 Adrenal hormones are essential for life. Too much of them or too little, however, can be dangerous. An imbalance of these crucial hormones can oftentimes be the source of what causes fatigue. How can we find a solution to what causes fatigue? Hormone replacement is commonly prescribed by physicians when presented with a patient's symptoms suggestive of adrenal insufficiency. In the early days of adrenal hormone replacement, researchers had little clue of the proper dosage or the complications resulting from toxicity. Misled by improvement in their patients' symptoms, they gave patients many times more adrenal hormones than the normal amount to fix what causes fatigue. Cortisol was the drug of choice. Many patients suffered toxic effects as a result of this and died. Long term and excessive use of cortisol has many negative side effects as well, to the extent that its use as a performance enhancer in competitive sports has now been universally banned. As a result of these bad experiences, many researchers became frightened and avoided prescribing adrenal hormones such as cortisol whenever possible to fix what causes fatigue.
Adrenal hormones are essential for life. Too much of them or too little, however, can be dangerous. An imbalance of these crucial hormones can oftentimes be the source of what causes fatigue. How can we find a solution to what causes fatigue? Hormone replacement is commonly prescribed by physicians when presented with a patient's symptoms suggestive of adrenal insufficiency. In the early days of adrenal hormone replacement, researchers had little clue of the proper dosage or the complications resulting from toxicity. Misled by improvement in their patients' symptoms, they gave patients many times more adrenal hormones than the normal amount to fix what causes fatigue. Cortisol was the drug of choice. Many patients suffered toxic effects as a result of this and died. Long term and excessive use of cortisol has many negative side effects as well, to the extent that its use as a performance enhancer in competitive sports has now been universally banned. As a result of these bad experiences, many researchers became frightened and avoided prescribing adrenal hormones such as cortisol whenever possible to fix what causes fatigue.
In addition to adrenal hormones, the use of thyroid replacement to fix what causes fatigue brought on by Adrenal Fatigue is a common practice. In fact, many people with Adrenal Fatigue with symptoms of low thyroid function are prescribed thyroid medications as if they suffer from primary hypothyroidism. Many continue to suffer. In the early days of thyroid hormone replacement, patients received up to many times the usual dose of thyroid hormone as well and as a result, the toxic effects could be severe.
Clearly, hormone replacement therapy in a setting of Adrenal Fatigue requires careful attention and the use of adrenal hormones needs to be put into perspective. In the right situation and using the right dose, hormone replacement can be of great benefit alleviating what causes fatigue.
Medical science is just beginning to realize that a person can feel horrible and function poorly even with a minimal to moderate hormone deficiency that is not clinically detectable by routine blood tests for a solution to what causes fatigue. This is evident in the case of Adrenal Fatigue. Adrenal hormones are under the control of the hypothalamus-pituitary-adrenal axis where over 50 hormones are involved, and dysregulation of any one of these can produce unpleasant symptoms and be a factor in what causes fatigue. For example, low aldosterone level can lead to blood pressure irregularities and fatigue, high estrogen can trigger PMS and anxiety, and low cortisol output can lead to sugar dysregulation, hypoglycemia and sluggishness. Those in the advanced stages of Adrenal Fatigue are especially vulnerable to what causes fatigue. Unfortunately, laboratory tests and other investigative tools are not very helpful when it comes to Adrenal Fatigue and what causes fatigue due to inconsistent clinical correlation. However, good qualitative challenges can be helpful. Paying close attention to the signs and symptoms of Adrenal Fatigue and what causes fatigue is perhaps the most effective way to assess whether or not there is the need for hormone replacement. The ultimate decision as to whether or not use hormone replacement as an Adrenal Fatigue recovery tool or for what causes fatigue is best left to the professional. Due to poorly understood patho-physiological mechanisms, some trial and error in administering hormone replacement will be inevitable even in the best of hands.
The adrenal glands are two small glands; each about the size of a large grape and their role in producing hormones required for optimal living is crucial. The outer adrenal cortex comprises eighty percent of the adrenal gland and is responsible for producing over 50 different types of hormones in three major classes-glucocorticoids, mineral corticoids and androgens. Without proper hormonal production and balance, it is impossible for anyone to feel good and what causes fatigue.
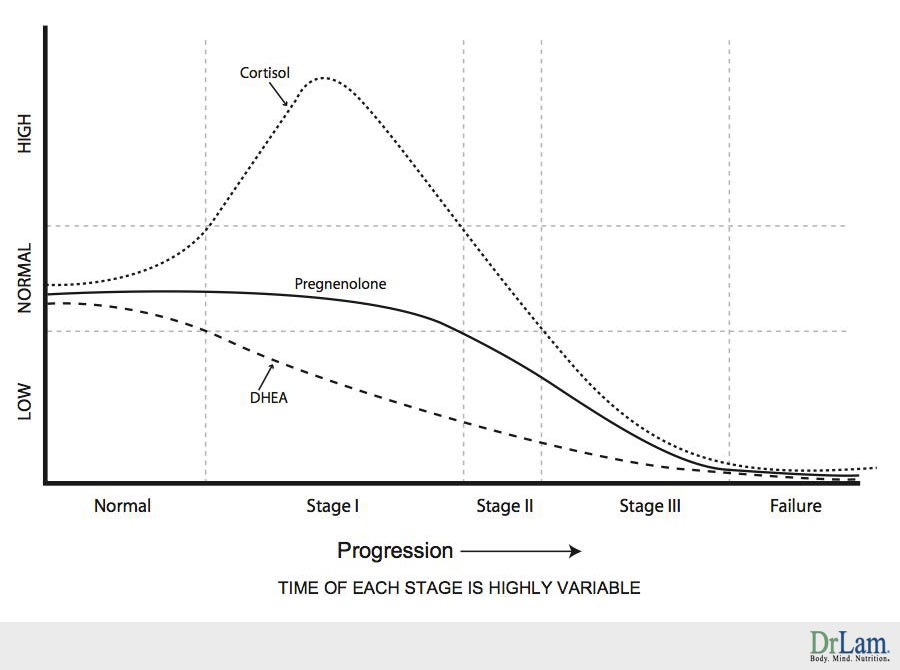
When the adrenals are weak, production of any or all of these hormones will be affected. Hormones can be over-produced or under produced, depending on the state of fatigue of the adrenals, and also on each person's intrinsic body constitution. For example, cortisol output in the body usually rises in Stages 1 and 2 but will subsequently fall when a person enters into Stage 3 and beyond. DHEA level tends to fall gradually as Adrenal Fatigue progresses from Stages 1 to 4. DHEA output can also be high temporarily during onset of Adrenal Fatigue. Pregnenolone output also tends to rise in early stages of Adrenal Fatigue just like cortisol before it starts to fall due to a phenomenon known as pregnenolone steal.
In addition to output considerations, we need to pay attention to how these hormones are broken down and metabolized to help understand what causes fatigue. All steroidal hormones are metabolized to a great degree by the liver. The more advanced the Adrenal Fatigue and signs of what causes fatigue, the more compromised the liver function generally. Hormones required for recovery from Adrenal Fatigue and from what causes fatigue need to be considered not only their absolute quantity. Just as important is consideration of the overall clearance state of the body to get rid of metabolic byproducts of the various hormones. Hormone replacement therapy for people suffering from Adrenal Fatigue, whether it is in synthetic or bio-identical form, is therefore difficult and challenging especially when factoring in what causes fatigue. It should be undertaken only under the close supervision of an experienced health care provider after more gentle first line recovery tools have been exhausted. In other words, adrenal hormone replacement should not be considered as a first line remedy for what causes fatigue until better and gentler compounds that can get the job done without the risk of side effects, has failed. Premature use of adrenal hormonal replacement is common in most self-navigation programs, is a common mistake, and can be a major cause of recovery delay or failure. Improper use of adrenal hormonal replacement in fact can be what causes fatigue and makes the condition worse due to toxicity, paradoxical effects, addiction, and withdrawal complications. Worst of all, it may also trigger adrenal crashes.
A steroid is a chemical substance with four carbon ring structures attached to each other in a very specific and unique fashion. Cortisol, DHEA, testosterone, pregnenolone, progesterone, and estrogen are all steroid-based hormones that chemically look very similar to each other in terms of their basic molecular structures. They are all made in the adrenals with cholesterol being the raw material. However, their actions differ markedly, with enormous differences in how they function and in the roles they play in the various chemical factories of our bodies.
The following is a simplified diagram of how the key adrenal hormones are made:
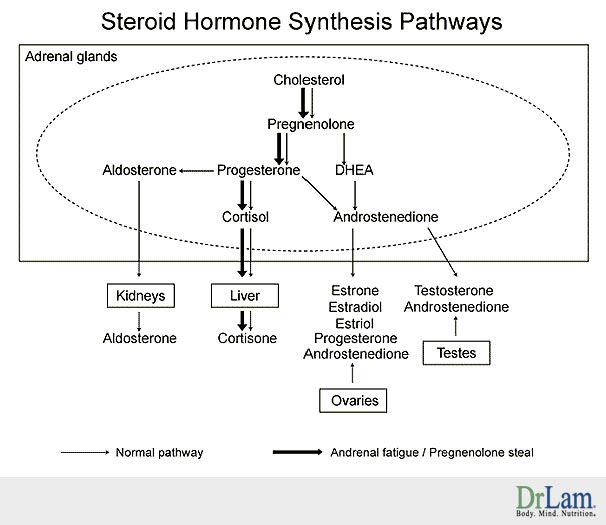
Each hormone produced acts as part of an overall orchestra of hormones where proper balance is essential for optimal adrenal function. Each hormone has an important role to play in the overall scheme of things inside the body. In addition to recognizing the sequential cascade of hormonal synthesis, it is very important to understand that pro-hormones such as pregnenolone and DHEA, which are placed naturally at the top of the cascade, are gentler as compared to down-stream hormones such as testosterone and cortisol. The more gentle the hormone, the more nurturing it is for the adrenal to make its own down-stream hormone and the less will be the side effects. Pro-hormones are less potent but contrast this with the cortisol, which is the most potent, and has the greatest potential side effects especially in what causes fatigue.
This article will examine some of the most common steroidal hormone replacements and their clinical ramification in the Adrenal Fatigue setting and these hormones are: Pregnenolone, DHEA, cortisol, melatonin, testosterone, estrogen, progesterone, and also DHEA. Thyroid replacement will be covered separately due to its importance.
Pregnenolone is called the mother of all steroid hormones for a good reason. It is a steroid hormone at the top of the hormonal production cascade. It is also the precursor in the synthesis of female hormones such as estrogen and progesterone, mineralocorticoids such as aldosterone that is responsible for sodium regulation, glucocorticoids such as cortisol that suppresses inflammation and helps to reduce stress, and androgens such as testosterone. Pregnenolone is therefore aptly called a pro-hormone.
Back in the 1940s, when researchers started experimenting with the use of pregnenolone, they realized that it could be helpful for people who were under stress and that it could also increase energy in those who were fatigued. However, at about the same time, cortisol, another closely related hormone, was discovered and it stole the limelight, as it was far more potent. When cortisol was given to individuals with rheumatoid arthritis or other inflammatory conditions, there were outstanding short-term improvements.
During periods of stress, the output of adrenal steroids such as cortisol will increase, which will put a great demand on pregnenolone production. This may lead to pregnenolone deficiency, which in turn may lead to a reduction of both glucocorticosteroids and mineralocorticoids such as cortisol and aldosterone respectively.
Numerous studies have shown the effects of pregnenolone on the body and brain. In normal people, pregnenolone will boost energy, elevate mood and improve memory and mental performance. Pregnenolone will also create a sense of well being while improving the ability to tolerate stress. Furthermore, pregnenolone has a host of other benefits, which include the ability to influence cerebral function, the female reproductive cycle, immune defenses, inflammation, mood, skin health, sleep patterns, stress tolerance, and wound healing. As an anti-aging tool, taking pregnenolone will, therefore, rejuvenate the entire adrenal cascade. However, in the case of Adrenal Fatigue, replacement tends to be more complex.
 Some with Adrenal Fatigue find pregnenolone replacement improves their energy, vision, memory, clarity of thinking, well being, and often sexual enjoyment or libido. Some women report lessening of hot flashes or premenstrual symptoms and this is likely due to the rise of progesterone (the biological daughter of pregnenolone) reduction in estrogen dominance. Others, however, may find pregnenolone worsen existing fatigue and may even trigger adrenal crashes. Such paradoxical reactions are common. The more advanced the adrenal weakness, the more likely such experiences are common.
Some with Adrenal Fatigue find pregnenolone replacement improves their energy, vision, memory, clarity of thinking, well being, and often sexual enjoyment or libido. Some women report lessening of hot flashes or premenstrual symptoms and this is likely due to the rise of progesterone (the biological daughter of pregnenolone) reduction in estrogen dominance. Others, however, may find pregnenolone worsen existing fatigue and may even trigger adrenal crashes. Such paradoxical reactions are common. The more advanced the adrenal weakness, the more likely such experiences are common.
Part of the reason can be explained by pregnenolone's unusual response curve. Many studies have found a U-shaped distribution in the therapeutic response to pregnenolone therapy. The U-shaped distribution describes a benefit associated with low dose pregnenolone, a loss of effect with increasing dose of pregnenolone, and a second peak of benefit with higher doses of the steroid. It is unknown what dosage range is represented in either part of the U-shaped curve for humans and whether or not this curve is altered by disease.
The cells of the adrenal glands, as well as the central nervous system, synthesize pregnenolone. In Adrenal Fatigue, pregnenolone level usually stays high in early stages, but tends to be low as adrenal weakness progresses due to a phenomena known as "pregnenolone steal" as the pregnenolone level drops because the body bypasses pregnenolone production in favor of producing more down-stream hormones such as DHEA and cortisol.
Taking pregnenolone for adrenal fatigue can therefore be challenging for multiple reasons as paradoxical reaction is a major concern. In addition, one can take what appears to be an adequate dosage but will not benefit from this if the body is shunting it towards cortisol production. On the other hand, overdose is possible if too much is taken over time.
The normal starting dose is 15 mg, increasing up to 100 mg for men or women. Pregnenolone should be derived from a pharmacologically pure product and not a yam-derived "precursor." Oral pregnenolone pills work well. Sublingual administration is an excellent option by bypassing the initial liver metabolism that occurs after swallowing an oral pill but it tends to be "spiky" and not well tolerated by those who are sensitive or in advanced s adrenal fatigue state.
Pregnenolone is converted in the body to progesterone and these two hormones have some overlapping similarities. Pregnenolone is also converted into DHEA, which, in turn may convert into androstenedione, testosterone, and estrogens. Pregnenolone supplementation may increase progesterone levels and consequently other hormones in the body (testosterone and estradiol).
Side effects of pregnenolone include:

Due to the possible side effects, pregnenolone should be taken under the supervision of a health care professional. Do not rely on blood or saliva tests alone to determine how much pregnenolone should be taken as the clinical correlation is unreliable in Adrenal Fatigue.
Due to its antagonistic effects on the GABA receptor in the central nervous system, pregnenolone therapy may be contraindicated in some people with a history of seizures. Pregnenolone may inhibit drugs used to increase GABA activity (i.e. Neurontin); these drugs are frequently used in the treatment of epilepsy and depression.
Both pregnenolone and DHEA can be taken together for Adrenal Fatigue. Since some pregnenolone is converted into DHEA, the intake amount of DHEA can be lowered if both are taken together.
DHEA is the biological daughter of pregnenolone. It is a weak androgenic hormone made in large amounts in the adrenal glands of both sexes. DHEA is a precursor of testosterone, estrogen, and corticosteroids. Their actions are similar, but generally, DHEA is more potent than pregnenolone. Energy generation appears to be more intense.
DHEA is commonly used as a hormone replacement therapy for energy enhancement and anti-aging. Supplementation with DHEA can improve well-being, energy levels, moods, and libido for normal healthy people. Dosages of 15 to 25 mg of pregnenolone and 25 to 50 mg DHEA seem to do the trick in many women as it can bring them a renewed sense of well-being. Men are less hormone sensitive and the results may not be as evident. For men, direct testosterone precursors such as androstenedione (and its metabolite androstenediol) may be more effective. These protocols, however, only apply to healthy individuals and not to those who are afflicted with Adrenal Fatigue.
DHEA is also widely used in Adrenal Fatigue. Their actions tend to mimic pregnenolone, but amplified, both in terms of desired results and side effects. Therefore, DHEA use should be judicious, as different doses appear to do different things. DHEA does not convert into progesterone; rather it converts into estrogen and testosterone. High dosages (100 to 200 mg or more) can lead to a repartitioning of body mass as a result of the conversion of the DHEA into more androgenic steroid hormones. Significant side effects are similar to those of pregnenolone, only more severe. Hair loss and acne are particularly common.
 Even low dose DHEA can be problematic, as it tends to be quite stimulatory for those people with advanced adrenal weakness. In particular, those in Stage 3 (Adrenal Exhaustion) tend to react strongly even at minute dosage. Additional side effects such as severe anxiety, feeling jittery, and PMS are common and they seem to be more prevalent in women.
Even low dose DHEA can be problematic, as it tends to be quite stimulatory for those people with advanced adrenal weakness. In particular, those in Stage 3 (Adrenal Exhaustion) tend to react strongly even at minute dosage. Additional side effects such as severe anxiety, feeling jittery, and PMS are common and they seem to be more prevalent in women.
Since DHEA is a slight mood elevator, it can potentially clash with anti-depressants. Theoretically, the dosage of anti-depressants can be lowered if DHEA is taken. People on cholesterol lowering drugs as well as blood thinning medications, such as Coumadin, may need to watch their medications, as well as their requirements, because the amounts required to be taken may well be reduced since DHEA has both a cholesterol lowering and blood thinning effect. Studies have shown that DHEA also reduces appetite and this means that those who want to lose weight may benefit from DHEA, and those who are already on weight reduction pills may need less.
One interesting thing about DHEA is that it is not regulated by a negative feedback loop in the body. In other words, taking DHEA supplements will not suppress the production of these hormones or cause the adrenals to rest and result in atrophy from disuse. Theoretically, no "resting period" is required, although it may be a good practice to have a resting cycle of a few weeks for every few months of therapy.
Commercial DHEA products are made from diosgenin, an extract from the Mexican wild yam of the Dioscorea family. Biochemists can convert diosgenin to DHEA by engineering a series of chemical conversions, but such conversion will only happen in the laboratory and not in the human body. Therefore, ingestion of Dioscorea plant extracts cannot possibly lead to the formation of DHEA inside the body. DHEA should be used under professional guidance in the Adrenal Fatigue setting. Dosage determination can be tricky as it is not straightforward. Special attention needs to be paid to the many possible side effects similar to those of pregnenolone.
Depending on the stage of Adrenal Fatigue and on each person's constitution, the blood or saliva DHEA level can increase while Adrenal Fatigue is in progression instead of going into gradual decline. Serum absolute levels are generally not very helpful due to inconsistent clinical correlation. From the Adrenal Fatigue perspective, DHEA should be viewed in conjunction with total cortisol. DHEA is an anabolic hormone (a building up hormone) while cortisol is a catabolic hormone (for breaking down tissues). The absolute DHEA level by itself in the Adrenal Fatigue context has little meaning. If the total cortisol to DHEA ratio is high, then there will be excessive cortisol relative to DHEA. That points to a body in a catabolic state.
The most important anti-stress hormone in the body is cortisol and it is produced in the adrenal cortex. Cortisol protects the body from excessive Adrenal Fatigue by:

In short, cortisol sustains life via two opposite, but related, kinds of regulatory actions: releasing and activating the existing defense mechanisms of the body, while shutting down and modifying the same mechanisms to prevent them.
Cortisol production from the adrenal glands is controlled via the hypothalamic-pituitary-adrenal (HPA) axis. There is an existing negative feedback loop that governs the amount of adrenal hormones that are being secreted under normal circumstances in normal people. For example, the HPA axis adjusts cortisol levels according to the body's need via a hormone called Adrenal Corticotropic Hormone (ACTH) that is secreted by the pituitary gland in response to signals from the hypothalamus. When the ACTH binds to the walls of the adrenal gland cells, a chain reaction occurs within the cells, leading to the release of cholesterol where it is manufactured into pregnenolone, the first hormone in the adrenal cascade. After this, cortisol is released into the blood stream where it travels in the circulatory system to all parts of the body and back to the hypothalamus.
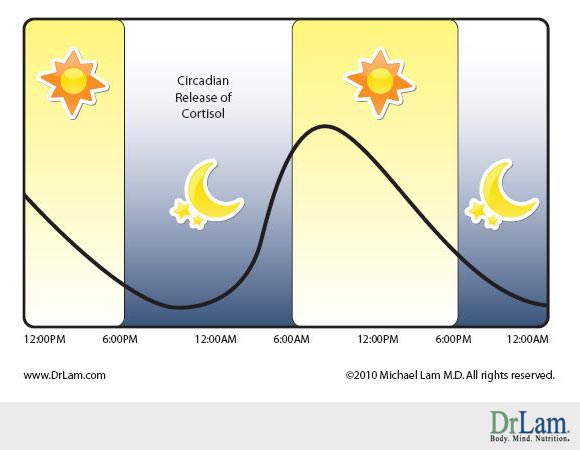
Cortisol and ACTH are not secreted uniformly throughout the day. They follow a diurnal pattern, with the highest level secreted at around 8:00 a.m., after which there is a gradual decline throughout the day. Episodic spikes during the day can also occur when the body is stressed or when certain foods are eaten. The cortisol level is at its lowest between midnight and 4:00 a.m. Morning cortisol is indicative of peak cortisol output. Noon cortisol is indicative of cortisol adaptability and usage. Afternoon cortisol is associated more with sugar regulation than adrenal cortex function, while evening cortisol level points to adrenal baseline function.
Cortisol level, especially in the morning, is characteristically high for those in Stages 1 and 2 Adrenal Fatigue as the adrenals are put on overdrive to produce more cortisol in order to neutralize stress. As Adrenal Fatigue progresses, cortisol output will eventually peak and then start to decline. Those people who are in Stage 3 Adrenal Fatigue invariably face a low cortisol level in the morning. After this time, the body's cortisol output for the rest of the day will remain low. A 24-hour saliva cortisol curve is commonly flat throughout the day in Adrenal Exhaustion (Stage 3 Adrenal Fatigue). There are many exceptions to the above generalization and this is why relying on a test result to determine the body's cortisol level, as the sole clinical yardstick can be very misleading. For example, some patients who are Stage 2 Adrenal Fatigue can present themselves with high evening cortisol but low or normal morning cortisol. These people tend to have low energy in the morning, with alertness returning around evening time. Despite high evening cortisol, they may be able to sleep well without sleep onset insomnia that commonly plagues those with high evening cortisol. As if this is not confusing enough, some people in Stage 3 Adrenal Fatigue clinically can present with a typical Stage 1 Adrenal Fatigue cortisol curve for reasons not well understood.
Conventional physicians have been using cortisol, also known as hydrocortisone, to combat Addison's disease for decades. The drug is widely available under the trade name Cortef. Some have advocated the use of cortisol for treating Adrenal Fatigue as well. Some physicians, notably, Dr. Jefferies in the mid 1980s, have advocated low dose cortisol as safe for long-term use. Dr. Jefferies found that as long as the adrenal hormone level is kept within the normal range, the main toxicity that a patient might experience was a slight upset stomach, due to the body not being used to having the hormone come in through the stomach. Advances in nutritional therapeutics over the years have now greatly reduced the need of using this medication in most Adrenal Fatigue situations other than in the most serious cases. Many, however, continue to use cortisol as a first line recovery medication for Adrenal Fatigue. Over-use of cortisol as an Adrenal Fatigue recovery tool is a serious concern.
There is little question of the great benefits of cortisol for those who need it; cortisol can be a lifesaver for someone in a severe stage of Adrenal Fatigue. The gentler natural compounds such as vitamin C, vitamin B, DHEA, and pregnenolone, when dosed and delivered properly, will greatly support adrenal health. In such cases, external cortisol administration may be delayed or avoided. However, the clinical picture is anything but straight-forward.
 The use of cortisol must be considered with great care. This is because the more advanced the Adrenal Fatigue the more prevalent the symptoms of intolerance. A good portion of people suffering from advanced Adrenal Fatigue actually cannot tolerate cortisol and in fact, their condition can become worse, even at low dose. Adrenal crashes may be triggered. The exact etiology is not known. Many will require a few weeks to get used to the medication, and the beneficial effect may not be immediately evident. Still worse is the issue of addiction and withdrawal symptoms, as anyone who has gone through those problems will tell you what a nightmare things can be.
The use of cortisol must be considered with great care. This is because the more advanced the Adrenal Fatigue the more prevalent the symptoms of intolerance. A good portion of people suffering from advanced Adrenal Fatigue actually cannot tolerate cortisol and in fact, their condition can become worse, even at low dose. Adrenal crashes may be triggered. The exact etiology is not known. Many will require a few weeks to get used to the medication, and the beneficial effect may not be immediately evident. Still worse is the issue of addiction and withdrawal symptoms, as anyone who has gone through those problems will tell you what a nightmare things can be.
Fortunately, as mentioned earlier, modern advances in nutritional therapeutics have rendered the use of cortisol unnecessary in most cases. Cortisol can be considered as a last resort. In fact, one of the key goals in Adrenal Fatigue recovery is to let the body heal itself naturally and wean off from cortisol dependency for those who have been on it long term.
Most patients find that 5 to 10 mg of Cortef in the morning, 0 to 7 1/2 mg at noon and 0 to 2 1/2 mg at 4 p.m. often work best. The actual dosage used needs to be adjusted to match the body's need. Those who are on cortisol should slowly decrease their dosage after a few months if possible, eventually discontinuing the treatment entirely. The key to this is to rebuild the adrenal reserve first with natural compounds before titrating down cortisol dosage to avoid negative and unpleasant rebound withdrawal side effects and adrenal crashes.
There are many side effects when using cortisol. If the dose is too high, one may feel shaky and the dosage should then be lowered. If cortisol causes upset stomach, the patients should take it with meals or lower the dose. If taken too late in the day, Cortef can disrupt sleep. At a dose of over 20 mg a day, one will begin to see the more toxic side effects of cortisol. Clearly higher doses are not recommended unless the benefits do clearly outweigh the risks.
Another important function of the adrenal glands is to maintain blood volume and pressure. Low blood pressure, low blood volume, electrolyte imbalance, and dehydration are common in people suffering from Adrenal Fatigue Stage 3. In such cases, the prescription adrenal hormone, fludrocortisones (sold under the brand name Florinef) may be indicated and can be a lifesaver.
 There may be things about hormonal imbalance that are affecting your quality of life. Could what you dont know about hormonal imbalance be causing you discomfort? Is what you dont know about hormonal imbalance degrading your life? Keep reading to learn more about hormonal imbalance and discover ways to improve your life. Testosterone is produced by both men and women but the amount produced by women is much smaller and the production comes from the adrenal glands. A decline in the testosterone level is associated with decrease in sex drive and libido in both sexes. This condition is commonly observed in those with Adrenal Fatigue. Testosterone replacement therapy (TRT) re-energizes the entire body, increases lean muscle mass, and reverses the fat accumulation and muscular atrophy characteristic of aging in normal people. Unfortunately, the tricky thing about hormonal imbalance, is that aggressive use of testosterone in Adrenal Fatigue can lead to over stimulation and eventually to adrenal crashes.
There may be things about hormonal imbalance that are affecting your quality of life. Could what you dont know about hormonal imbalance be causing you discomfort? Is what you dont know about hormonal imbalance degrading your life? Keep reading to learn more about hormonal imbalance and discover ways to improve your life. Testosterone is produced by both men and women but the amount produced by women is much smaller and the production comes from the adrenal glands. A decline in the testosterone level is associated with decrease in sex drive and libido in both sexes. This condition is commonly observed in those with Adrenal Fatigue. Testosterone replacement therapy (TRT) re-energizes the entire body, increases lean muscle mass, and reverses the fat accumulation and muscular atrophy characteristic of aging in normal people. Unfortunately, the tricky thing about hormonal imbalance, is that aggressive use of testosterone in Adrenal Fatigue can lead to over stimulation and eventually to adrenal crashes.
Pre-TRT workups should include a complete history and physical examination, together with a battery of blood tests including male hormonal profile and cancer screening tests such as prostate specific antigen (PSA) to rule out any relative or absolute contraindications to testosterone replacement therapy. Various forms of synthetic testosterone have traditionally been used and these include oral, sublingual, intramuscular injection, and trans-dermal patches. While these synthetic hormones have been widely used with beneficial effects, there are drawbacks to their use. Keep reading to learn even more about hormonal imbalance.
Oral synthetic preparations result in short-term elevation and undesirably high inter-individual and intra-individual variability of concentrations of testosterone. There are also commonly associated elevations of liver function tests and abnormalities at liver scans. Despite this, oral preparations still constitute about a third of prescriptions filled in the United States. Some common forms are pure testosterone, methyl testosterone, sublingual methyl testosterone and fluoxymesterone.e
The injectable synthetic testosterone is etherified. It is safe, effective, and the least expensive androgen preparation available. Learn more about hormonal imbalance treatment. Keep reading. When injected into a large muscle, it slowly absorbs and lasts longer, taking effect over several days to weeks. Injections eliminate the natural daily diurnal rhythm of testosterone production-high at night and early morning and low during the day. Testosterone enanthate and cypionate are forms commonly used and they have comparable pharmacokinetics. Both result in supra-physiologic concentration of testosterone for one to four days after injection. A satisfactory regimen is to administer 200 mg of one of these esters once every two weeks intramuscularly, but a more physiologic replacement therapy would be 100 mg of one of these on a weekly basis.
Trans-dermal synthetic TRT systems are perhaps the most commonly used and they come in scrotal and non-scrotal forms. Clinical studies about hormonal imbalance have shown that both are effective forms of androgen replacement. The advantage of the scrotal form is that it produces high levels of circulating dihydrotestosterone (DHT) due to the high 5-alpha-reductase enzyme activity of scrotal skin and it requires shaving the scrotum. Inadequate scrotal size and adherence problems are limitations. Skin irritation does occur in those with sensitive skin. Non-scrotal skin patch's advantage is that the serum testosterone concentration profile mimics the normal circadian variation observed in healthy young men. However, skin irritation is more common, with over 50 percent of users experiencing some form of site reaction sometimes during treatment. Pretreatment with corticosteroid creams (not the ointment forms) has been shown to reduce the severity and incidence of skin irritation without significantly affecting testosterone absorption from the patch helping us to learn more about hormonal imbalance treatments.
 When learning about hormonal imbalance, it is important to remember that testosterone replacement can have undesirable side effects, including frequent or persistent erections, nausea, vomiting, jaundice, ankle swelling, or virilization of the female sexual partner. Breast enlargement can also develop as testosterone can be converted to estrogen via the enzyme aromatase. More serious complications include water retention, liver toxicity, cardiovascular disease, sleep apnea and prostate enlargement. These side effect risks are relatively uncommon when the dosage is closely monitored to that found physiologically in the body.
When learning about hormonal imbalance, it is important to remember that testosterone replacement can have undesirable side effects, including frequent or persistent erections, nausea, vomiting, jaundice, ankle swelling, or virilization of the female sexual partner. Breast enlargement can also develop as testosterone can be converted to estrogen via the enzyme aromatase. More serious complications include water retention, liver toxicity, cardiovascular disease, sleep apnea and prostate enlargement. These side effect risks are relatively uncommon when the dosage is closely monitored to that found physiologically in the body.
Results of testosterone replacement may not be evident for several weeks. Impotence may not be corrected after several months of therapy despite improvement in other andropause symptoms. For these patients, evaluation for causes of erectile dysfunction other than hypogonadism due to andropause is indicated.
Close monitoring of serum testosterone levels should be carried out for patients on testosterone. Other signs, such as acne, increase in breast size, and tenderness should be checked. After one week or more of trans-dermal TRT, serum testosterone levels can be measured about 12 hours after patch application and the dosage can then be adjusted accordingly. For oral methyltestosterone therapy, no assays are available to monitor therapy. For patients on the injectable form, nadir testosterone levels should be obtained three to four months prior to the next injection.
In studying about hormonal imbalance, we learn the alternatives to testosterone includes the testosterone precursors, androstenedione and androstenediol, which are available in oral capsules or sublingual sprays.
While testosterone replacement is one of the most effective ways to boost energy, extensive workup should be conducted prior to its use. This hormone should not be used in people with normal testosterone levels. In the Adrenal Fatigue setting, testosterone replacement is seldom necessary as there are many more gentle nutrients available without the body being exposed to this strong androgen.
One of the causes of the disruptions of sleeping patterns for people suffering from Adrenal Fatigue and aging is the reduction in the nightly release of melatonin by the pineal gland. Many people have discovered that bedtime doses of melatonin will restore their ability to have a sound and peaceful night's sleep. This helps not only with sleep onset insomnia (difficulty in falling asleep), but also sleep maintenance insomnia (waking up at night and unable to fall back to sleep).
In our studies, we have learned about hormonal imbalance and its interactions with melatonin. Melatonin levels are known to decline drastically with age. Since melatonin and FSH appear to be antagonistic in women, the same relationship may be true for men. It has been postulated that melatonin may even act to normalize (lower) gonadotropin levels. It is one of the few substances that have repeatedly been shown to extend the maximum life span of experimental animals. While low doses of melatonin (0.5 to 6 mg) act as a natural sleeping pill, high doses of melatonin (20 mg or more) have excellent anti-oxidative properties and are being used commonly in alternative medicine circle to fight breast cancer. Because of its ability to cross the blood-brain barrier, melatonin is also a highly effective compound that can fight cancer that has metastasized to the brain or in treating other neurodegenerative diseases such as Parkinson's Disease or Alzheimer's Disease.
 The exact dosage of melatonin varies greatly among people as the dosage curve is not linear. This is especially true in Adrenal Fatigue. Trial and error is, therefore, the best method. A higher dose does not mean more potency as some people may feel better with a smaller dose. To normalize sleep and the bio clock, a good dosage to start is 0.5 to 1 mg and this should gradually be increased if there are no adverse side effects.
The exact dosage of melatonin varies greatly among people as the dosage curve is not linear. This is especially true in Adrenal Fatigue. Trial and error is, therefore, the best method. A higher dose does not mean more potency as some people may feel better with a smaller dose. To normalize sleep and the bio clock, a good dosage to start is 0.5 to 1 mg and this should gradually be increased if there are no adverse side effects.
Slight disorientation and dizziness may be experienced for the first few hours after waking up when melatonin treatment is first started. This hangover sensation should go away after a few nights of melatonin use. If it persists, a reduced dose is recommended. Some people require as much as 60mg to before it begins to work. This is contraindicated in a pregnant or nursing mother, children, women trying to conceive, people who are on prescription steroids or who have a mental illness, severe allergies, or immune system cancers such as lymphoma.
There are a few rules for the effective use of melatonin. Firstly, always take this hormone just before bedtime. If you take it earlier in the day, it may disrupt sleeping and waking cycles. Those who wake up with a hangover may wish to take it earlier in the evening instead of at bedtime.
Estrogen and progesterone work in synchronization with each other as checks and balances to achieve hormonal harmony in both sexes. It is not the absolute deficiency of estrogen or progesterone but rather the relative dominance of estrogen and relative deficiency of progesterone that is main culprit in Adrenal Fatigue. Let us examine this in more detail.
What we know about hormonal imbalance is that while sex hormones such as estrogen and progesterone decline with age gradually, there is a drastic change in the rate of decline during the perimenopausal and menopausal years for the women in these two hormones.
From age 35 to 50, there is a 75% reduction in production of progesterone in the female body. Estrogen, during the same period, only declines about 35%. By menopause, the total amount of progesterone made in the body is extremely low, while estrogen is still present in the body at about half its pre-menopausal level. With the gradual drop in estrogen but severe drop in progesterone, there is insufficient progesterone to counteract the amount of estrogen in our body. This state is called Estrogen Dominance.
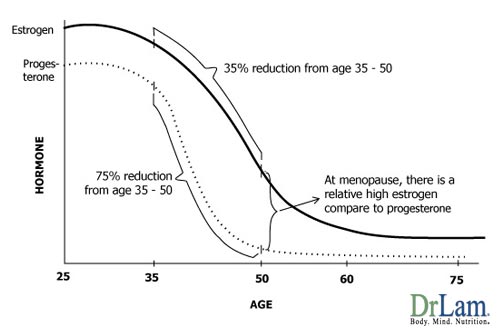
Estrogen Dominance affects about half the women in the United States. It is caused by an imbalance between 'the stimulating hormone' estrogen and 'the calming hormone' progesterone and is the cause of many metabolic dysfunction symptoms. Many women in their mid-thirties, most women during perimenopausal (mid-forties), and essentially all women during menopause (age 50 and beyond) are overloaded with estrogen and at the same time suffering from progesterone deficiency because of the severe drop in physiological production during this period. This is further compounded by stress and the environment, both of which result in the body's overall estrogen load. The end result - excessive estrogen relative to progesterone is a condition we call estrogen dominance.
What is so bad about estrogen dominance? It is the root cause of a myriad of illnesses. Conditions associated with this include fibrocystic breast disease, PMS, uterine fibroids, breast cancer, endometriosis, infertility problem, endometrial polyps, PCOS, auto-immune disorders, low blood sugar problems and menstrual pain, among many others.
Estrogen dominance and Adrenal Fatigue are closely related. One of the hallmarks of Adrenal Fatigue Stage 3B is the presence of Estrogen Dominance. When the adrenals are stressed, their response is to increase cortisol output and this requires more progesterone, a precursor. Cortisol output rises in Stage 1 and Stage 2 of Adrenal Fatigue. As adrenal weakness advances, cortisol output will begin to decline after peak production cannot be sustained and the adrenal glands become tired. The body's increased need for cortisol depletes the progesterone levels. As more progesterone (and also pregnenolone) is shunted or sequestered to make cortisol, less is available to balance off the estrogen. As a result, there is a relative increase in estrogen in the body compared to progesterone during Adrenal Fatigue, further compounding any pre-existing Estrogen Dominance.
Most women with Stage 3B Adrenal Fatigue or higher invariably suffer from Estrogen Dominance as a result. Those women who suffer from one condition tend to have the other condition to some degree. Because the symptoms are similar, Estrogen Dominance, when prominent, can mask the underlying Adrenal Fatigue, which then is overlooked. Clinicians can be misled into believing that the root problem is Estrogen Dominance when in fact it is Adrenal Fatigue in disguise. Administration of hormone replacement, natural or otherwise, may give temporary relief but it will normally fail over time if adrenal recovery is not first given the primary focus. Conversely, symptoms of Estrogen Dominance tend to subside when optimum adrenal health returns.
Another common reason for low progesterone levels is the anovulatory cycle (a menstrual cycle in which there is no ovulation). In Adrenal Fatigue, the body's emergency repair system is activated but priority is given to metabolic balance to keep the basic bodily functions, such as blood pressure and blood sugar, stable. Reproductive functions are considered to be low priority at this point and accordingly, ovulation can be temporary shutdown. In fact, many women under high stress will have irregular menstrual cycles and amenorrhea for this reason. Without the ovulation, there is no corpus luteum to make additional progesterone for the cycle. The lowered progesterone level leaves the women with an excessive estrogenic effect due to the deficiency of progesterone.

Estrogen Dominance can also be caused by excessive estrogenic stimulation from other sources. As Adrenal Fatigue progresses (with the exception of adrenal failure), weight gain is usually the norm as the body tries to slow down metabolism to conserve energy. When this happens, excessive fatty tissues are accumulated and fat cells will make estrogen and this estrogen will, in turn, cause fatty tissue growth. Both Estrogen Dominance and Adrenal Fatigue will lead to excessive estrogen and relative progesterone deficiency.
Those who are on birth control pill, as well as those who are exposed to environmental estrogen-like compounds called xenoestrogen, may compound that problem. Chemicals that mimic estrogen can be found in many plastics and they can enter the food chain when microwaving food in plastic dishes or when plastic wraps and containers are used. These estrogen-like compounds can also come from eating non-organic food as livestock are typically given potent estrogenic substances ('super-estrogens') to make them more grow faster.
Estrogen also increases thyroid-binding proteins in the bloodstream. Thyroid blood test results may, therefore, be normal although there may be insufficient free thyroid hormone in the tissues, resulting in a state of sub-clinical or secondary clinical hypothyroidism.
When estrogen levels are high, the adrenal cortex will fail to respond to signals from the brain. A woman with Estrogen Dominance may have adequate levels of total cortisol in her bloodstream and blood tests of total cortisol may be well within the normal range. However, her free available cortisol level may be low. Since only free cortisol can pass through cell membranes and activate the receptors inside the cell, the effectiveness of cortisol is blunted at the cellular level.
Synthetic progesterone called Progestin is sometimes prescribed to combat such deficiency by conventional physicians but this can make matters worse. Progestin is similar to progesterone but acts differently from progesterone because it is molecularly different. Our bodies cannot convert the Progestin into cortisol to help the adrenals or convert them into any other hormonal compounds as we can with bio-identical progesterone. Progestin can also be highly toxic and hard to break down in those people suffering from advanced Adrenal Fatigue, leading to a build-up of toxic metabolites in the body.
Reducing estrogen overload is an important clinical goal in Adrenal Fatigue recovery. Healing the adrenals indirectly helps improve this by allowing more progesterone to be available to offset the estrogen. Direct help to the estrogen-progesterone balance will indirectly support the adrenals by making more progesterone available for cortisol production. Both go hand in hand. In addition, progesterone itself has a toning down, calming and sleep-supporting effect which will further help to restore the stressed adrenals.
The easiest way to restore balance to Estrogen Dominance is with natural progesterone which is different from the prescription Progestin mentioned above. There are different ways to take progesterone and they can the women differently. There are many delivery systems available, but for most women, the low dose topical form is most inexpensive and works well. However, the right dosage and time are the keys and this is especially true in the case of Adrenal Fatigue.
 Wrong dosage or timing can make Adrenal Fatigue condition worse and may even trigger adrenal crashes. People who are in low clearance state which is characteristic of Adrenal Exhaustion need to be especially careful. For these people, even normal physiological dose may be too much for the body to handle. The temptation to overcome Estrogen Dominance may be great, especially if the clinical symptoms are severe but it is always best to heal the adrenals first as much as possible and delay the administration of natural progesterone until the body becomes ready. The stronger the body, the better it is able to tolerate natural progesterone and the stronger the liver will be to metabolize the chemical.
Wrong dosage or timing can make Adrenal Fatigue condition worse and may even trigger adrenal crashes. People who are in low clearance state which is characteristic of Adrenal Exhaustion need to be especially careful. For these people, even normal physiological dose may be too much for the body to handle. The temptation to overcome Estrogen Dominance may be great, especially if the clinical symptoms are severe but it is always best to heal the adrenals first as much as possible and delay the administration of natural progesterone until the body becomes ready. The stronger the body, the better it is able to tolerate natural progesterone and the stronger the liver will be to metabolize the chemical.
There has been some controversy regarding which form is best to take the progesterone. Physicians tend to favor oral form (Prometrium), which is a prescription medication. Since around 80% is broken down by the liver, to get a 20mg blood level dose, you will need to take a 100mg capsule. This places an extra burden on the liver as it is the clearance center for this hormone. Most with Adrenal Fatigue are already stressed and in low clearance state, to begin with and this overload of oral progesterone may trigger adrenal crashes when the liver is being overwhelmed sub-clinically. Blood level tends to be short lasting and as a result, it may require splitting the original dose into 2 doses daily to get a more even or stable blood level throughout the day/night. In short, oral form of progesterone is not recommended for those suffering from Adrenal Fatigue.
Troche (soft tablets you dissolve under your tongue) is another option. It is less convenient than a capsule but less messy than a cream overall. To get the physiological level of 20mg, you need a 20mg troche. Some people don't like sucking on a tablet for the 1-2 minutes it takes to dissolve. Blood level tends to be short lasting and it may require splitting the original dose into 2 doses daily to get a more stable blood level throughout the day/night. Furthermore, it is also expansive.
Topical progesterone cream is the most common and it comes in a variety of concentrations. The best for people suffering from Adrenal Fatigue is the low-dose over the counter form. To get a 20mg blood level, you need to apply 20mg. Progesterone is lipophilic and it likes to stay in a fatty environment, allowing us to modulate the rate of release. Application to an area such as the abdomen with a thick fatty layer will slow the release. Application to an area such as the wrist or a thin fatty layer would lead to faster release. Cream tends to be a bit messy, but for most women, this is the best alternative overall and the least expensive. For best results, one needs to rotate the site of application to allow the skin to refresh itself. Many over the counter brands are available and they vary greatly in quality. Topical progesterone cream tends to release slowly over hours, days, or weeks from fatty tissue deposits. If used correctly, a steady blood level of progesterone can be achieved better with cream than by any other practical method. Those in Adrenal Fatigue will do much better with the topical form of progesterone as compared to other forms.
Women suffering from Adrenal Fatigue should be especially careful of high potency progesterone cream which is commercially available because it can trigger adrenal crashes. Even normal potency cream may sometimes be too much for those suffering from Adrenal Fatigue.
As with most hormones, too much can cause problems. In the case of Adrenal Fatigue, even a small amount below physiological amount can be a big problem. In addition to intolerance and sensitivity, too much progesterone is actually counterproductive. Chronically high dose of progesterone over many months will eventually cause progesterone receptors to turn off, reducing its effectiveness and may lead to toxic side effects. Some possible side effects include:
It is important to be as accurate as possible when applying progesterone cream. The best low dose progesterone cream should contain 1.7% of progesterone and yield 20 mg of progesterone per application. The simplest application method is through the use of a metered pump that measures the exact amount (20 mg), each time the pump is pressed. Progesterone is best absorbed where the skin is relatively thin and well supplied with capillary blood flow. Areas such as the face, neck, upper chest and inner arms are good areas for application. Spread out to as big an area as possible for maximum absorption and allow for as much time as possible for absorption. Therefore, bedtime application is best if you are applying it once a day. Twice a day application is best but it may be too troublesome for most people. Lastly, rotate to different areas to avoid saturation in any one particular site.
Here is a sample rotational application protocol:

Practically speaking, the best gauge for the ideal dose should not be determined by any laboratory test alone. It is important to rely on the relief of symptoms when figuring out the ideal dose. The right dose is the dose that works. This is especially critical in Adrenal Fatigue. Always start only after the adrenal functional reserve is well established. Start with a small dose if in doubt and slowly scale up under professional guidance.
The following are general recommendations for topical progesterone cream application that may need to be modified in specific situations:
Women in premenopausal - still ovulating:
Women in perimenopausal (still menstruating with menopausal symptoms and/or PMS but not ovulating):
Women in menopause (not menstruating):
Estrogen represents an entire family of female related hormones and consists of three components: E1 (estrone), E2 (estradial), and E3 (estriol). E1 is the most potent and carcinogenic. E3 is the most gentle and in fact has anti-cancer properties. In the body, these hormones exist in perfectly balanced proportions. The amount of E3 is highest, while E1 is lowest. Estrogen is manufactured primarily in three places of the body: ovaries, adrenal glands, and fat cells. Your chances of Estrogen Dominance increase if you are overweight.
Receptor dysfunction can also trigger Estrogen Dominance. This is more commonly seen in skinny women that are not under any apparent stress but are clinically symptomatic. Because estrogen deficiency or dominance can produce similar symptoms, estrogen replacement, whether it is natural or synthetic, needs to proceed with care.

Most women who have Adrenal Fatigue are in a state of Estrogen Dominance due to progesterone deficiency. This is made with women who are also overweight. Symptoms consistent with excessive estrogen such as PMS, endometriosis, fluid retention, depression, fibrocystic breast disease are commonly associated the Ovarian-Adrenal-Thyroid Axis Imbalance characteristic of women who are in Stage 3B Adrenal Fatigue.
The best way to normalize Estrogen Dominance is through the use of natural progesterone. From time to time, a woman can present with the all too familiar symptoms of Estrogen Dominance, but in fact she is estrogen deficient. This is usually more prevalent in women with normal or below normal weight. The physiology is unclear, but may be related to receptor site or transport dysfunction. Enhancing liver function also can be helpful.
As mentioned earlier in this article about hormonal imbalance, symptoms of estrogen deficiency can be similar to Estrogen Dominance. Those with these symptoms occurring from day 4-14 of the menstrual cycle should be on the alert for estrogen deficiency if they fit the weight distribution profile and should learn about hormonal imbalance. Estrogen replacement can be of great relief once the woman's adrenal function has been stabilized. Because estrogen is metabolized by the liver, the majority of those with advanced Adrenal Fatigue will concurrently have weak liver function and slow clearance. Aggressive use of estrogen when the liver and adrenals are not normalized can actually make the Adrenal Fatigue condition worse off and may trigger adrenal crashes, making it important to know all you can about hormonal imbalance.

Balance Hormones for Natural Energy – Liquid Vitex
People with AFS tend to have weak immune system, where candida thrives.
For a disease to be an official diagnosis, it has to go through many clinical trials. This is a slow process that can take upwards of 50 years.
When your body is stronger and able to sustain itself, the level of steroid can be reduced. Letting your doctor know is the key as well as following your doctor's instructions.
It may, depending on the purpose and timing. Often in a setting of AFS, allowing the body to self-regulate is much better because the body can then have the automatic mechanisms to activate the feedback loop and fine tune what it needs.
Depending on what kind of hormones are left untreated you may or may not experiences that make you concerned about hormonal imbalance. If you are concerned about hormonal imbalance, note that if your thyroid is not functioning properly, metabolism may go down, feeling of fatigue, lethargic, or other health issues can surface. For ovarian hormones, irregular cycles, PMS, infertility, miscarriage, or breast cancer are just a few problems. For Adrenals, inability to handle stress, fight and flight, hypoglycemia, weight gain, fatigue are just some symptoms. For those of you that continue to wonder about hormonal imbalance, continue also to read and learn and educate yourself concerning health options.
"I looked at the video DHEA and Cortisol. I loved it very much."
"Dr. Lam, I looked at the video DHEA and Cortisol. I loved it very much and it has been a great help The guidance and education imparted was of much use. I listen to others as well, but this one fell onto my plate. Thank you so much. Take care and have a wonderful day. Talk with you at our next appointment"