the world's authority on natural hormone therapy, the key to hormonal balance is the modulation of progesterone to estrogen ratio. For optimum health, the progesterone to estrogen ratio should be between 200 and 300 to 1.
What is so bad about estrogen dominance? It is the root cause of a myriad of illnesses. Conditions associated with this include fibrocystic breast disease, PMS, uterine fibroids, breast cancer, endometriosis, infertility problems, endometrial polyps, PCOS, auto-immune disorders, low blood sugar problems, and menstrual pain, among many others.
There are two time periods in a women's life that her progesterone level is low - at puberty and again at peri-menopause (the few years right before menopause). Between puberty and peri-menopause, the production of progesterone can go astray, leading to estrogen dominance as mentioned earlier. Between this time, estrogen dominance can also be the result of excessive external estrogen intake (from diet and environment) or internal estrogen production (from obesity, birth control pills, or ovarian tumors).
Two common causes:
 If a woman were not ovulating, there would not be a corpus luteum and therefore no increased progesterone production. Laboratory measurement would show both a low estrogen and a low progesterone level. Many still have a seemingly normal menstrual cycle even if there is no ovulation. The lack of progesterone, however, leads to relative estrogen dominance and symptoms like PMS, mood swings, cramps, and tender breasts. Anovulation is commonly caused by exposure of female embryos to environmental estrogen (also called xenobiotics or xenoestrogens) such as pesticides, plastic, and pollution. This is often related to poor diet and stress.
If a woman were not ovulating, there would not be a corpus luteum and therefore no increased progesterone production. Laboratory measurement would show both a low estrogen and a low progesterone level. Many still have a seemingly normal menstrual cycle even if there is no ovulation. The lack of progesterone, however, leads to relative estrogen dominance and symptoms like PMS, mood swings, cramps, and tender breasts. Anovulation is commonly caused by exposure of female embryos to environmental estrogen (also called xenobiotics or xenoestrogens) such as pesticides, plastic, and pollution. This is often related to poor diet and stress.The predominant reason why menopausal women develop estrogen dominance is that they are being prescribed unopposed estrogen such as Premarin as part of their hormone replacement therapy (HRT) program. Despite decades of research clearly showing that HRT significantly increases breast cancer, millions of women worldwide are on unopposed estrogen for treatment of menopausal symptoms.
Obesity is another cause. During menopause, the amount of estrogen produced from the ovaries decreases, but not as drastically as another hormone the ovaries produce called androstenedione (a male hormone). Fat cells can convert androstenedione into estrogen. The amount of conversion in some people is enough to maintain a reasonable estrogen level in the body well into the 70s. The result of excessive estrogen and absolute deficiency in progesterone is clear - estrogen dominance.
We mentioned before that our body is essentially soaked in a sea of estrogen. Where does the estrogen come from? Let us take a closer look.
Our body normally functions in perfect homeostasis. With the advent of society and industrial state in the past 70 years, our body has been subjected to unprecedented insults from environmental estrogen-like hormones. In less than one hundred years, we have managed to turn our diet from whole fruits and whole foods to fast and processed food. In the past, cattle were raised on grass and natural organic feed and chickens were allowed to run free. This is in stark contrast to the commercialization of cattle and poultry farms of today where animals are in cages most of the time. Worse yet, feeds laced with pesticides and hormones, both of which have estrogen-like activities, are routinely given to animals, which in turn is passed to humans.
Women in non-industrialized cultures whose diets are whole food based and are untainted with modern processed foods and pesticides seldom suffer a deficiency in progesterone and the signs of estrogen dominance manifested as menopausal symptoms.
12 of the most common reasons:
 Commercially raised cattle and poultry. These animals arefed estrogen-like hormones as well as growth hormone that are passed onto humans. It takes 60 pounds of grain, feed, and hay to produce one pound of edible beef. On the other hand, it only takes one pound of feed to produce one pound of edible fish. Deep-sea fish such as halibut, sardine, cod, and mackerel are good to consume. Young ones are often less contaminated than older fish, and smaller fish are better shielded from contamination than larger fish like sharks and swordfish. Avoid all coastal fish and shellfish, which are high in contaminants. Fish are far superior to beef or chicken in terms of hormone load. It is interesting to note that one-half of all antibiotics in the United States are used in livestock - 25 million pounds a year. These antibiotics can contribute to hormone disruptor exposure. The use of antibiotics is especially prevalent in poultry farms. It only takes 6 weeks now to grow a chicken to full size (down from four months in 1940). Up to 80,000 birds may be packed into one warehouse. Feeds used contain a myriad of hormone-disrupting toxins including pesticides, antibiotics, and drugs to combat disease when so many animals are packed closely together.
Commercially raised cattle and poultry. These animals arefed estrogen-like hormones as well as growth hormone that are passed onto humans. It takes 60 pounds of grain, feed, and hay to produce one pound of edible beef. On the other hand, it only takes one pound of feed to produce one pound of edible fish. Deep-sea fish such as halibut, sardine, cod, and mackerel are good to consume. Young ones are often less contaminated than older fish, and smaller fish are better shielded from contamination than larger fish like sharks and swordfish. Avoid all coastal fish and shellfish, which are high in contaminants. Fish are far superior to beef or chicken in terms of hormone load. It is interesting to note that one-half of all antibiotics in the United States are used in livestock - 25 million pounds a year. These antibiotics can contribute to hormone disruptor exposure. The use of antibiotics is especially prevalent in poultry farms. It only takes 6 weeks now to grow a chicken to full size (down from four months in 1940). Up to 80,000 birds may be packed into one warehouse. Feeds used contain a myriad of hormone-disrupting toxins including pesticides, antibiotics, and drugs to combat disease when so many animals are packed closely together. Exposure to xenoestrogens. When a female embryo develops in the womb, 500,000 to 800,000 follicles are created in the embryo, each enclosing an immature ovum. These fragile ovarian follicles are extremely sensitive to the toxicity of environmental pollutants. When the mother is exposed to toxic chemicals that resemble estrogen in its molecular structure, she may experience no apparent damage outwardly. However, the baby is more vulnerable to the toxins that may damage its ovarian follicles and render them dysfunctional. This will not be apparent until the baby reaches puberty some 10 to 15 years later, when symptoms of incomplete ovulation or insufficient progesterone production can be noted. Petrochemical compounds found in general consumer products such as creams, lotions, soaps, shampoos, perfumes, hair sprays and room deodorizers. Such compounds often have chemical structures similar to estrogen and indeed act like estrogen. Other sources of xenoestrogens include car exhaust, petrochemically derived pesticides, herbicides, and fungicides; solvents and adhesives such as those found in nail polish, paint removers, and glues; dry-cleaning chemicals; practically all plastics, industrial waste such as PCBs and dioxins, synthetic estrogens from urine of women taking HRT and birth control pills that are flushed down the toilet and eventually find their way into the food chain and back into the body. They are fat soluble and non-biodegradable.
Exposure to xenoestrogens. When a female embryo develops in the womb, 500,000 to 800,000 follicles are created in the embryo, each enclosing an immature ovum. These fragile ovarian follicles are extremely sensitive to the toxicity of environmental pollutants. When the mother is exposed to toxic chemicals that resemble estrogen in its molecular structure, she may experience no apparent damage outwardly. However, the baby is more vulnerable to the toxins that may damage its ovarian follicles and render them dysfunctional. This will not be apparent until the baby reaches puberty some 10 to 15 years later, when symptoms of incomplete ovulation or insufficient progesterone production can be noted. Petrochemical compounds found in general consumer products such as creams, lotions, soaps, shampoos, perfumes, hair sprays and room deodorizers. Such compounds often have chemical structures similar to estrogen and indeed act like estrogen. Other sources of xenoestrogens include car exhaust, petrochemically derived pesticides, herbicides, and fungicides; solvents and adhesives such as those found in nail polish, paint removers, and glues; dry-cleaning chemicals; practically all plastics, industrial waste such as PCBs and dioxins, synthetic estrogens from urine of women taking HRT and birth control pills that are flushed down the toilet and eventually find their way into the food chain and back into the body. They are fat soluble and non-biodegradable. Obesity. Fat has an enzyme that converts adrenal steroids to estrogen. The higher the fat intake, the higher the conversion of fat to estrogen. Overeating is the norm in developed countries. A population from such countries, especially in the Western hemisphere where a large part of the dietary calorie is derived from fat, has a much higher incidence of menopausal symptoms. Studies have shown that estrogen and progesterone levels fell in women who switched from a typical high-fat, refined-carbohydrate diet to a low-fat, high-fiber and plant-based diet even though they did not adjust their total calorie intake. Plants contain over 5,000 known sterols that have progestogenic effects. People who eat more wholesome foods have a far lower incidence of menopausal symptoms because their pre- and post-menopause levels of estrogen do not drop as significantly.
Obesity. Fat has an enzyme that converts adrenal steroids to estrogen. The higher the fat intake, the higher the conversion of fat to estrogen. Overeating is the norm in developed countries. A population from such countries, especially in the Western hemisphere where a large part of the dietary calorie is derived from fat, has a much higher incidence of menopausal symptoms. Studies have shown that estrogen and progesterone levels fell in women who switched from a typical high-fat, refined-carbohydrate diet to a low-fat, high-fiber and plant-based diet even though they did not adjust their total calorie intake. Plants contain over 5,000 known sterols that have progestogenic effects. People who eat more wholesome foods have a far lower incidence of menopausal symptoms because their pre- and post-menopause levels of estrogen do not drop as significantly.In absolute terms, those who live in the developed world are bathed in a continuous sea of estrogen and do not know it. Yes, most of us have hormonal imbalances, and specifically - estrogen dominance.
It is clear that estrogen dominance is the underlying common denominator for a variety of illnesses and syndromes that were previously regarded as unrelated entities. They in fact represent different expressions of the same illness in different cell settings. The continuum is a state of excessive estrogen throughout one's lifetime, with different manifestations at different times.
Conditions and diseases linked to this continuum includes:

Let us now look at each of these in more detail.
Endometriosis is a very common condition. Statistics show that approximately ten to fifteen percent of women in their reproductive years from age 25 to 45 are affected. About thirty percent of affected women are infertile. It is a condition where endometrium (the lining of the uterus) is found in locations outside the uterus, such as the ovaries, fallopian tubes, vagina, abdomen, deep inside the uterine muscle, bowel, bladder, utero-sacral ligaments (ligaments that hold the uterus in place), peritoneum (covering lining of the pelvis and abdominal cavity), or other parts of the body. It can grow between organs and cause them to stick together with adhesions.
The causes of endometriosis are not yet fully known. There are quite a few theories, from genetics to toxic environment. Backward bleeding, or retrograde menstruation (when bleeding travels up into the uterus) is thought to be the leading cause. Endometrial cells are estrogen responsive, and estrogen dominance is the norm in developed society. Many researchers believe that estrogens and their close relative xenoestrogens (environmental estrogens) play a significant causative role in this disease. Some have tried to link bleached tampons with pollutant residues as the cause, but these have yet to be proven.
Risk factors for endometriosis:
Endometrial tissue responds to the same tissue as the uterus. It grows with estrogen, and may bleed during menstruation just like tissues in the uterus. The most common symptom is pain and cramps that coincide with the menstrual cycle, while scar tissue can form wherever the endometrial tissue is located and interfere with the function of the organs. Other symptoms include heavy menstrual bleeding, pain during intercourse, abdominal pain and or low back pain and diarrhea during menstruation. Sometimes there are no symptoms at all. The degree of severity of symptoms does not necessarily correlate with the degree of involvement, as each person reacts differently. Endometriosis increases risk of uterine fibroids or breast cysts, and may be accompanied by severe fatigue, chronic fatigue syndrome, or fibromyalgia.
The only way to diagnose endometriosis is by laparoscopy, a surgical procedure in which the surgeon places a small scope inside the pelvic cavity looking for endometrial tissues. This is often not successful, and a diagnosis can take years.
Surgical intervention focuses on the removal of endometrial tissues, while drug therapy focuses on balancing the hormonal picture with birth control pills. Both are not very successful. More than 500,000 surgeries are performed each year for endometriosis, and there is an upward of forty percent recurrence rate, continued pain, and disability. This disease often subsides with menopause when the estrogen level is reduced in absolute terms. It also goes away when ovaries are non-functional. This can be surgically induced by the removal of both ovaries, or chemically induced by the use of drugs on a temporary.
 In addition to menopausal symptoms commonly blamed on estrogen deficiency instead of relative estrogen dominance, researchers note that many women suffer a similar set of symptoms associated with estrogen dominance during the menstrual cycle each month. PMS can affect women soon after puberty and all the way to later years.
In addition to menopausal symptoms commonly blamed on estrogen deficiency instead of relative estrogen dominance, researchers note that many women suffer a similar set of symptoms associated with estrogen dominance during the menstrual cycle each month. PMS can affect women soon after puberty and all the way to later years.
Here are some typical complaints of patients with PMS:
This syndrome was first described in 1931. It is a well-established syndrome consisting of a host of physical and emotional symptoms that develop after ovulation and before the onset of the menstrual cycles. The syndrome can range from a few days to two weeks. The intensity can be mild (relieved by an aspirin) or it can be severe and debilitating. Generally, its symptoms intensify as the period approaches. Interestingly, ninety-five percent of PMS can be vastly improved if steps are taken to balance the body's hormones.
Dr. Katherine Dalton published the first medical report on PMS in 1953. She observed that the administration of a high dose of progesterone by rectal suppository relieved symptoms of PMS.
It is important to note that not all PMS symptoms are caused by progesterone deficiency and estrogen dominance. Hypothyroidism can produce similar symptoms. Stress leading to adrenal exhaustion and low adrenal reserve commonly seen in working mothers for example, can also cause similar symptoms. A diet low in fiber can cause estrogen to be reabsorbed and recycled. An excessive intake of xenoestrogen-laced beef and poultry also contributes to relative estrogen dominance associated with PMS. Many researchers think that PMS may be linked to xenoestrogen exposure during embryo life, damaging the ovarian follicle. Pollutant damaged ovaries, while they are in the womb, can result in infertility and chronic estrogen dominance.
The key dietary adjustments are elimination of:
In addition to regular exercise, elimination of coffee, sugar, alcohol, dairy products, and natural progesterone replacement, these steps frequently succeeded in reducing the symptoms of PMS. A diet high in phytoestrogens or supplementation of isoflavone extract or DIM, as well as nutritional supplementation with nutrients high in fatty acids such as evening primrose oil or fish oil to reduce the inflammatory response also helps. Last and most importantly, the use of natural progesterone cream should be considered.
 One of the most common reasons why women visit the gynecologist is the discovery of a breast lump. Fortunately, not all lumps are cancerous.
One of the most common reasons why women visit the gynecologist is the discovery of a breast lump. Fortunately, not all lumps are cancerous.
After a needle biopsy and workup, many of these patients are told that they suffer from benign cystic breast disease. The patient is reassured that the lumps are not cancerous for now. However, it is most important to alert these patients that such lumps are the body's cry for more progesterone. Estrogen promotes the growth and proliferation of breast cells. Breast fibrocysts are an overgrowth of these normal breast tissues. The primary causative factor is excessive estrogen. It is an early warning sign of progesterone deficiency and impending estrogen dominance.
Progesterone cream is a good remedy. Apply 20 mg of progesterone cream from ovulation (day 12 to 14) until the day or two before your period starts. Normal breast tissue will return within three to four months. In addition to reducing estrogen, supplementing with natural vitamin E (d-alpha tocopherol) and borage or evening primrose oil (omega-6) will help reduce the inflammatory response. Borage oil is preferred over evening primrose oil as it is more potent.
Scientists have also identified a chronic condition similar to PMS, which they call pre-menopause syndrome. The symptoms are similar to those of menopause, but they often occur from the mid-thirties to early forties and years ahead of menopause. This may be due to primary ovulation failure and the resultant lack of progesterone output from the ovaries. More often than not, it is due to luteal failure (failure to produce enough progesterone) in pre-menopausal women. In addition, there may also be stress induced adrenal gland exhaustion leading to a reduction of progesterone output from the adrenal glands. The overall reduction in progesterone level leads to a relative excess of estrogen or estrogen dominance. Pre-menopausal syndrome may include PMS, fibrocystic breast, uterine fibroids, irregular periods, and endometriosis.
Polycystic Ovarian Syndrome (PCOS) is a condition where multiple cysts are found on the ovaries together with other symptoms like anovulation (lack of ovulation), menstrual abnormalities, hirsutism (facial hair), male pattern baldness, acne, and often obesity. It is estimated that ten to twenty percent of women today have PCOS, and among young women, this figure could be even higher, thus qualifying PCOS as an epidemic.
PCOS takes place when the normal ovulation cycle of a woman is disrupted or stopped. This upsets the normal balance between the glands of the pituitary, hypothalamus, and ovarian axis. Under normal conditions, the hypothalamus regulates the hormone output of the ovaries and synchronizes the menstrual cycle.
PCOS happens when this cycle is disrupted due to unsuccessful ovulation. This could take place for a myriad of reasons, for example, the follicle migrates to the outside of the ovary, but does not pop the egg to release it. This follicle thus becomes a cyst and there will be no progesterone production. If for some reason these follicles are also unable to produce a mature egg that can secrete the progesterone, the menstrual cycle is dominated by increased estrogen and androgen production without progesterone. This hormonal imbalance is the main reason behind PCOS.
 These women may concurrently have different degrees of insulin resistance (Syndrome X) and therefore higher incidence of Type II diabetes, unfavorable lipid patterns (usually high triglycerides, high LDL and low HDL cholesterol), and a low bone density. Laboratory tests often show higher than normal circulating androgens, especially testosterone.
These women may concurrently have different degrees of insulin resistance (Syndrome X) and therefore higher incidence of Type II diabetes, unfavorable lipid patterns (usually high triglycerides, high LDL and low HDL cholesterol), and a low bone density. Laboratory tests often show higher than normal circulating androgens, especially testosterone.
Since standard tests usually indicate that a woman with PCOS has plenty of estrogen, and since she is still having periods, there is a danger that the doctor assumes she is still ovulating and producing plenty of progesterone.
Uterine fibroids (uterine leiomyomata) are non-cancerous tumors consisting of fibers or fibrous tissue that arise in the uterus. It is the most common tumor within the female genital tract. These growths are highly sensitive to estrogen. They develop following the onset of menstruation; enlarge during pregnancy, and decrease, often disappearing after menopause when the estrogen level decreases by half. They can be as small as a hen's egg, or commonly grow to the size of an orange or grapefruit. The largest fibroid on record weighed over 100 pounds. It afflicts many women, especially from ages 35 to 50. One in four women in the U.S. have at least some evidence of fibroids. Discovery is usually accidental, and coincidental with heavier periods, irregular bleeding, and/or irregular bleeding, or work up for endometriosis or PMS.
In cases where the tumor's size compromises other bodily functions such as compression of the bladder or excessive bleeding, surgery may be indicated. The most common surgery is hysterectomy where the uterus is removed. Many hysterectomies, however, are performed way before the patient reaches this stage. In fact, over 500,000 hysterectomies are performed every year in the US alone as mentioned earlier.
Fibrous tissues are sensitive to estrogen. The higher the estrogen, the faster the fibroid grows. While a fibroid in itself does not usually lead to cancer or become cancerous, it clearly signals a serious underlying imbalance in a woman's reproductive and hormonal system. Specifically there is an estrogen dominance and progesterone deficiency. Such imbalance does not only affect the uterus, but affects other hormone-sensitive tissues such as breast, cervix, ovaries and the vagina as well. If not taken care of, the consequences can be devastating.
The fibroid is clearly one part of a continuum of disease associated with estrogen dominance.
Breast cancer is a rampant epidemic, striking one in nine women in the U.S. Up from 1 in 30 women in 1960, before estrogen replacement therapy was popularized. The greatest surge of breast cancer diagnoses is in the western hemisphere and now spreading globally to all industrialized countries. Among women between the ages of 18 to 54, it is the most common cause of death. It is also the top cancer killer among women aged 45 to 50.
There are many forms of breast cancer. Some grow slowly, while others are much more aggressive. Ninety percent of breast cancers start in the milk glands or milk ducts, and ten percent in the fatty or connective tissue. The size of the tumor alone is not an accurate marker for virulence. About fifteen percent of all breast cancer are called in situ carcinoma. This cancer is contained entirely within a milk duct with no invasion into surrounding tissue.  Ninety-two percent of breast cancer stricken women aged 30 to 39 and forty-three percent of all breast cancer in women aged 40 to 49 has what is called ductal carcinoma in situ (DCIS). This is considered a precursor to invasive cancer. It is localized, but can be invasive. The diagnosis of DCIS has risen dramatically with the advent of mammogram, since it often presents as small calcifications on this test. Lobular carcinoma in situ (LCIS) occurs mostly in pre-menopausal women and does not form palpable mass. Its detection is therefore more difficult. About twenty-five percent of women with LCIS develop invasive breast cancer, often up to 40 years after finding the LCIS. Because of its low virulence, many oncologists think of LCIS as atypical hyperplasia (abnormal changes are found in the cells but not necessarily cancerous) with higher propensity of breast cancer. Lastly, invasive ductal and lobular breast cancers have the worst prognosis because cancer cells can spread relatively quickly. Breast cancers are usually discovered when a women feels a painless lump during a self-breast examination. Other symptoms include an area of dimpled, creased skin on the breast, vague discomfort in the breast; and indentation of the nipple.
Ninety-two percent of breast cancer stricken women aged 30 to 39 and forty-three percent of all breast cancer in women aged 40 to 49 has what is called ductal carcinoma in situ (DCIS). This is considered a precursor to invasive cancer. It is localized, but can be invasive. The diagnosis of DCIS has risen dramatically with the advent of mammogram, since it often presents as small calcifications on this test. Lobular carcinoma in situ (LCIS) occurs mostly in pre-menopausal women and does not form palpable mass. Its detection is therefore more difficult. About twenty-five percent of women with LCIS develop invasive breast cancer, often up to 40 years after finding the LCIS. Because of its low virulence, many oncologists think of LCIS as atypical hyperplasia (abnormal changes are found in the cells but not necessarily cancerous) with higher propensity of breast cancer. Lastly, invasive ductal and lobular breast cancers have the worst prognosis because cancer cells can spread relatively quickly. Breast cancers are usually discovered when a women feels a painless lump during a self-breast examination. Other symptoms include an area of dimpled, creased skin on the breast, vague discomfort in the breast; and indentation of the nipple.
FDA-approved estrogen drugs have been documented to cause cancer. Published studies have shown that women taking estrogen and a synthetic progesterone drug had a thirty-two to forty-six percent increase in their risk of breast cancer. This was based upon a large pool of data from the famous Nurses' Health Study conducted at Harvard Medical School. This study showed that the carcinogenic risk of estrogen-progestin replacement therapy became most pronounced when it was used for 10 or more years. However, recent data from the Breast Cancer Detection Demonstration Project suggest that relative risk is increased by twenty percent even after four years of use compared to no hormone treatment, and that surprisingly there was a forty percent increased risk of breast cancer using both estrogen and synthetic progesterone (called progestin) combined, compared to only twenty percent increase for estrogen alone. Clearly, the progestin (such as Provera) that is supposed to counter-balance the estrogen is not what the body recognizes as good.
The body needs natural progesterone to counter the estrogen effect. Synthetic progesterone's are far from the natural form. While some studies in fact show that estrogen does not cause cancer in the short-term, but in women taking estrogen and/or a synthetic progestin for more than 10 years, there appears to be a significantly elevated risk of breast, ovarian, and uterine cancers.
In addition to breast cancer risk, long-term estrogen replacement therapy increased the risk of fatal ovarian cancer. A large seven-year study included 240,073 pre- and post-menopausal women focuses on this. After adjusting for other risk factors, women who used estrogen for six to eight years had a forty percent higher risk of deadly ovarian tumors, while women who used estrogen drugs for 11 or more years had a startling seventy percent higher risk of dying from cancer of the ovaries.
The highest incidence of breast cancer occurs when women are in their mid-thirties to mid-forties. The peak time is about five years before menopause. During this time, levels of estrogen are still high in the body, but progesterone levels have already started, a precipitous drop. Studies have shown that by the time a lump is discovered in the breast, the tumor has been there already for about seven years. Clearly, non-genetically linked cancer is one that starts in a woman in her early thirties and is not a cancer of estrogen deficiency. This is the time when many women in industrialized nations have anovulatory cycles. As explained earlier, anovulation can be due to a variety of causes, the most important being stress and excessive xenoestrogen exposure during prenatal life. Women suffering from anovulation have reduced progesterone in their body and resulting unopposed estrogen and estrogen dominance.
Furthermore, xenoestrogens contribute to increased breast cancer risk by:
Clinicians have often reported seeing patients return with breast lumps six to twelve months after starting on HRT. This classic history reflects the effect of HRT on breast cells. Researchers have shown that estradiol increases breast cell proliferation rates by two hundred and thirty percent, while progesterone decrease it by more than four hundred percent. When estradiol is combined with progesterone, the normal proliferation rate is maintained. It is clear that unopposed estrogen (especially estradiol) is an important causative factor of breast cancer. This is well documented by numerous scientific studies. In addition, studies also show that estrogen stimulates breast cell (and breast cancer cell) hyperplasia and dysplasia whereas progesterone inhibits it. Pathologically, estradiol has been shown to stimulate and up-regulate the oncogene, Bcl-2, leading to cancer cell proliferation. Progesterone, on the other hand, up-regulates the p53 gene that increases apoptosis and blocks the Bcl-2 carcinogenic effect. It is clear that estrogen stimulates breast cancer while progesterone has the opposing effect.
Study after study has repeatedly shown that the majority of breast cancers in adult women are non-genetically linked, and upwards of eighty percent of breast cancer, is caused by estrogen dominance. Therefore, breast cancer can be cured and reversed if the body's estrogen level is bought under control. It is not a coincidence that after menopause (and reduced rate of estrogen production), the rate of increase in the risk for breast cancer drops dramatically.
We shall not dwell in depth on breast cancer here. Suffice to say that reducing estrogen aggressively forms the key foundation to prevention and treatment of breast cancer.
 Strictly speaking, all of us, men and women alike, suffer from estrogen hormone dominance. There simply is so much of it around and it is impossible to fully escape its impact. Plastics, car exhaust, meats, soaps, carpet, furniture, and paneling are just some of the examples. You may have on-and-off sinus problems, headaches, dry eyes, asthma, cold hands and feet, and may not attribute them to your exposure to xenoestrogen. Over time, the exposure can cause more chronic problems such as arthritis, and gallbladder disease.
Strictly speaking, all of us, men and women alike, suffer from estrogen hormone dominance. There simply is so much of it around and it is impossible to fully escape its impact. Plastics, car exhaust, meats, soaps, carpet, furniture, and paneling are just some of the examples. You may have on-and-off sinus problems, headaches, dry eyes, asthma, cold hands and feet, and may not attribute them to your exposure to xenoestrogen. Over time, the exposure can cause more chronic problems such as arthritis, and gallbladder disease.
While a definitive diagnosis can be made through a thorough history and physical examination, together with laboratory tests of estrogens and progesterone levels, this is seldom done. Instead, synthetic estrogen such as Premarin, or combination synthetic estrogen and synthetic progesterone (such as Pempro) are often passed out on the premise that symptoms presented are due to estrogen deficiency without any consideration for the progesterone part of the equation. In reality, many are suffering from relative estrogen dominance.
This naturally oriented protocol is designed to reduced the body's estrogen hormone load and prevent the onset of cancer. If you already have been diagnosed with cancer, more aggressive action will be needed including all these steps.
While addressing an estrogen hormone reduction protocol, it is also good to understand the role of the NeuroEndoMetabolic (NEM) Stress ResponseSM. This is how hormones, neurotransmitters, and our metabolism and detoxification all interact to keep balances in the body. When the estrogen hormone dominates, our estrogen hormone production decreases, and detoxification to clear the excess estrogen hormone increases. This all has implications in how to treat estrogen hormone dominance, which you will read about in this article. The NEM response is how the body all interacts together to maintain health. A hormone imbalance creates an imbalance in the NEM response, which causes issues with the breakdown of certain hormones, and the cleansing of hormones, specifically estrogen, from the body.
The typical domino effect of estrogen hormone dominance starts with proliferation of estrogen-sensitive cells, leading to overgrowth of endometrial lining, to PMS, to PCOS, to uterine fibroid, to hysterectomy, to severe iatrogenic (doctor-caused) hormonal imbalance (when estrogen is given alone with opposing progesterone), to misguided medication for depression and anxiety, to bone loss and reduced libido. These all can be reduced if the amount of estrogen in the body is normalized by administration of natural progesterone as a balancer.
Natural progesterone is therefore a cornerstone of estrogen hormone reduction therapy. It helps to reduce the risk of ovarian, endometrial and breast cancers, while unopposed estradiol causes that is frequently associated with fibrocystic breast disease, endometriosis, PMS, fibroids, and breast cancer. If you have symptoms of estrogen hormone dominance but have not been diagnosed with estrogen hormone-related cancer, natural progesterone will still be valuable for its cancer prevention properties. Specific dosage varies depending on the condition. Baseline saliva testing of estrogen, progesterone, and their respective ratios should be undertaken. The body normally produces 20 mg of progesterone a day. Replacement of this physiological amount in natural cream form is suggested in most cases. There is a tremendous variation in the amount that should be taken for optimum effectiveness. It is recommended that you consult a naturally oriented physician prior to treatment.
 Overeating and under-exercising are the norm in developed countries. Populations from such countries, especially in the Western hemisphere, derive a large part of their dietary calorie from fat. They also show a much higher incidence of menopausal symptoms. Studies have shown that the estrogen hormone level fell in women who switched from a typical high-fat, refined-carbohydrate diet to a low-fat, high-fiber, plant-based diet even though they did not adjust their total calorie intake. Plants contain over 5,000 known sterols that have progestogenic effects. Cultures whose eating habits are more wholesome and who exercise more have a far lower incidence of menopausal symptoms because their pre and postmenopausal levels of the estrogen hormone do not drop as significantly.
Overeating and under-exercising are the norm in developed countries. Populations from such countries, especially in the Western hemisphere, derive a large part of their dietary calorie from fat. They also show a much higher incidence of menopausal symptoms. Studies have shown that the estrogen hormone level fell in women who switched from a typical high-fat, refined-carbohydrate diet to a low-fat, high-fiber, plant-based diet even though they did not adjust their total calorie intake. Plants contain over 5,000 known sterols that have progestogenic effects. Cultures whose eating habits are more wholesome and who exercise more have a far lower incidence of menopausal symptoms because their pre and postmenopausal levels of the estrogen hormone do not drop as significantly.
In non-industrialized societies not subjected to environmental estrogen hormone insults, progesterone deficiency is rare. During menopause, sufficient progestogenic substances are circulating in the body to keep the sex drive unabated, bones strong, and passage through menopause symptom-free.
Some years back, scientists discovered that unfermented soy and various cruciferous vegetables such as broccoli, cauliflower, cabbage, kale, bok choy, and brussels sprouts contain a high level of phyto-estrogen. These compounds' chemical structure resembles the estrogen hormone but is many times weaker in potency. Women consuming these vegetables reported some relief of menopausal symptoms such as hot flashes. The prevalent wisdom is that women in menopause lack the estrogen hormone, and phyto-estrogen replenish the body with estrogen. Soy and cruciferous vegetables are heavily promoted.
It is now known that these vegetables work by competitively occupying the estrogen hormone receptor sites on the cell membrane to prevent internal estrogen from exerting its effects on the cell. Those who have an estrogen hormone dominance may therefore experience relief of symptoms as phyto-estrogen is many times weaker than the estrogen hormone in our body.
While phyto-estrogen may work and relieve symptoms, the long-term effect is probably undesirable because the estrogen hormone receptor sites are still occupied, although by the less potent phyto-estrogen. Over consumption of phyto-estrogenic food such as unfermented soy and cruciferous vegetables on a long-term basis may actually not reduce the risk of estrogen hormone dominance significantly. It's akin to replacing one potent devil with a lesser potent one. It is far more beneficial to get rid of the estrogen hormone from the receptor sites and replace them with progesterone. Estrogen load will therefore reduce significantly and the risk of estrogenic diseases such as breast cancer will be less.
Furthermore, phyto-estrogen have been shown to inhibit the conversion of T4 to the active T3 thyroid hormone, and can trigger hypothyroidism.
Women with estrogen dominance should only take unfermented soy such as tofu and cruciferous vegetables in moderation. Those with a history of thyroid imbalance should refrain from such vegetables.
A plant-based unprocessed whole-food diet is recommended. At least 15 grams of fiber should be consumed a day. Avoid high-glycemic foods such as refined sugar. Avoid alcohol or drugs that can damage the liver which will lead to an increase in estrogen due to the lack of estrogen breakdown. Caffeine intake from all sources is linked with higher estrogen hormone levels regardless of age, body mass index (BMI), caloric intake, smoking, and alcohol and cholesterol intake.
 Studies have shown that drinking more than two cups of coffee a day may increase estrogen hormone levels in women. It could also lead to problems such as endometriosis and breast pain.
Studies have shown that drinking more than two cups of coffee a day may increase estrogen hormone levels in women. It could also lead to problems such as endometriosis and breast pain.
In a clinical trial conducted, about 500 women between the ages of 36 to 45 were studied. These women were not pregnant, breastfeeding or having hormonal treatment. They were interviewed regarding their diets, smoking habits, height, and weight. Their estrogen hormone levels during the first five days of their menstrual cycle were also measured. The results showed that women who consumed more than one cup of coffee a day had significantly higher levels of estrogen during the early follicular phase of their menstrual cycle. Those who consumed at least 500 mg of caffeine daily, the equivalent of four or five cups of coffee had nearly 70% more estrogen than women who consumed less than 100 mg of caffeine daily. Coffee consumption increases estradiol levels. There are three different forms of estrogen hormone in the body - estrone, estradiol, and estriol. Estradiol is the form that is pro-cancerous.
Having high levels of estrogen for women in such cases can be detrimental as it can lead to breast cancer in women and prostate cancer in men. Those who have a family history of cancer also have a higher risk. Women should limit their intake of coffee to no more than one to two cups daily to decrease their risk of having more serious health problems. Excessive chronic coffee intake is associated also with Adrenal Fatigue and reduced progesterone production. The proper progesterone to estrogen hormone ratio is therefore not maintained, resulting in further estrogen dominance.
Coffee (especially when accompanied with sugar) also creates an acidic internal environment. The body will try to neutralize the acid by withdrawing valuable minerals such as magnesium and calcium from the bone. This leads to mineral depletion if chronic and ultimately osteoporosis.
In summary, coffee consumption can lead to increased estrogen, adrenal gland exhaustion, and osteoporosis. Clearly, coffee is not women's best friend by any means.
The liver has two mechanisms designed to help detoxify the body. They are called Phase 1 and Phase 2 detoxification pathways. Individual xenoestrogen and metabolites, once entered our body, usually follow one or both of the pathways.
In Phase one, enzymes present in the liver cell help convert toxins into metabolites through a series of chemical reactions (such as oxidation, reduction, and hydrolysis). One example of the phase one pathway involves the Cytochrome P-450 enzyme. Toxins are rendered harmless in this process and excreted through the kidneys. During this process, free radicals are often produced which, if present in excessive amounts, can damage the liver cells. Fortunately, the body has a built-in protection mechanism and antioxidants (such as vitamin C and E and natural carotenoids) can reduce the damage caused by these free radicals. If these antioxidants are lacking, the toxin exposure is too high, the toxic chemicals can become very dangerous because some of them may be converted from relatively harmless substances into potentially carcinogenic substances.
 In our polluted environment, excessive amounts of toxic chemicals such as pesticides, alcohol or medication, can disrupt the P-450 enzyme pathway by causing over activity or 'induction'. Substances that may cause overactivity (or induction) of the P- 450 enzyme pathway include caffeine, saturated fats, trans fat, paint fumes, car exhaust, cigarette smokes, and barbiturates. As a result of this induction, high levels of free radical can be produced inside the body. In order to enhance Phase 1 detoxification pathway and prevent free radical overload, a wide variety of antioxidants including ascorbic acid, lipoic acid, grape seed extract, quercetin, and N-acetyl-cysteine is needed by the body.
In our polluted environment, excessive amounts of toxic chemicals such as pesticides, alcohol or medication, can disrupt the P-450 enzyme pathway by causing over activity or 'induction'. Substances that may cause overactivity (or induction) of the P- 450 enzyme pathway include caffeine, saturated fats, trans fat, paint fumes, car exhaust, cigarette smokes, and barbiturates. As a result of this induction, high levels of free radical can be produced inside the body. In order to enhance Phase 1 detoxification pathway and prevent free radical overload, a wide variety of antioxidants including ascorbic acid, lipoic acid, grape seed extract, quercetin, and N-acetyl-cysteine is needed by the body.
In Phase two, the liver cells, in a process called conjugation, add another substance (eg. cysteine, glutathione, glucuronide, sulphur or glycine molecule) to the toxic drug or chemical which has entered the body. Once conjugated, the metabolite compound, whether it is toxic or not, is neutralized and is rendered less harmful to the body. In Phase 2, drugs, toxins, and hormones are converted into excretable substances that are in turn excreted from the body via watery fluids such as bile or urine.
Studies have shown that calcium d-glucurate, a natural ingredient found in certain vegetables and fruits can inhibit beta glucuronidase activity resulting in increased elimination of toxins from the liver. Supplements of calcium d-glucurate will enhance the glucuronidation pathway critical in the conjugation process. In addition, methionine, folic acid, taurine, N-acetyl-cysteine are very useful synergistic nutrients that will help this pathway.
Estradiol (E2) is the principal and most active estrogen circulating inside our body, and its breakdown, like many other steroidal hormones, occurs in the liver. The half-life of estradiol (E2) is about 3 hours. There are multiple pathways that convert E2 to metabolites that have widely different biological activities.
Estrone is the second most potent estrogen in circulation. It is easily converted back and forth from estradiol through enzymatic reactions. Both estrone and estradiol are metabolized by a process called hydroxylation. Some of the hydroxylated products are converted into estriol ( E3), while others are further broken down and secreted out the body. E3 is further conjugated in the liver and excreted in the urine.
Normal pre-menopausal women produce several hundred micrograms of estradiol every day. Some of this estradiol find its way to binding with the nuclei in a wide variety of tissues, resulting in genetic transcription as well as cellular division. While the production of estrogen is going on, a similar amount of estradiol is removed from the body, primarily in the liver. This on going production and destruction process results in a constant balance of estradiol in our body.
Since the metabolites are estrogen derivatives, they all possess estrogenic properties in varying degrees, as they are all part of the estrogen family. The degree of the hydroxylation (either through the two-hydroxylation or sixteen alpha-hydroxylation process) provides an indication of the metabolite's estrogenic potency.
 Metabolites such as 2-(OH)-estrone or 2-(OH)-estradiol are considered good estrogen. They are derived from hydroxylation of estrone and are the most prevalent metabolite of estradiol and estrone. These good estrogens are present in decreased level in people who are obese and in women who are on a diet high in animal fat. These good estrogens can be increased by consistent moderate exercise, a diet high in protein and low in fat, and by the consumption of food containing indol-3-carbinol such as cabbage and broccoli. In addition to being good estrogens, both 2-(OH)-estrone and 2-(OH)-estradiol have been found to be powerful antioxidants and can protect the lipid proxidation process by circulating iron molecules.
Metabolites such as 2-(OH)-estrone or 2-(OH)-estradiol are considered good estrogen. They are derived from hydroxylation of estrone and are the most prevalent metabolite of estradiol and estrone. These good estrogens are present in decreased level in people who are obese and in women who are on a diet high in animal fat. These good estrogens can be increased by consistent moderate exercise, a diet high in protein and low in fat, and by the consumption of food containing indol-3-carbinol such as cabbage and broccoli. In addition to being good estrogens, both 2-(OH)-estrone and 2-(OH)-estradiol have been found to be powerful antioxidants and can protect the lipid proxidation process by circulating iron molecules.
Another metabolite of estrone is called the 16 alpha-(OH) estrone. This is called the genotoxic form of estrogen or "bad" estrogen. It has been shown to be more potent than estradiol. Due to its ability to combine with estrogen receptors and transforming the nuclei to synthesize DNA, the risk of breast cancer is increased significantly. For this reason, it is also called the transforming estrogen. Another bad metabolite is 4-(OH)-estrone. This is a free radical generator and its role as far as being a "bad estrogen" is still under intense investigation.
It should be clear that just as there are good and bad cholesterols, we have good and bad estrogens. 2-(OH)-estrone is considered good, being a potent anti-oxidant and has anti-cancer properties 4-(OH)-estrone as well as 16-alpha-(OH)-estrone are considered bad, being free radical generators and at high level they are considered to be important indicators of cancer risk. The ideal ratio of 2-(OH)-estrone to 16-alpha-(OH)-estrone as measured in the urine is 2.0 or more.
Studies have shown that 73% of breast cancer patients have a ratio below 2.0. In other words, their 16-alpha- (OH) estrone level is high compared to the 2-(OH)-estrone. Studies have also shown that women 35 years and older with breast cancer have 2-(OH)-estrone to 16-alpha-(OH)-estrone ratio that is lower than control groups. Those women with the lowest ratio have a 30% greater chance of developing breast cancer compared to the highest 2/3. The ratio of 2-(OH)-estrone to 16-alpha-(OH)-estrone is significant and is an important predictive indicator of breast cancer risk in postmenopausal women. Fortunately, both levels can be measured in the urine.
In summary, estrogen is metabolized in the liver. Herbs that fortify the liver will speed up estrogen clearance from the body. Estrogen that is not metabolized by the liver will continue to circulate and exert it.
The most impressive research has been done on a special extract of milk thistle (Silybum marianum) known as silymarin, a group of flavonoids compounds. These compounds protect the liver from damage and enhance the detoxification process.
 Silymarin prevents damage to the liver by acting as an antioxidant. It is much more effective than vitamin E and vitamin C. Numerous research studies have demonstrated its protective effect on the liver. Extremely toxic chemicals such as carbon tetrachloride, amanita toxin, galactosamine and praseodymium nitrate produce experimental liver damage in animals. Silymarin has been shown to protect the liver against these toxins.
Silymarin prevents damage to the liver by acting as an antioxidant. It is much more effective than vitamin E and vitamin C. Numerous research studies have demonstrated its protective effect on the liver. Extremely toxic chemicals such as carbon tetrachloride, amanita toxin, galactosamine and praseodymium nitrate produce experimental liver damage in animals. Silymarin has been shown to protect the liver against these toxins.
Silymarin also works by preventing the depletion of glutathione. The higher the glutathione content, the greater the liver's capacity to detoxify harmful chemicals. Moreover, silymarin has been shown to increase the level of glutathione by up to 35 %. In human studies, silymarin has been shown to exhibit positive effects in treating liver diseases of various kinds including cirrhosis, chronic hepatitis, fatty infiltration of the liver, and inflammation of the bile duct. The common dosage for silymarin is 70 to 200 mg one to three times a day.
In addition, avoid caffeine, alcohol and medications that interfere with the liver's detoxification mechanism.
Half of the adults in Europe and 61% of American adults are overweight. If you are overweight, lose it as fat cells increase estrogen production. Aromatase is an enzyme that helps produce estrone locally within fat cells. Estrone (one of the three main estrogen in the body) in turn fools the pituitary gland into thinking, through a normal negative feedback mechanism, that there is a sufficient amount of estrogen on board. Ovaries are therefore instructed not to produce hormone. Progesterone output is thus reduced, setting up an environment of estrogen dominance. Obesity also is associated with a higher output of testosterone that in turn will cause the liver to put out more SHBG (sex hormone binding globulin). The more SHBG, the more hormones are bound are not available to the cells.
Over-consumption of calories leads to increased metabolic activity in the body. This, in turn, leads to excessive free radical formation. Free radicals damage cells and cause genetic mutations, which ultimately can lead to cancer. Cancer is more common in overweight people. The evidence on weight is strongest for post-menopausal breast cancer and cancer of the endometrium (lining of the womb), gall bladder, and kidney.
Obesity is normally defined by the body mass index or BMI, which is calculated by dividing weight in kilograms by height in meters squared. An index of between 18.5 and 25 is considered healthy, while those with a score between 25 and 29 are classified as overweight and those whose BMI is higher than that are considered obese. The target weight should be to attain ideal body weight. Your ideal body weight can be calculated easily. For women, the formula is 100 pounds plus 5 pounds for every inch above 5 feet. Therefore, for a woman standing 5 feet 6 inches tall, her ideal weight is 100 + (5 pounds/inch x 6 inches) = 130 pounds. Give or take 5 pounds for large or small frame size respectively.
 Properly performed exercises have been shown to modulate hormonal imbalance through the pre-menopausal years and beyond. Those who exercise regularly are also happier, less depressed, and have an optimistic outlook on life. This results in increased life expectancy. Statistically, life expectancy increases by two hours for every hour spent doing the proper exercises.
Properly performed exercises have been shown to modulate hormonal imbalance through the pre-menopausal years and beyond. Those who exercise regularly are also happier, less depressed, and have an optimistic outlook on life. This results in increased life expectancy. Statistically, life expectancy increases by two hours for every hour spent doing the proper exercises.
Numerous studies have confirmed that vigorous exercise can reduce breast cancer risk. Dr. Esther M. John, an epidemiologist at the Northern California Cancer Center in Union City, found that even moderate consistent exercise over a lifetime can reduce a young woman's risk of developing breast cancer by 33%, and the risk of breast cancer after menopause by 26% as compare to those who are sedentary. Moderate exercise is brisk walking 2 miles three times a week. In another study reported in the Journal Cancer, it was found that postmenopausal women who exercise 1 hour each day can significantly cut their breast cancer risk. Regardless of age, regular exercise is a proven key to reduction of breast cancer, not to mention the cardiovascular health benefits.
Precision anti-aging exercises must incorporate flexibility, cardiovascular, and strength training exercises. All it takes is 5 minutes of flexibility training every day, 20-30 minutes cardiovascular training 3 times a week, and 15-20 minutes of strength training 2 times a week. A properly structured program takes an average of 30 minutes a day, which is less than 2% of the entire day. Daily exercise can be broken down into 10-minute blocks.
Pyridoxine 50-100 mg, fish oil 200-1000 mg, natural vitamin E 90-400 I.U., Magnesium 200-800 mg, vitamin C 100-1000 mg, folic acid 100-800 mcg; quercetin 350-1,000 mg.
Diindolylmethane (DIM) 60 mg standardized extract once or twice a day-The use of DIM is compatible with other phyto-nutrients such as soy, black cohosh, red clover, and chaste berry extract. Not everyone likes vegetables, and scientists are able to isolate the active ingredient of cruciferous vegetables. It is called Indole-3-Carbinol (I3C). Unfortunately, I3C has drawbacks. Fortunately, I3C combines with stomach acid to form 3,3'-Diindolylmethane (DIM) which is safe. DIM supplementation is available. DIM is a balancer of estrogen hormone metabolism. It increases 2-hydroxyestrone (2-OHE), which is also known as the good or protective estrogen hormone. It can be used in conjunction with a phyto-estrogen such as isoflavone as well as other phyto-nutrients such as soy, red clover, and chaste berry extract in selected cases. Women who are on oral contraceptives are advised DIM is contraindicated as it might reduce the effectiveness. DIM works well together with Tamoxifen and inhibits angiogenesis. DIM also raises progesterone levels when necessary. It is interesting to note that both isoflavone and DIM work along different pathways. While studies have shown that supplementation with 200 mg per day of soy isoflavone increases the production of estrogen hormone metabolites, the effect is much less than that seen with absorbable DIM. From a nutritional supplementation perspective, 70 to 400 mg may be used.
Methionine is a valuable nutritional compound of multiple benefits to the body. In Europe, doctors have been using it with excellent results to treat depression, inflammation, liver diseases, and certain muscle pains. Methionine is an especially important nutrient beneficial to those suffering from estrogen dominance, where the amount of estrogen in the body is excessively high when compared to its opposing hormone called progesterone. Similarly, those who are on oral contraceptives or estrogen replacement therapy will find methionine to be helpful. Since estrogen is cleared through the liver, an enhanced liver function will reduce the body's estrogen load. Specifically, methionine converts the stronger and carcinogenic bad estradiol (E2) into estriol (E3) that is the good estrogen.
 The body can convert methionine into cysteine, a precursor of glutathione. Methionine therefore protects against glutathione depletion if the body is over loaded with toxins. Because glutathione is the key neutralizer of toxins in the liver, high glutathione levels protect the liver from the damaging effects of toxic compounds. Methionine is also used by the body to make a substance called choline that is essential for healthy cellular membrane function.
The body can convert methionine into cysteine, a precursor of glutathione. Methionine therefore protects against glutathione depletion if the body is over loaded with toxins. Because glutathione is the key neutralizer of toxins in the liver, high glutathione levels protect the liver from the damaging effects of toxic compounds. Methionine is also used by the body to make a substance called choline that is essential for healthy cellular membrane function.
Most people consume enough methionine from a typical diet. The daily requirement varies depending on the body weight, but approximately 100 to 1,000 mg a day is sufficient for those who are not estrogen dominant.
Most of us do not need to have methionine supplementation if we are in good health. However, strict vegetarians and anybody who follows a low protein diet should consider methionine supplementation. Those whose diet is high in soy should also consider methionine supplementation, as soy is low in amino acids. When taking methionine supplementation, intake of taurine, cysteine, and other sulfur containing amino acids, as well as folic acid should also be included.
Because of this ability to enhance estrogen clearance from the liver, methionine supplementation should be considered for anybody with symptoms of estrogen hormone dominance, including breast cancer. Excessive methionine intake in the presence of folic acid and vitamin B6 deficiency can increase the conversion of methionine to homocysteine that is linked to heart disease and strokes. Therefore it is essential that supplementation of folic acid and vitamin B6 be added as well. Supplementation of up to 4 grams of methionine daily for long periods has not been associated with any serious side effects.
Suggested Dosage: 500 mg to 4,000 mg in divided dosages throughout the day.
 Vegetarians with a low intake of protein may have difficulty producing taurine in their bodies. In addition to meat, taurine is found in abundance in shell-fish. Vegetarians as well as those on a low fat diet will have to be mindful of the amount of taurine consumed. In cells, taurine keeps potassium and magnesium inside the cell while keeping excessive sodium out. In this sense, it works like a diuretic. However, unlike prescription diuretics, it is not a cellular poison. It does not act against the kidney but improves kidney function instead. Taurine is very useful in fighting tissue swelling and fluid accumulation. People with heart failure, liver disease, late-stage ovarian cancer, and congestive heart failure frequently have unwanted fluid accumulation inside their bodies. Taurine has been very successfully used to treat people with high blood pressure. When excessive fluid in the body is normalized, the blood pressure becomes normalized. Taurine supplementation functions to dampen the sympathetic nervous system, thereby relieving arterial spasm. When the blood vessels relax, the body's blood pressure will fall.There have been studies showing the positive effectiveness of taurine on heart failure. Aside from having diuretic properties, taurine is able to strengthen the heart muscles and maintain proper calcium balance. Together with CoQ10 and carnitine, taurine is able to regulate the heart's contractility and guard against the toxic threat of chemotherapeutic drugs such as Adriamycin (doxorubicin). Working together with magnesium, taurine also is able to regulate heart rhythm and help to stabilize it.
Vegetarians with a low intake of protein may have difficulty producing taurine in their bodies. In addition to meat, taurine is found in abundance in shell-fish. Vegetarians as well as those on a low fat diet will have to be mindful of the amount of taurine consumed. In cells, taurine keeps potassium and magnesium inside the cell while keeping excessive sodium out. In this sense, it works like a diuretic. However, unlike prescription diuretics, it is not a cellular poison. It does not act against the kidney but improves kidney function instead. Taurine is very useful in fighting tissue swelling and fluid accumulation. People with heart failure, liver disease, late-stage ovarian cancer, and congestive heart failure frequently have unwanted fluid accumulation inside their bodies. Taurine has been very successfully used to treat people with high blood pressure. When excessive fluid in the body is normalized, the blood pressure becomes normalized. Taurine supplementation functions to dampen the sympathetic nervous system, thereby relieving arterial spasm. When the blood vessels relax, the body's blood pressure will fall.There have been studies showing the positive effectiveness of taurine on heart failure. Aside from having diuretic properties, taurine is able to strengthen the heart muscles and maintain proper calcium balance. Together with CoQ10 and carnitine, taurine is able to regulate the heart's contractility and guard against the toxic threat of chemotherapeutic drugs such as Adriamycin (doxorubicin). Working together with magnesium, taurine also is able to regulate heart rhythm and help to stabilize it.
Taurine is an important amino acid in the female body. The female hormone estradiol depresses the formation of taurine in the liver. Women who are on estrogen hormone replacement, birth control pills, or those suffering from excessive estrogen hormone(this is a widespread condition commonly called estrogen dominance) may need more taurine. Taurine is also helpful in clearing excessive fluid retention during menstrual periods. Furthermore, synthetic estrogen hormone replacement therapy blocks the production of taurine in the body, as well as in the case of chemotherapy and the lack of good bacteria in the intestinal tract.
Suggested Dosage: Between 1 and 3 g a day, there is usually no problem. However, at a dosage of more than 5 g a day, taurine may occasionally cause loose stools. The general dosage for people who have edema, high blood pressure, and seizure disorders range from 0.5 to 4 g a day. In high doses, taurine may increase slightly the secretion of stomach acid.
 Several theories have been proposed to explain the link between the high intake of fish oil and the low risk of cancer. Among the most important is the inhibition of ecosinoids production from AA, and omega 6. Ecosinoids belong to a class of compounds that are derived from poly and saturated fatty acids including prostaglandins, hydroxyl, prostaglandins, and leukotrienes. Prostaglandins are unsaturated fats that perform a wide variety of actions. Prostaglandin E2 (PGE2) has been linked to the formation of several types of breast and prostate cancer. Tumor cells generally produce a large amount of AA derived from PGE2. Fish oil inhibits the oxidation of AA to PGE2. Ecosinoids derived from AA is also related to the modulation of estrogen metabolism. DHA has been shown to improve the response of breast tumors to cytotoxic agents. Inflammatory molecules called leukotrienes are one of several substances that are released by mast cells during an asthma attack, and it is the leukotrienes, which are primarily responsible for the bronchoconstriction. In chronic, more severe cases of asthma, general bronchial hyperactivity (or smooth muscle twitchiness) is largely caused by eosinophils, which are attracted into the bronchioles by leukotrienes (and other chemoattractants), which also produce leukotrienes. Thus, leukotrienes seem to be critical both in the triggering of acute asthma attacks and in causing longer-term hypersensitivity of the airways in the case of chronic asthma. Leukotrienes are derived from arachidonic acid, the precursor of prostaglandins.Suggested Dosage: 500 to 10,000 mg a day
Several theories have been proposed to explain the link between the high intake of fish oil and the low risk of cancer. Among the most important is the inhibition of ecosinoids production from AA, and omega 6. Ecosinoids belong to a class of compounds that are derived from poly and saturated fatty acids including prostaglandins, hydroxyl, prostaglandins, and leukotrienes. Prostaglandins are unsaturated fats that perform a wide variety of actions. Prostaglandin E2 (PGE2) has been linked to the formation of several types of breast and prostate cancer. Tumor cells generally produce a large amount of AA derived from PGE2. Fish oil inhibits the oxidation of AA to PGE2. Ecosinoids derived from AA is also related to the modulation of estrogen metabolism. DHA has been shown to improve the response of breast tumors to cytotoxic agents. Inflammatory molecules called leukotrienes are one of several substances that are released by mast cells during an asthma attack, and it is the leukotrienes, which are primarily responsible for the bronchoconstriction. In chronic, more severe cases of asthma, general bronchial hyperactivity (or smooth muscle twitchiness) is largely caused by eosinophils, which are attracted into the bronchioles by leukotrienes (and other chemoattractants), which also produce leukotrienes. Thus, leukotrienes seem to be critical both in the triggering of acute asthma attacks and in causing longer-term hypersensitivity of the airways in the case of chronic asthma. Leukotrienes are derived from arachidonic acid, the precursor of prostaglandins.Suggested Dosage: 500 to 10,000 mg a day Silymarin prevents damage to the liver by acting as an antioxidant. It is much more effective than vitamin E and vitamin C. Numerous research studies have demonstrated its protective effect on the liver. Experimental liver damage in animals is produced by extremely toxic chemicals such as carbon tetrachloride, amanita toxin, galactosamine, and praseodymium nitrate. Silymarin has been shown to protect the liver against these toxins. Silymarin also works by preventing the depletion of glutathione the higher the glutathione content, the greater the liver's capacity to detoxify harmful chemicals. Moreover, silymarin is shown to increase the level of glutathione by up to thirty-five percent. In human studies, silymarin is shown to exhibit positive effects in treating liver diseases of various kinds including cirrhosis, chronic hepatitis, fatty infiltration of the liver, and inflammation of the bile duct. The common dosage for silymarin is 70 to 200 mg one to three times a day.Suggested Dosage: standardized milk thistle extract 200 to 800 mg a day
Silymarin prevents damage to the liver by acting as an antioxidant. It is much more effective than vitamin E and vitamin C. Numerous research studies have demonstrated its protective effect on the liver. Experimental liver damage in animals is produced by extremely toxic chemicals such as carbon tetrachloride, amanita toxin, galactosamine, and praseodymium nitrate. Silymarin has been shown to protect the liver against these toxins. Silymarin also works by preventing the depletion of glutathione the higher the glutathione content, the greater the liver's capacity to detoxify harmful chemicals. Moreover, silymarin is shown to increase the level of glutathione by up to thirty-five percent. In human studies, silymarin is shown to exhibit positive effects in treating liver diseases of various kinds including cirrhosis, chronic hepatitis, fatty infiltration of the liver, and inflammation of the bile duct. The common dosage for silymarin is 70 to 200 mg one to three times a day.Suggested Dosage: standardized milk thistle extract 200 to 800 mg a day It stimulates the immune system like reishi and maitake mushrooms, potent antioxidant and free radical scavengers, and alters the mitotic cell cycle in tumor cells and genetic expression. Most importantly, it is anti-angiogenesis and enhances apoptosis. It increases the intracellular glutathione level, thereby enhancing liver function. It acts synergistically with hyperthermia treatment protocols. Quercetin inhibits mutant P53 protein that arrests the G2 end phase of the cell cycle. Most drugs only inhibit the G1 phase. It induces apoptosis of cancer cells. It suppresses glycolysis and ATP production, interferes with ion pump systems, various signal transduction pathways, and inhibition of DNA polymerase B and I. It binds to estrogen receptor sites, working like tamoxifen and inhibits the growth of estrogen positive and estrogen negative cells. It inhibits mutant P21 genes found in over 50 percent of colon cancers which signals DNA replication in cancer cells.Vitamin C enhances the effectiveness of quercetin, and vice-versa. One caution is that tangeretin, a flavonoid found in citrus fruits, completely blocked the inhibitory effect of tamoxifen on mammary cancer in mice. Another study also shows that tamoxifen and genistein synergistically inhibit the growth of estrogen receptor-negative breast cancer cells. Until more confirmatory studies are conducted and the flavonoid-tamoxifen interactions more thoroughly investigated, it is best to avoid high therapeutic (over 1,500 mg) doses of flavonoid compounds in breast cancer treated with tamoxifen. Low remission and preventive doses (350 to 1,500 mg) are acceptable and helps to reduce estrogen-sensitive receptors.Suggested Dosage: 350 mg to 3,000 mg a day
It stimulates the immune system like reishi and maitake mushrooms, potent antioxidant and free radical scavengers, and alters the mitotic cell cycle in tumor cells and genetic expression. Most importantly, it is anti-angiogenesis and enhances apoptosis. It increases the intracellular glutathione level, thereby enhancing liver function. It acts synergistically with hyperthermia treatment protocols. Quercetin inhibits mutant P53 protein that arrests the G2 end phase of the cell cycle. Most drugs only inhibit the G1 phase. It induces apoptosis of cancer cells. It suppresses glycolysis and ATP production, interferes with ion pump systems, various signal transduction pathways, and inhibition of DNA polymerase B and I. It binds to estrogen receptor sites, working like tamoxifen and inhibits the growth of estrogen positive and estrogen negative cells. It inhibits mutant P21 genes found in over 50 percent of colon cancers which signals DNA replication in cancer cells.Vitamin C enhances the effectiveness of quercetin, and vice-versa. One caution is that tangeretin, a flavonoid found in citrus fruits, completely blocked the inhibitory effect of tamoxifen on mammary cancer in mice. Another study also shows that tamoxifen and genistein synergistically inhibit the growth of estrogen receptor-negative breast cancer cells. Until more confirmatory studies are conducted and the flavonoid-tamoxifen interactions more thoroughly investigated, it is best to avoid high therapeutic (over 1,500 mg) doses of flavonoid compounds in breast cancer treated with tamoxifen. Low remission and preventive doses (350 to 1,500 mg) are acceptable and helps to reduce estrogen-sensitive receptors.Suggested Dosage: 350 mg to 3,000 mg a day Grape Seed Extract: In 1951, a French researcher named Dr. Jacques Masquelier patented the process of extracting proanthocyanidins from the bark of the European coastal pine tree. The extracted proanthocyanidins, which are powerful antioxidant nutrients from the bioflavonoid family of compounds, were named Pycnogenol® (pronounced Pick-nah-geh-nol).The name pycnogenol can refer to two things. Besides Dr. Masquelier's trademarked compound, Pycnogenol® is also the name of a variety of compounds that contain proanthocyanidins (the active ingredient in Pycnogenol). These compounds can be derived from a variety of natural sources, such as grape seeds, which contain a high concentration of these substances.The extracted proanthocyanidins (PCO) functions the same way as vitamins C and E. By scavenging free radicals, it can help to fortify Phase I of the liver detoxification pathway, resulting in an increase of estrogen clearance. With less estrogen, heavy menstrual bleed can be normalized.What makes PCO so effective? Firstly, it is rapidly absorbed due to its excellent water solubility and distributed throughout the body within twenty minutes. It can be retained for as long as 72 hours while it neutralizes free radicals and prevents oxidation. It also works synergistically with other antioxidants like vitamin C, quercetin, and lipoic acid, thereby enhancing their effects. The results usually noted are delayed signs of aging, improved circulation as well as a stronger immune system. PCO also arms the human body with excellent antioxidant nutritional support for a variety of body repairs. It makes capillaries less susceptible to fragility and rupture; consequently, PCO is useful in blood vessel related conditions like varicose veins, peripheral hemorrhage, diabetic retinopathy, and high blood pressure.
Grape Seed Extract: In 1951, a French researcher named Dr. Jacques Masquelier patented the process of extracting proanthocyanidins from the bark of the European coastal pine tree. The extracted proanthocyanidins, which are powerful antioxidant nutrients from the bioflavonoid family of compounds, were named Pycnogenol® (pronounced Pick-nah-geh-nol).The name pycnogenol can refer to two things. Besides Dr. Masquelier's trademarked compound, Pycnogenol® is also the name of a variety of compounds that contain proanthocyanidins (the active ingredient in Pycnogenol). These compounds can be derived from a variety of natural sources, such as grape seeds, which contain a high concentration of these substances.The extracted proanthocyanidins (PCO) functions the same way as vitamins C and E. By scavenging free radicals, it can help to fortify Phase I of the liver detoxification pathway, resulting in an increase of estrogen clearance. With less estrogen, heavy menstrual bleed can be normalized.What makes PCO so effective? Firstly, it is rapidly absorbed due to its excellent water solubility and distributed throughout the body within twenty minutes. It can be retained for as long as 72 hours while it neutralizes free radicals and prevents oxidation. It also works synergistically with other antioxidants like vitamin C, quercetin, and lipoic acid, thereby enhancing their effects. The results usually noted are delayed signs of aging, improved circulation as well as a stronger immune system. PCO also arms the human body with excellent antioxidant nutritional support for a variety of body repairs. It makes capillaries less susceptible to fragility and rupture; consequently, PCO is useful in blood vessel related conditions like varicose veins, peripheral hemorrhage, diabetic retinopathy, and high blood pressure.
Compared to other nutrients normally prescribed for the above conditions, PCO demonstrated a threefold improvement of their damaged capillaries. PCO works by inhibiting the release of unwanted collagenases, which breaks down proteins. Whenever there is tissue damage and/or inflammation, these collagenases are released, thus causing the decay of the fragile capillary walls. Proanthocyanidins strengthen our capillary walls, making them valuable for circulatory disorders of all kinds, including varicose veins, hardening of arteries, and impaired blood flow to the brain.
Nineteen years after Dr Masquelier patented the process, proanthocyanidins were also extracted from grape seeds. The Pycnogenol® bioflavonoid concentration is eighty-five percent while that of grape seeds' stands higher at ninety-two percent to ninety-five percent. The cost of the grape seed extract is also much less expensive.
Some people have replaced their vitamins supplements totally with Pycnogenol®, thinking that it offers better protection. This is an incorrect assumption. It should be understood that any compounds with proanthocyanidins couldn't take the place of the other vitamins. PCOs work together with vitamins to increase the overall effectiveness of each other. In other words, PCOs should be taken in addition to and not in place of common well-researched and established antioxidants such as vitamin C and E. For practical purposes, the small difference in bioflavonoid concentration between Pycnogenol® and grape seed extract is insignificant for the same dosage. Based on cost factors, however, grape seed extract is usually recommended.
Suggested Dosage: 100 to 1,000 mg a day
Significantly, higher dosages are needed for specific problems. To limit heavy menstrual flow, up to 3,000 mg a day may be required. Therapeutic effects can be seen as early as one month, with menstrual flow reduced from 7 to 4 days.
Gamma-aminobutyric acid (GABA) for emotional stability at 250 to 2,000 mg; taurine for excessive fluid accumulation at 300 to 3,000 mg; chromium polynicotinate to help control sugar cravings at 100 to 800 mcg; Glutamine to enhance energy and gastric function at 300-3,000 mg a day.
Avoid Iron unless you are anemic.
Avoid copper unless advised by a health care professional.
Last but not least, external estrogen load is a key component that should inspire everyone to:

The adrenal gland is where stress is expressed. Chronic stress leading to Adrenal Fatigue is a leading cause of progesterone depletion and thus estrogen dominance. Balancing excessive estrogen requires taking into consideration steps to reduce and remove stressors which compromise adrenal function. Many women with estrogen dominance will see their symptoms improve by simply optimizing the adrenal gland function for the simple reasons that a properly functioning adrenal gland will put out the necessary progesterone needed to balance any excessive estrogen.
Pregnenolone and DHEA are precursors of progesterone, estrogen, and androgen. Fortification of the adrenal function with these two hormones is particularly effective in reducing Adrenal Fatigue, together with identification and removal of stressors. This is especially true if there are signs of chronic stress response.
 Vivian is a 46-year-old mother of two. She has a history of mild PMS. For the past year prior to her consultation, she began having heavy periods as well as urinary urgency. She would go to the bathroom more frequently. A qualified gynecologist saw her and complete investigation followed. Ultrasound study of her uterus showed the presence of two uterine fibroids (4.2 x 5.7 x 4.9 cm, and 2 x 1.8 cm respectively). This is the cause of her frequent bathroom visits, compression of fibroids on her bladder. Her surgeon recommended a total hysterectomy with removal of ovaries. This is the standard conventional treatment. She wants to avoid surgery if possible. She knew she was suffering from estrogen dominance but was not sure how to properly proceed for the maximum result in a short time frame.
Vivian is a 46-year-old mother of two. She has a history of mild PMS. For the past year prior to her consultation, she began having heavy periods as well as urinary urgency. She would go to the bathroom more frequently. A qualified gynecologist saw her and complete investigation followed. Ultrasound study of her uterus showed the presence of two uterine fibroids (4.2 x 5.7 x 4.9 cm, and 2 x 1.8 cm respectively). This is the cause of her frequent bathroom visits, compression of fibroids on her bladder. Her surgeon recommended a total hysterectomy with removal of ovaries. This is the standard conventional treatment. She wants to avoid surgery if possible. She knew she was suffering from estrogen dominance but was not sure how to properly proceed for the maximum result in a short time frame.
Vivian consulted with me to plan a strategy that could help her reduce the fibroids naturally. After discussing various options, both natural and conventional, Vivian decided to try the natural way. She began a personalized estrogen hormone reduction program. A complete personalized nutritional cocktail was prepared for her to help reduce her internal estrogen load. Lifestyle and dietary changes were implemented. The correct amount of natural progesterone cream was administered and adjusted over time. Vivian stayed on the program faithfully. She had a repeat ultrasound done six months later. The results were astounding. The larger fibroid has shrunk by twenty-five percent. It measures 4.6 x 4.4 x 3.3 cm. The smaller fibroid has shrunk by fifty percent. It measures only 1.6 x 0.8 cm. Vivian's urinary urgency due to the compression of the fibroids on the bladder has subsided.
This is just one of many examples of cases showing how a good estrogen reduction program can effectively control and often, reverse uterine fibroid growth. Embarking on a properly tailored estrogen reduction program should be considered for anyone suffering from estrogen dominance. There is no downside and everything to gain. Surgical intervention should be considered only as a last resort.
Estrogen Dominance is the result of excessive estrogen and progesterone deficiency. It affects about fifty percent of Western women. It is an epidemic of gigantic proportion. The primary causes are excessive environmental estrogen, obesity, stress, poor diet, lack of exercise, and unopposed estrogen hormone given as part of a hormone replacement therapy. Estrogen dominance is a major root cause of a myriad of conditions including PMS, endometriosis, cystic breast disease, PCOS, uterine fibroids, and breast cancer. Fortunately, the level of estrogen in our body can be reduced. Following an estrogen hormone reduction protocol will go a long way to reduce the amount of estrogen in the body, curing women from the dreaded illness mentioned above.
In females, a large part of the hormonal balance is controlled by three major glands: adrenal, thyroid, and ovaries. Maintaining a proper balance among these three glands is of critical importance in any estrogen hormone dominance recovery program. Excessive estrogen affects both thyroid and adrenal function, and in turn, dysfunctional thyroid and Adrenal Fatigue makes estrogen dominance worse. They all go hand in hand. When not functioning properly, these three glands, controlling the majority of hormones in the body, can lead to a vicious downward cycle of hormonal imbalance. Worse yet is that conventional medicine often misleads us into treating symptom after symptom without addressing the root cause. A wide variety of prescriptions from sleeping pills to anti-depressants is dispensed. Unfortunately, such symptom-based protocols will often make matters worse instead of better.
As a result, many following the advice of well-trained but misguided doctors may not find relief with conventional medicine or even with natural compounds unless special attention is paid to the thyroid and adrenal glands proper functioning during recovery. Any attempt to overcome one without paying attention to the other will more likely than not result in failure and discouragement for the physician and the patient. The key is to find a qualified naturally oriented physician who is experienced in all aspects of hormonal balancing. A knowledgeable physician can tell which part of the hormonal system is imbalanced with a detailed history. Laboratory tests are seldom necessary in the hands of a good clinician.
The menstrual cycle is like a fine-tuned symphony, a fascinating interplay of hormones and physiological responses played out in the orchestra of our magnificent body. Mother nature prepares you for a potential pregnancy every cycle, whether or not you want to actually conceive. Let us take a tour of the normal 28-day cycle known as the menstrual cycle.
 Day 1 of your cycle is defined as the first full day of menstrual bleeding. The uterine lining built up from the immediate preceding cycle is sloughed off and cleared away. Hormone levels from the previous cycle take a sharp decline. The result is a myriad of physical and emotional symptoms commonly associated with menstruation.
Day 1 of your cycle is defined as the first full day of menstrual bleeding. The uterine lining built up from the immediate preceding cycle is sloughed off and cleared away. Hormone levels from the previous cycle take a sharp decline. The result is a myriad of physical and emotional symptoms commonly associated with menstruation.
The menstrual bleeding usually lasts a few days. From Day 2 on, the body is already starting to prepare itself for the next cycle. Under the influence of the follicle stimulating hormone (FSH) and the luteinizing hormone (LH) from the pituitary gland, the ovarian follicle starts to manufacture and secrete estrogen. Estrogen causes the uterine lining to grow. About 15 to 20 eggs start to mature in each ovary during this period. Each egg is encased and protected in its own follicle. The follicles also produce estrogen, the hormone necessary for ovulation to eventually occur. The level of estrogen slowly rises during this period as the uterus lining thickens and starts its preparation to receive the egg if ovulation occurs. A race progresses for one follicle to become the largest. Eventually, ovulation occurs when one ovary releases an egg from the most dominant follicle.
Although it averages about two weeks, this race to release an egg can take anywhere from about eight days to a month or longer to complete. The key factor that determines how long it will take before you ovulate is how soon your body reaches its estrogen threshold. The high levels of estrogen will trigger an abrupt surge of LH. It's this LH surge, which causes the egg to literally burst through the ovarian wall, usually within a day or so of the occurrence that we called ovulation. After ovulation, the egg tumbles out into the pelvic cavity, where it is quickly transported into the fallopian tubes. The remainder of the ruptured follicle (called the corpus luteum) recedes back to the ovary and begins an important task of secreting progesterone. Why is progesterone so important? It causes an increase in blood vessels to the uterine lining in order to provide nutrients for the fetus in case fertilization occurs. It also inhibits other eggs from developing and causes the Basal Body Temperature (BBT) to rise about half a degree.
The luteal phase is the time (usually 11 to 14 days) following ovulation. In simple terms, it is the last two weeks of the menstrual cycle.
The egg can be fertilized within 24 hours of release, while it is still in the fallopian tubes. If the egg is fertilized, the pituitary gland produces human chorionic gonadotrophin (hCG), which causes the increased production of progesterone. The progesterone level reaches its peak on days 19 to 22, after which the level starts to fall if no fertilization takes place. The progesterone in turn causes the BBT to remain high throughout the luteal phase and after the 14th day. High progesterone levels are also responsible for morning sickness.
If the egg is not fertilized within 24 hours, the corpus luteum regresses and slows its progesterone production. After reaching peak production on days 19 through 22, the progesterone level starts its decline. Without progesterone's support of the rich uterine lining, menstruation starts as the slough begins and the uterus clears itself and prepares once more for the next cycle.
From the beginning of menstruation counting forward to ovulation can vary tremendously from 8 to 14 days. However, the time from start of menses, counting backward, to ovulation of the previous month is quite consistent at 14 days. This can be significant for those who have irregular cycles and are trying to determine when ovulation is taking place each month.
This menstrual cycle occurs on a monthly basis from onset of menses at age 12 or thereabouts. The exact number of days varies from person to person. In general, the menstrual cycle lasts anywhere from 28 to 35 days. It is usually only interrupted by pregnancy.
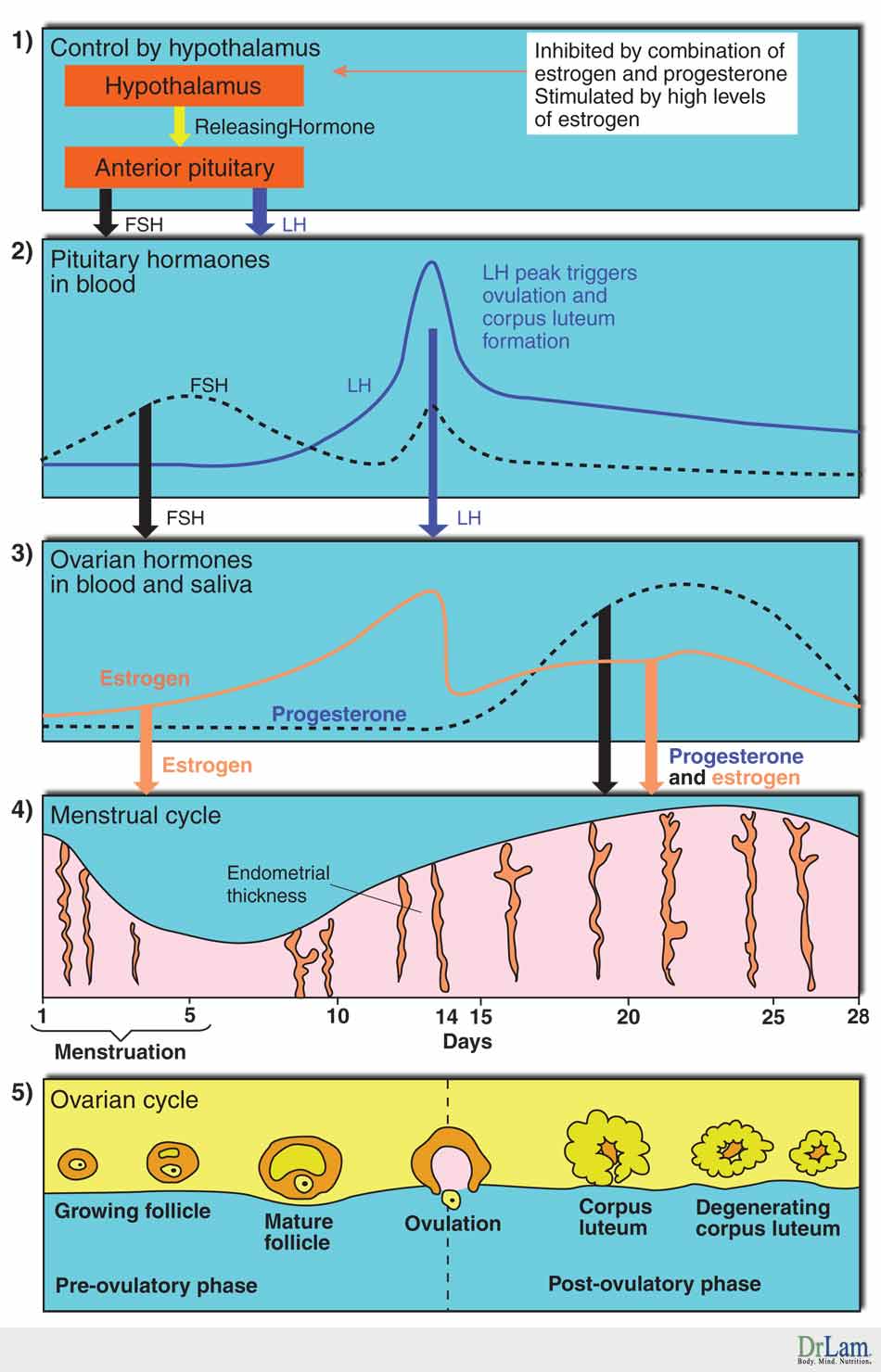
Peri-menopause is a transitional stage of two to 10 years before the complete cessation of the menstrual period (and thus, onset of menopause). Its average duration is six years and can appear in women from 35 to 50 years of age. Peri-menopause is caused by the declining function of the ovaries, although women are still menstruating. A woman can find she experiences puzzling changes, and not know why. What is actually going on is a steep decrease of progesterone with a gradual decrease in estrogen. The manifestations of peri-menopause can vary greatly.
Some of the common symptoms include:
No two women will experience peri-menopause in the same way. Unfortunately, this is a time when attention to hormonal balance is overlooked. Women are told that there is little they can do to avert many of the same symptoms that often occur during menopause. It is also a critical time for women as it represents the last window of opportunity for hormonal balancing before the dawning of menopause.
The onset of menopause signals the ending of a woman's reproductive cycle. Menopause actually begins after the women's last period, at an average age of 50. This event marks the culmination of many years of pre- and peri-menopausal changes during which hormones secreted by the ovaries estrogen and progesterone decline.
The timing of the average menopause is linked to a number of factors. Smokers, those who are nutritionally depleted, those who do not have children, and those who had their uterus removed without the removal of ovaries tend to have an earlier menopause by up to two years or more due to reduced estrogen hormone output from the ovaries.
Women who are obese or suffer from PMS or fibroids tend to have a later menopause because of excessive estrogen.
Menopausal symptoms vary considerably from person to person. Asians are known to have few to no symptoms other than irregular menses. Western women, however, have much higher incidences of body changes such as hot flashes, night sweats, fatigue, thinning of hair, insomnia, breakthrough bleeding, breast tenderness, vaginal dryness, food allergies, indigestion, reduced libido, forgetfulness, heart palpitations, loss of bladder control, frequent urination, night sweats, painful intercourse, and joint pains, to name a few. Changes in metabolism may lead to osteoporosis, a rise in blood pressure, increased fats in the blood, atherosclerosis, and increased risk of stroke. Changes in emotion can result in depression, anxiety, and irritability. The average woman gains eight pounds in the first two years of her living hell.
Typically, menopause is diagnosed when women have the following:
 A pelvic ultrasound will typically show a thin endometrium (lining of the uterus) and small ovaries that may be atrophied.
A pelvic ultrasound will typically show a thin endometrium (lining of the uterus) and small ovaries that may be atrophied.
Menopause usually progresses through three stages that last about 10 years. The first few years signifies onset of menopause. These years are the most problematic.
For the past 40 years, the conventional wisdom is that menopause is caused by the absolute deficiency of estrogen. Estrogen hormone replacement has been prescribed to millions of women since the mid 1960s. This explanation has now been shown to be an incomplete answer. Many women who cannot be prescribed estrogen hormone found relief if given natural progesterone alone. Clearly, there is more to the menopausal picture than deficiency of estrogen alone. Let us now look more deeply into female hormones.
Pregnancy is a traumatic event as far as the body is concerned. Fortunately, the body tends to release more hormones to stabilize itself during this process. Those in mild AFS tend to feel wonderful as a result during pregnancy. Those in advanced AFS will fare much worse. From worsening fatigue to miscarriages. Everyone is different.
The underlying issues of women having high testosterone could be much fold, such as AFS, OAT axis imbalance, stress, lifestyle, overexercise. So the underlying problems need to be addressed before your body will be able to self-adjust and balance the testosterone.
Breastfeeding can be very stressful on the mother because you are feeding another person and have to keep a schedule 24/7.
An elevated PE ratio means the body has more progesterone relative to estrogen. The normal targeted ratio is 200.
Either too much or too little estrogen can cause hot flashes. There are underlying issues that cause such imbalance, such as AFS, OAT axis imbalance, stress, lifestyle.
Soy products, cruciferous vegetables, flax seeds, garbanzos, etc. could be food that are phytoestrogen, therefore may affect the increase of estrogen.