 What are andropause symptoms? What do andropause symptoms look like? How can andropause symptoms affect your life? Keep reading to have these questions and more answered about you potential andropause symptoms. Andropause a.k.a "Midlife crisis" — this is often the transitional period for men when they experience what is termed as the "second childhood." This period usually starts from age 40 to 45. It is also called andropause or male menopause because its symptoms coincide with the decrease in a class of male hormones called androgen. All men are affected, although some to a larger degree than others. A thorough knowledge of the underlying hormonal and physiological changes of andropause symptoms will better prepare all males to deal with this phase of life. You can regulate and moderate your andropause symptoms.
What are andropause symptoms? What do andropause symptoms look like? How can andropause symptoms affect your life? Keep reading to have these questions and more answered about you potential andropause symptoms. Andropause a.k.a "Midlife crisis" — this is often the transitional period for men when they experience what is termed as the "second childhood." This period usually starts from age 40 to 45. It is also called andropause or male menopause because its symptoms coincide with the decrease in a class of male hormones called androgen. All men are affected, although some to a larger degree than others. A thorough knowledge of the underlying hormonal and physiological changes of andropause symptoms will better prepare all males to deal with this phase of life. You can regulate and moderate your andropause symptoms.
The male reproductive regulatory system consists of four components and these components are affected by andropause symptoms:
The master control starts in the hypothalamus where gonadotropin-releasing hormone (GnRH) is synthesized and is released in a pulsatile fashion into a vascular network that connects the hypothalamus to the pituitary gland. GnRH production and release is controlled by numerous neurotransmitters, including norepinephrine, dopamine, and endorphins. GnRH regulates the release of two pituitary hormones — the gonadotropins — luteinizing hormone (LH) and follicle-stimulating hormone (FSH) in a pulsitile fashion. LH regulates the production and secretion of testosterone by the Leydig cells of the testes, and FSH stimulates spermatogenesis. Keep reading to learn the impact of andropause symptoms.
Testosterone circulates in the blood in several forms. It can be bound to both albumin and sex hormone-binding globulin (SHBG) where it is referred to as "bound testosterone." This is the least active form. It can also circulate in a free (unbound) form, which is considered the most active.
Testosterone can exert its effects directly on the testosterone receptors in cells. It can also be converted to two active metabolites — dihydrotestosterone (DHT) through the enzyme 5 alpha reductase, or by the enzyme aromatase to estradiol.
So what andropause symptoms should you look for? What types of andropause symptoms should you worry about? Testosterone, together with its metabolites, is collectively known as androgens. As a group of steroid hormones, they stimulate the development of masculine characteristics and are responsible for male puberty characterized by deepening voice, broadening shoulders, and mustache growth. The hallmark of andropause is declining testosterone levels.
Testosterone levels begin to decline with age after maturation. This is accompanied by the concurrent appearance of a myriad of related physiological changes commonly associated with aging. These changes result in andropause symptoms including diminished libido, reduced frequency of sex (the "senior slump"), erectile dysfunction, infertility, changes in body composition, reductions in body and facial hair, and osteoporosis. Andropause is in effect the reverse of puberty, and the andropause symptoms mimic opposit physical responses.
In addition, mood inventory scores and andropause symptoms indicate that during andropause, men report levels of anger, confusion, depression, and fatigue that are significantly higher than those reported by men with normal testosterone levels. The average human male begins to feel some symptoms of andropause after 40 to 45 years old, which is followed by rapid deterioration after the age of 50.
Many of the andropause symptoms and the aging processes in men are similar to those of hypogonadism. We can attribute at least some of these symptoms to a decrease in testosterone levels, including:

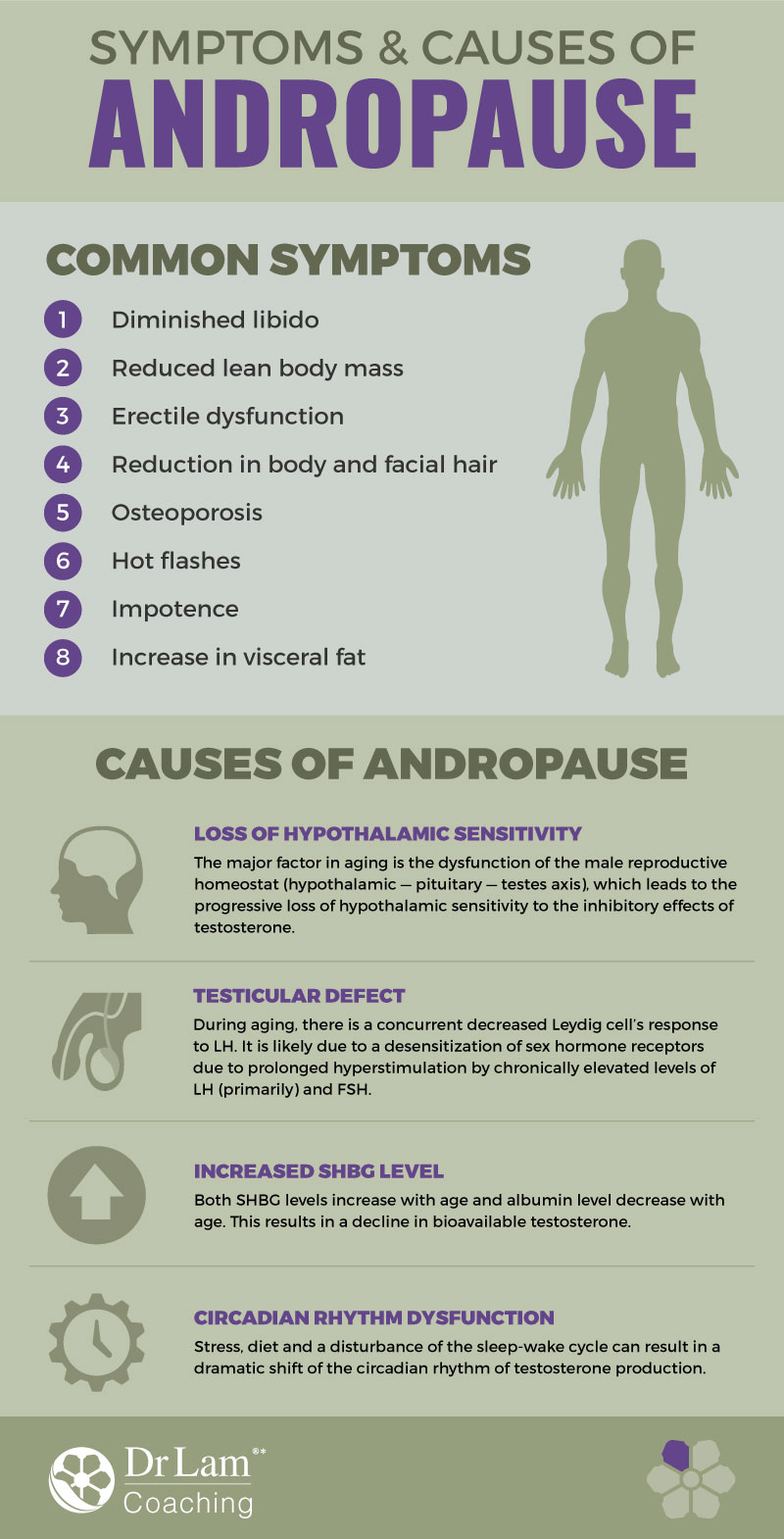
Aging males, like hypo-gonadal men, accumulate preferentially visceral fat as one of many andropause symptoms. This accumulation is a major cause of insulin resistance and the atherogenic lipid profile. This suggests that obesity in elderly men is a more important health hazard than in young men. Contrary to popular belief, clinical trials have shown that a low androgen status increases the risk of coronary artery disease (CAD) or atherosclerosis. It was previously believed that testosterone and other androgens had the opposite effect since men have higher rates of heart disease generally than women. Researchers now find that low androgen levels were associated with an increased incidence of CAD. Men with CAD had a 22 percent lower 'free androgen index'.
In relation to andropause symptoms decreased free and total testosterone levels can lead to increased fat mass, it could also be suggested that the decrease in testosterone levels in the aging male is the consequence of an increase in fat mass. In other words, there is a likely bi-directional relationship, the exact mechanism of which is still not fully known. Obesity is a multi-factorial disease that also includes genetic, social and psychological factors.
Two factors may contribute to accelerated hypogonadism in aging men and an increase in andropause symptoms. The first is a slightly decreased production of testosterone and the second is an increase in the circulating fraction of testosterone bound to SHBG.
Semen analysis in elderly men revealed an alteration in sperm counts in varying degrees from normal to increased or a decreased sperm motility and increase in abnormal sperm forms. This finding in older men suggests some degree of primary testicular failure.
However, after controlling for age, the correlation between serum testosterone levels and sexual activity was not significant. This suggests that reduced testosterone levels are not likely to be responsible for sexual dysfunction and hypogonadism in and of itself is an uncommon cause of impotence in elderly male. These types of andropause symptoms can be very hard on relationships.
 Based on these findings concerning andropause symptoms, the supplementation of testosterone in older men to improve erectile function may be of little benefit. Nevertheless, studies have also shown that aging men with high sexual activity levels have greater plasma testosterone concentrations than men with less sexual activity. Although decreases in serum testosterone may have a correlation with the diminished sexual activity in older men, this effect is probably minor compared with the contributions of psychological, social and other health factors such as cardiovascular diseases. Indeed, the question of whether or not to use testosterone as a replacement strategy in andropause use is not clear-cut. While andropause symptoms can be intense, so can the affects of hormone therapy.
Based on these findings concerning andropause symptoms, the supplementation of testosterone in older men to improve erectile function may be of little benefit. Nevertheless, studies have also shown that aging men with high sexual activity levels have greater plasma testosterone concentrations than men with less sexual activity. Although decreases in serum testosterone may have a correlation with the diminished sexual activity in older men, this effect is probably minor compared with the contributions of psychological, social and other health factors such as cardiovascular diseases. Indeed, the question of whether or not to use testosterone as a replacement strategy in andropause use is not clear-cut. While andropause symptoms can be intense, so can the affects of hormone therapy.
In studying andropause symptoms, it has been found that the vast majority of men do not experience a total loss of testosterone production compared to the total loss of estrogen that occurs in women in menopause. As a result, they do not generally experience hot flashes. Hot flashes in men mostly occur when there is a complete loss of testosterone such as during gonadal failures, pituitary problems or treatments for advanced prostate cancer.
Numerous researches looking at andropause symptoms have been conducted to explore the mechanism that triggers the decreased testosterone production with age. Theories that have been proposed include:
 Other important hormones that have reduced production levels from age 30 onwards include Human Growth Hormone, Melatonin, DHEA, and Pregnenolone.
Other important hormones that have reduced production levels from age 30 onwards include Human Growth Hormone, Melatonin, DHEA, and Pregnenolone.
Growth hormone level in the body reaches its peak in the late teens. Then it starts its long decline at the rate of 14 percent reduction for each decade thereafter. By age 60, you could have lost as much as 60 percent of the amount of growth hormone in your body.
The growth hormone has been touted as the "elixir of growth" ever since Dr. Rudman published his landmark study in the New England Journal of Medicine. Dr. Rudman gave a group of healthy aging adults a high dose, low-frequency program of synthetic growth hormone injections for six months. The results showed a significant increase in lean body mass and a reduction of body fat. Dr. Rudman concluded that the growth hormone injections changed the body composition consistent with 10 to 15 years of aging. Since then, many studies and clinical trials have been conducted on growth hormone.
The deficiency of the human growth hormone causes many changes of somatopause with similar symptoms as testosterone deficiency. The replacement of testosterone without replacing growth hormone generally does not produce maximum effective results as both hormones work in synergistically with each other to produce the best results.
DHEA, an adrenal hormone, is the most abundant steroid hormone in the body. DHEA levels plummet dramatically with age, more than any other hormones, after peaking at around age 20. At the age of 40, production levels are only half the amount compared to age 20. By age 80, production levels are only five percent of the peak levels.
William Regelson, M. D. (1995), reviewed the effect on the male sexual function as documented in the groundbreaking Massachusetts Male Aging Study. This study investigated primarily the sexual function and activity in men aged 40 to 70. Of the 17 hormones measured in each man, only DHEA showed a direct and consistent correlation with impotence. As DHEA levels declined, the incidence of impotence increased. Other reported effects of increased DHEA included a reduction in blood insulin and glucose, increased lean body mass and reduction in fat, increased bone density and lowered cholesterol and blood pressure. DHEA rejuvenates virtually every organ system so it "actually makes you look, feel, and think better."
Pregnenolone is produced in the adrenal gland. Its production declines with age. Pregnenolone blocks and reverses many age-accelerating effects of excess cortisol.
Pregnenolone is also a potent neuro-nutrient that improves memory, concentration, and moods. It enhances brain function by facilitating the transmission of nerve impulses so that brain cells can communicate more easily. Pregnenolone can help to fight depression too. In one study, people who were not depressed had twice the amount of pregnenolone circulating in their bloodstreams.
Pregnenolone has the unique ability to balance all other hormones. It stimulates the production of other hormones only when they are needed.
Melatonin is produced in the pineal, which is located deep within the brain. Production levels of melatonin is reduced during the day and increased in the night. The amount of melatonin produced during the night is ten times the amount produced during the day.
 Melatonin is also a potent antioxidant that protects the pineal gland against free radical damage and helps defend our immune system. Researchers now believe that the pineal gland also drives the aging process.
Melatonin is also a potent antioxidant that protects the pineal gland against free radical damage and helps defend our immune system. Researchers now believe that the pineal gland also drives the aging process.
As you get older, the pineal gland produces less melatonin. The decline in production is slow and gradual after the age of 20. The loss is accelerated after the age of 40. Melatonin is usually not recommended for people under 40 years of age solely for its anti-aging benefits. This is because their production levels of melatonin have not yet declined significantly. Melatonin is commonly recommended for jet lag and as a sleeping aid, but we know that it can do much more.
Numerous scientific studies are currently underway to study the relationship of melatonin and longevity. In one interesting experiment, aging mice that received pineal gland from younger mice was discovered to have their life span increased by a third. Conversely, young mice given pineal gland from old mice had their life span reduced by one-third.
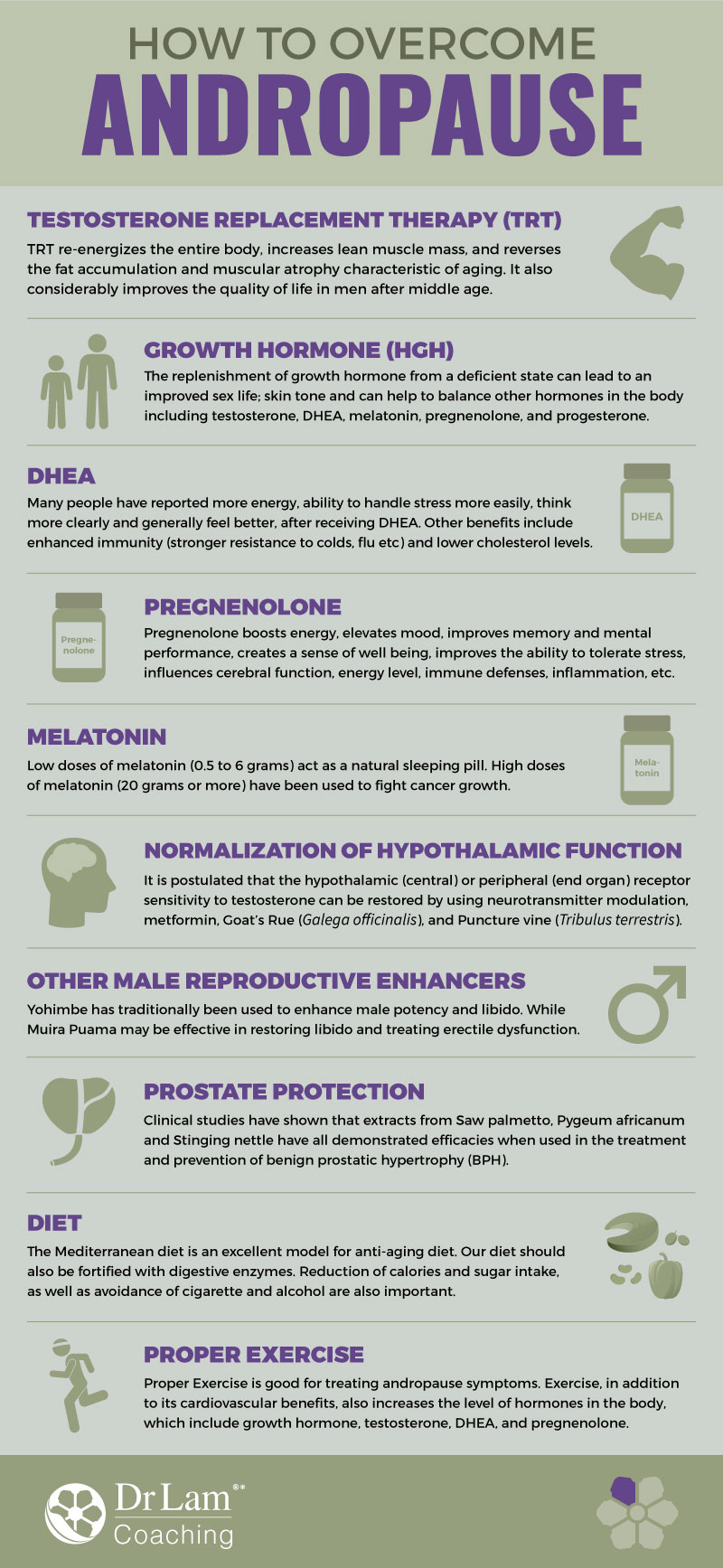
 Testosterone enanthate and cypionate are forms commonly used. They have comparable pharmacokinetics. Both result in supra-physiologic concentration of testosterone for 1 to 4 days after injection. A satisfactory regimen is to administer 200 mg of one of these esters once every two weeks intramuscularly, but a more physiologic replacement therapy would be 100 mg of one of these on a weekly basis. Trans-dermal synthetic TRT systems are perhaps the most commonly used. It comes in the form of scrotal and non-scrotal forms. Clinical studies have shown that both are effective forms of androgen replacement. The advantage of the scrotal form is that it produces high levels of circulating DHT due to the high 5-alpha-reductase enzyme activity of scrotal skin. It also requires shaving of the scrotum. Inadequate scrotal size and adherence problems are limitations. Skin irritation does occur in those with sensitive skins. Non-scrotal skin patch's advantage is that the serum testosterone concentration profile mimics the normal circadian variation observed in healthy young men. Skin irritation is more common, with over 50 percent experience some form of site reaction sometime during the treatment. Pretreatment with corticosteroid creams (not the ointment forms) has been shown to reduce the severity and incidence of skin irritation without significantly affecting testosterone absorption from the patch. Androgen replacement can have undesirable side effects, including frequent or persistent erections, nausea, vomiting, jaundice, ankle swelling, or virilization of female sexual partner. Breast enlargement can also develop as testosterone can be converted to estrogen via the enzyme aromatase. More serious complications include water retention, liver toxicity, cardiovascular disease, sleep apnea, and prostate enlargement. These risks are relatively uncommon when the dosage is closely monitored to that found physiologically in the body. Androgens are contraindicated in men with carcinoma of the breast or known or suspected carcinoma of the prostate. They also should not be considered in those with known hypersensitivity to the preparation or in patients with compromised cardiac, renal, or hepatic functions. While there is no direct evidence that link testosterone replacement to accelerated prostate enlargement, there is a correlation between testosterone treated hypogonadal men and normal men with prostrate volume and age. Prostate cancer is an androgen-responsive cancer, although there is no evidence to directly indicate that testosterone therapy causes prostate cancer. If prostate cancer cells already exist in the body, the disease may be stimulated to spread. Therefore, pre-treatment screening for any prostate dysfunction is mandatory. A digital rectal examination (DRE) and laboratory test for prostate specific antigen (PSA) should be checked before initiation of therapy and every 3 to 6 months thereafter. An abnormal DRE, an increase in PSA of more than 2 ng/dl, or a total PSA of greater than 4.0 ng/dl requires further urological evaluation. Other tests include hemotocrit, bone density, and plasma lipids on an annual basis. Results of testosterone replacement may not be evident for several weeks. Impotence may not be corrected after several months of therapy despite improvement in other andropause symptoms. For these patients, evaluation for causes of erectile dysfunction other than hypogonadism due to andropause is indicated.
Testosterone enanthate and cypionate are forms commonly used. They have comparable pharmacokinetics. Both result in supra-physiologic concentration of testosterone for 1 to 4 days after injection. A satisfactory regimen is to administer 200 mg of one of these esters once every two weeks intramuscularly, but a more physiologic replacement therapy would be 100 mg of one of these on a weekly basis. Trans-dermal synthetic TRT systems are perhaps the most commonly used. It comes in the form of scrotal and non-scrotal forms. Clinical studies have shown that both are effective forms of androgen replacement. The advantage of the scrotal form is that it produces high levels of circulating DHT due to the high 5-alpha-reductase enzyme activity of scrotal skin. It also requires shaving of the scrotum. Inadequate scrotal size and adherence problems are limitations. Skin irritation does occur in those with sensitive skins. Non-scrotal skin patch's advantage is that the serum testosterone concentration profile mimics the normal circadian variation observed in healthy young men. Skin irritation is more common, with over 50 percent experience some form of site reaction sometime during the treatment. Pretreatment with corticosteroid creams (not the ointment forms) has been shown to reduce the severity and incidence of skin irritation without significantly affecting testosterone absorption from the patch. Androgen replacement can have undesirable side effects, including frequent or persistent erections, nausea, vomiting, jaundice, ankle swelling, or virilization of female sexual partner. Breast enlargement can also develop as testosterone can be converted to estrogen via the enzyme aromatase. More serious complications include water retention, liver toxicity, cardiovascular disease, sleep apnea, and prostate enlargement. These risks are relatively uncommon when the dosage is closely monitored to that found physiologically in the body. Androgens are contraindicated in men with carcinoma of the breast or known or suspected carcinoma of the prostate. They also should not be considered in those with known hypersensitivity to the preparation or in patients with compromised cardiac, renal, or hepatic functions. While there is no direct evidence that link testosterone replacement to accelerated prostate enlargement, there is a correlation between testosterone treated hypogonadal men and normal men with prostrate volume and age. Prostate cancer is an androgen-responsive cancer, although there is no evidence to directly indicate that testosterone therapy causes prostate cancer. If prostate cancer cells already exist in the body, the disease may be stimulated to spread. Therefore, pre-treatment screening for any prostate dysfunction is mandatory. A digital rectal examination (DRE) and laboratory test for prostate specific antigen (PSA) should be checked before initiation of therapy and every 3 to 6 months thereafter. An abnormal DRE, an increase in PSA of more than 2 ng/dl, or a total PSA of greater than 4.0 ng/dl requires further urological evaluation. Other tests include hemotocrit, bone density, and plasma lipids on an annual basis. Results of testosterone replacement may not be evident for several weeks. Impotence may not be corrected after several months of therapy despite improvement in other andropause symptoms. For these patients, evaluation for causes of erectile dysfunction other than hypogonadism due to andropause is indicated. Close monitoring of serum testosterone levels should be carried out for patients on testosterone. Other signs, such as acne, increase breast size, and tenderness should be checked. After one week or more of trans-dermal TRT, serum testosterone levels can be measured about 12 hours after patch application and dosage adjusted accordingly. For oral methyltestosterone therapy, no assays are available to monitor therapy. For patients on the injectable form, nadir testosterone levels should be obtained 3 to 4 months prior to the next injection. Recently, natural forms of testosterone have become available which possess all the benefits of synthetic hormones and little adverse side effects. They are available from specialized compounding pharmacy under the prescription of a physician. The alternatives to testosterone include the testosterone precursors, androstenedione and androstenediol, which are available in oral capsules or sublingual sprays.While testosterone replacement is one of the most effective ways to relief andropause symptoms and may be indicated in the aging male with documented hypogonadism, this hormone should not be used in those with normal testosterone levels. Under the care of a knowledgeable physician, this therapy is very safe for the vast majority of andropause patients.
Close monitoring of serum testosterone levels should be carried out for patients on testosterone. Other signs, such as acne, increase breast size, and tenderness should be checked. After one week or more of trans-dermal TRT, serum testosterone levels can be measured about 12 hours after patch application and dosage adjusted accordingly. For oral methyltestosterone therapy, no assays are available to monitor therapy. For patients on the injectable form, nadir testosterone levels should be obtained 3 to 4 months prior to the next injection. Recently, natural forms of testosterone have become available which possess all the benefits of synthetic hormones and little adverse side effects. They are available from specialized compounding pharmacy under the prescription of a physician. The alternatives to testosterone include the testosterone precursors, androstenedione and androstenediol, which are available in oral capsules or sublingual sprays.While testosterone replacement is one of the most effective ways to relief andropause symptoms and may be indicated in the aging male with documented hypogonadism, this hormone should not be used in those with normal testosterone levels. Under the care of a knowledgeable physician, this therapy is very safe for the vast majority of andropause patients. DHEA. Many people have reported more energy, ability to handle stress more easily, think more clearly and generally feel better, after receiving DHEA. Other benefits include enhanced immunity (stronger resistance to colds, flu etc) and lower cholesterol levels. DHEA's ability to rejuvenate the immune function is particularly worthy of consideration. It boosts antibody production; enhances the activity of monocytes and maximizes the anti-cancer function of immune cells known as T lymphocytes. When administered concurrently with a flu vaccine, DHEA has been shown to improve the effectiveness of the vaccine in laboratory animals and in aging humans. One interesting note is that DHEA is not regulated by a negative feedback loop in the body. In other words, taking supplements of DHEA will not suppress the production of these hormones or cause the adrenal to rest and result in atrophy from the disuse. Theoretically, no "resting period" is required, although it is a good practice to have a resting cycle of a few weeks for every few months of therapy, as with all hormone replacement. DHEA replacement therapy offers powerful health benefits and is virtually risk-free. The usual starting dose is 25 mg. Men may require a higher quantity (up to 100 mg) while women may need less (up to 50 mg). The ideal anti-aging strategy is to supplement both DHEA and its precursor, pregnenolone. Commercial DHEA products are made from diosgenin, an extract from the Mexican wild yam of the Dioscorea family. Biochemists can convert diosgenin to DHEA by engineering a series of chemical conversions, but such conversion only happens in the laboratory and not in the human body. The ingestion of Dioscorea plant extracts cannot possibly lead to the formation of DHEA in the body.
DHEA. Many people have reported more energy, ability to handle stress more easily, think more clearly and generally feel better, after receiving DHEA. Other benefits include enhanced immunity (stronger resistance to colds, flu etc) and lower cholesterol levels. DHEA's ability to rejuvenate the immune function is particularly worthy of consideration. It boosts antibody production; enhances the activity of monocytes and maximizes the anti-cancer function of immune cells known as T lymphocytes. When administered concurrently with a flu vaccine, DHEA has been shown to improve the effectiveness of the vaccine in laboratory animals and in aging humans. One interesting note is that DHEA is not regulated by a negative feedback loop in the body. In other words, taking supplements of DHEA will not suppress the production of these hormones or cause the adrenal to rest and result in atrophy from the disuse. Theoretically, no "resting period" is required, although it is a good practice to have a resting cycle of a few weeks for every few months of therapy, as with all hormone replacement. DHEA replacement therapy offers powerful health benefits and is virtually risk-free. The usual starting dose is 25 mg. Men may require a higher quantity (up to 100 mg) while women may need less (up to 50 mg). The ideal anti-aging strategy is to supplement both DHEA and its precursor, pregnenolone. Commercial DHEA products are made from diosgenin, an extract from the Mexican wild yam of the Dioscorea family. Biochemists can convert diosgenin to DHEA by engineering a series of chemical conversions, but such conversion only happens in the laboratory and not in the human body. The ingestion of Dioscorea plant extracts cannot possibly lead to the formation of DHEA in the body. Melatonin One of the causes of the disruptions of sleeping patterns during aging is the reduction in the nightly release of melatonin by the pineal gland. Many people have discovered that bedtime doses of melatonin restored their ability to obtain a sound and peaceful night's sleep. Melatonin levels are known to decline drastically with age. Since melatonin and FSH appear to be antagonistic in women, the same relationship may be true for men. It has been postulated that melatonin may even act to normalize (lower) gonadotropin levels. It is one of the few substances that have repeatedly been shown to extend the maximum lifespan of experimental animals. While low doses of melatonin (0.5 to 6 grams) act as a natural sleeping pill, high doses of melatonin (20 grams or more) have been used to fight cancer growth.The exact dosage varies greatly between people . Trial and error is the best method. A higher dose does not mean more potency. Some people may feel better with a smaller dose. To normalize sleep and the bioclock, a good dosage to start is 1 mg and should be gradually increased if there are no side effects. A slight disorientation and dizziness may be experienced for the first few hours after waking up when melatonin treatment is first started. This sensation should go away after a few nights of melatonin use. If it persists, a reduced dose is recommended. There are a few rules for the effective use of melatonin. Firstly, always take this hormone just before bedtime. If you take it earlier in the day, it may disrupt sleeping and waking cycles.
Melatonin One of the causes of the disruptions of sleeping patterns during aging is the reduction in the nightly release of melatonin by the pineal gland. Many people have discovered that bedtime doses of melatonin restored their ability to obtain a sound and peaceful night's sleep. Melatonin levels are known to decline drastically with age. Since melatonin and FSH appear to be antagonistic in women, the same relationship may be true for men. It has been postulated that melatonin may even act to normalize (lower) gonadotropin levels. It is one of the few substances that have repeatedly been shown to extend the maximum lifespan of experimental animals. While low doses of melatonin (0.5 to 6 grams) act as a natural sleeping pill, high doses of melatonin (20 grams or more) have been used to fight cancer growth.The exact dosage varies greatly between people . Trial and error is the best method. A higher dose does not mean more potency. Some people may feel better with a smaller dose. To normalize sleep and the bioclock, a good dosage to start is 1 mg and should be gradually increased if there are no side effects. A slight disorientation and dizziness may be experienced for the first few hours after waking up when melatonin treatment is first started. This sensation should go away after a few nights of melatonin use. If it persists, a reduced dose is recommended. There are a few rules for the effective use of melatonin. Firstly, always take this hormone just before bedtime. If you take it earlier in the day, it may disrupt sleeping and waking cycles. Puncture vine (Tribulus terrestris) Tribulus is an herb that has been used for centuries in India as a treatment for both male and female sexual dysfunction including andropause symptoms. It has been widely tested for its efficacy in enhancing sperm quality and mobility. Tribulus has also been used to increase libido and sexual performance in experimental animals and men. Studies have shown that tribulus administration has resulted in an increase of LH levels by 72 percent and free testosterone levels by 41 percent. While the exact mechanism of action is not known, studies have shown that it enhances spermatogenesis by enhancing the activity of FSH upon the Sertolli cells in the testes. Tribulus also seems to stimulate the central nervous system directly to increase the secretion of LH thus resulting in an increased level of testosterone. It is also postulated that tribulus may directly sensitize the Leydig cells of the testes. These cells, in turn, produce testosterone in response to LH.
Puncture vine (Tribulus terrestris) Tribulus is an herb that has been used for centuries in India as a treatment for both male and female sexual dysfunction including andropause symptoms. It has been widely tested for its efficacy in enhancing sperm quality and mobility. Tribulus has also been used to increase libido and sexual performance in experimental animals and men. Studies have shown that tribulus administration has resulted in an increase of LH levels by 72 percent and free testosterone levels by 41 percent. While the exact mechanism of action is not known, studies have shown that it enhances spermatogenesis by enhancing the activity of FSH upon the Sertolli cells in the testes. Tribulus also seems to stimulate the central nervous system directly to increase the secretion of LH thus resulting in an increased level of testosterone. It is also postulated that tribulus may directly sensitize the Leydig cells of the testes. These cells, in turn, produce testosterone in response to LH. Due to their multiple actions, it should be no surprise that when these botanicals are combined, they are even more effective than when used individually. An estimated 90 percent of men who have mild to moderate BPH experience some improvement in symptoms during the first four to six weeks of therapy. Saw palmetto has been shown to have very few side effects. Since it does not interfere with PSA levels, saw palmetto will not hide cancer symptoms during PSA tests. Botanical should be seriously considered as a first natural alternative to drugs for those who wish to alleviate symptoms of BPH. These botanicals can also act as a prophylactic for those who are keen to prevent the onset of BPH. Healthy men about to or already in andropause should consider saw palmetto as part of a comprehensive anti-aging program.
Due to their multiple actions, it should be no surprise that when these botanicals are combined, they are even more effective than when used individually. An estimated 90 percent of men who have mild to moderate BPH experience some improvement in symptoms during the first four to six weeks of therapy. Saw palmetto has been shown to have very few side effects. Since it does not interfere with PSA levels, saw palmetto will not hide cancer symptoms during PSA tests. Botanical should be seriously considered as a first natural alternative to drugs for those who wish to alleviate symptoms of BPH. These botanicals can also act as a prophylactic for those who are keen to prevent the onset of BPH. Healthy men about to or already in andropause should consider saw palmetto as part of a comprehensive anti-aging program.Musculoskeletal System Protection:
Cancer Prevention:
 Their saturated fats, refined carbohydrates and sugar intake are very low. The Mediterranean diet is an excellent model for anti-aging diet. Fruits and vegetables contain abundant antioxidants and phytonutrients. Fish contains essential fatty acids that are critical building blocks of neurotransmitters and hormones. Moderate amount of plant-based protein such as soybean is easy on the digestive system compared to red or white meat. Our diet should be fortified with digestive enzymes such as amylase, cellulase and lipase, which may be needed to digest protein and enhance gastrointestinal health and treatandropause symptoms. This should be part of the daily supplement intake. Reduction of sugar intake and avoidance of cigarette and alcohol are also important. Finally, a reduction of calories by 30 percent to achieve 5 to 10 percent below the ideal body weight should be considered.
Their saturated fats, refined carbohydrates and sugar intake are very low. The Mediterranean diet is an excellent model for anti-aging diet. Fruits and vegetables contain abundant antioxidants and phytonutrients. Fish contains essential fatty acids that are critical building blocks of neurotransmitters and hormones. Moderate amount of plant-based protein such as soybean is easy on the digestive system compared to red or white meat. Our diet should be fortified with digestive enzymes such as amylase, cellulase and lipase, which may be needed to digest protein and enhance gastrointestinal health and treatandropause symptoms. This should be part of the daily supplement intake. Reduction of sugar intake and avoidance of cigarette and alcohol are also important. Finally, a reduction of calories by 30 percent to achieve 5 to 10 percent below the ideal body weight should be considered.
Andropause symptoms are a very common complaint for men over the age of forty. They're caused by the changes in hormone levels that occur during life stage and can be mild or can almost completely disrupt your health and way of life. There are several different ways to address these symptoms ranging from medications to lifestyle changes that support more natural hormone levels. If you experience problems because of hormone imbalances as you age, then here's what to do:
The human body can experience a range of problems as it age and these issues are often compounded by the symptoms and issues associated with adrenal fatigue. If you need help, support, or advice relating to this process, talk to our team by clicking here or call us on +1 (626) 571-1234.
© Copyright 2020 Michael Lam, M.D. All Rights Reserved.
