 Benzodiazepines, also called “benzos” or BZD for short, are tranquilizers. They are most often given for anxiety and insomnia, but also as muscle relaxants and anticonvulsants. They are also used for alcohol withdrawal symptoms. Although benzos are meant for medical use only, some people use them recreationally. If taken for long enough, you can develop a benzodiazepine dependency, which leads to benzo withdrawal symptoms when trying to cut down or discontinue use. This is why it’s not a good idea to take them on a daily basis for three months or longer, as this increases the chance of dependency.
Benzodiazepines, also called “benzos” or BZD for short, are tranquilizers. They are most often given for anxiety and insomnia, but also as muscle relaxants and anticonvulsants. They are also used for alcohol withdrawal symptoms. Although benzos are meant for medical use only, some people use them recreationally. If taken for long enough, you can develop a benzodiazepine dependency, which leads to benzo withdrawal symptoms when trying to cut down or discontinue use. This is why it’s not a good idea to take them on a daily basis for three months or longer, as this increases the chance of dependency.
You’ve probably heard of some of these benzodiazepine meds and sleeping aids, as well as the similar-in-action yet chemically different “Z-drugs”:
There are other types and brands of benzodiazepines as well. If your doctor ever recommends tranquilizers or sleeping aids, it’s a good idea to check to see if they are benzos, so you know what you’re dealing with.
Although some are taken through intravenous injections, most benzo drugs are taken in oral form. When ingested, they are absorbed by the stomach and small intestines, then metabolized by the liver. They are excreted through urine, saliva, sweat, and feces. These drugs are fat-soluble and stored in fatty tissues.
Benzo withdrawal is known to be one of the more difficult to experience, and if coupled with a condition like adrenal fatigue, it can be quite a complex challenge. For those with adrenal fatigue and chronic stress, this article covers what benzodiazepines are and how they affect the body, as well as their relationship to the adrenal glands, cortisol, and the overall stress response.
Benzodiazepines act by enhancing the effect of the neurotransmitter gamma-aminobutyric acid (GABA) throughout the brain and nervous system. Neurotransmitters are chemicals that transmit impulses between brain cells, either exciting or inhibiting reactions by the receiving brain cells.
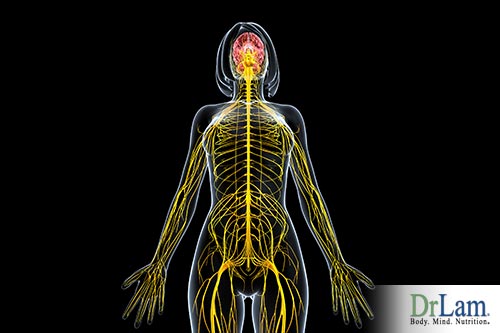 GABAs are the body’s primary inhibitory neurotransmitters. They decrease the excitability of neurons in the nervous system and regulate the muscle tone. By binding to GABAA receptors, they help calm anxiety, induce sleep, and relax the muscles. They affect memory, emotions, coordination, thinking, and consciousness.
GABAs are the body’s primary inhibitory neurotransmitters. They decrease the excitability of neurons in the nervous system and regulate the muscle tone. By binding to GABAA receptors, they help calm anxiety, induce sleep, and relax the muscles. They affect memory, emotions, coordination, thinking, and consciousness.
GABAs do an important job calming down nervous system responses. To understand their function, it helps to understand how the nervous system operates.
The autonomic nervous system (ANS) is composed of five branches, including the parasympathetic nervous system (PNS), the sympathetic nervous system (SNS), and the sympathoadrenal hormone system (SHS).
Each system controls a certain response depending on what’s needed at the time. When there is stress, the SNS and SHS are activated, creating the “fight or flight” response. The degree of activation corresponds to the degree of stress perceived by the body.
It is all part of the NeuroEndoMetabolic (NEM) Stress Response that helps the body deal with stress. This holistic and functional perspective on stress explains how the whole body reacts. When there is no stress, the PNS activates the “rest and digest” response.
Although the “fight or flight” response is necessary in dangerous situations, most stress in modern times is not due to a threat to survival. Your SNS and SHS can be triggered to release norepinephrine and epinephrine (also called adrenaline) deal with stress that can be emotional or psychological as well as physical.
 Adrenaline is a hormone that is excreted by the adrenal medulla which acts on metabolism. It is the most powerful hormone in the body when it comes to dealing with stress. Norepinephrine is both a neurotransmitter and a hormone. In the brain, it acts as a neurotransmitter, putting us on alert mentally. Peripherally, outside the central nervous system, norepinephrine acts on the cardiovascular system’s sympathetic nerves. Together, they increase heart rate and breathing and release a shot of energy into the body, so that you can fight off danger or run away from it.
Adrenaline is a hormone that is excreted by the adrenal medulla which acts on metabolism. It is the most powerful hormone in the body when it comes to dealing with stress. Norepinephrine is both a neurotransmitter and a hormone. In the brain, it acts as a neurotransmitter, putting us on alert mentally. Peripherally, outside the central nervous system, norepinephrine acts on the cardiovascular system’s sympathetic nerves. Together, they increase heart rate and breathing and release a shot of energy into the body, so that you can fight off danger or run away from it.
Norepinephrine, adrenaline, and dopamine fall into a class of chemical compounds called catecholamines. GABAs help to reduce the effect of catecholamine-driven responses so that you’re not constantly “switched on”, enabling you to relax in mind and body. They are like an antidote to adrenaline and norepinephrine.
Taking a benzodiazepine will enhance the GABAs’ ability to neutralize this “fight or flight” response, letting your “rest and digest” response activate. In other words, GABA is a natural opponent and balancer of catecholamines.
There are short-acting, intermediate-acting and long-acting benzos. Short-acting benzos, like Tranxene, can last for three to eight hours. Intermediate-acting benzos, like Ativan, can last from eleven to twenty hours. And long-acting benzos, like Librium, can last one to three days. Some benzo drugs have a very fast onset of action, like Valium for example, which can have an effect within an hour.
Unlike other psychiatric medications, such as antidepressants (which may take weeks to begin having an effect), benzos are effective almost immediately.
Different types of benzos can be taken for short-term, intermediate-term, or long-term use. After understanding their potential side effects and withdrawal symptoms, however, you will most likely feel that short-term is the best option.
Short-term use can be for things like sedation during surgery, or just for a few days during a challenging life situation such as a death in the family or losing a job. These types of benzos should not be taken for more than a few days if possible.
Intermediate use could be to help with alcohol withdrawal symptoms, for example.
Long-term benzo use is usually reserved for chronic anxiety and panic attacks, although in some people this can worsen the very symptoms they are meant to help.
Long-term use of benzos can damage the GABA receptors. Development of dependency and resistance can make dosage reduction difficult. Not only that, but long-term use, over years for example, actually induces withdrawal-like symptoms, even if you do not reduce the dose.
One peculiar symptom that long-term users can experience, with or without going through benzo withdrawal, is something called ‘depersonalization’. It’s a feeling of not being quite real, that parts of your body are not attached to the rest, or that you are outside of yourself as an observer. It can also seem like the world itself is less real.
Some people with depersonalization feel like they are looking at someone familiar in the mirror but that this person is not actually themselves. What is most disturbing about depersonalization is the emotional reaction to it. Feeling this way can be very frightening, making you think you’re going crazy. These reactions will depend on the severity of the symptom and how long it lasts.
A patient goes to a doctor complaining of anxiety and insomnia and is given a benzodiazepine. At first, it works so well that this patient feels she has found an easy and effective solution to her problems. After a little while, though, she begins to experience some unwanted side effects and hears that these drugs are addictive.
 She then goes back to her doctor with concerns, where she is promptly told that these drugs are perfectly safe, non-addictive, and can be taken for life. So she keeps renewing her prescription and taking the medication.
She then goes back to her doctor with concerns, where she is promptly told that these drugs are perfectly safe, non-addictive, and can be taken for life. So she keeps renewing her prescription and taking the medication.
However, as her tolerance builds, she needs to increase her dosage or take the drugs more often for them to work. On challenging days, she might even take double what she normally takes. At some point, that dose may become the norm.
After a while, this patient begins to worry about her health and considers getting off the drug completely. However, as she starts to experience benzo withdrawal symptoms, she mistakes these symptoms for her original state of panic and insomnia, and she feels she needs to be taking the medication again.
This dance may go on for many years if she is not well informed about the effects and symptoms of benzo withdrawal.
Because of this common scenario, it is highly recommended that if you are considering or taking benzos, you get the full picture before deciding what steps to take next. The best approach is to make a plan and have some realistic expectations of how this journey will unfold.
There are many benzo withdrawal symptoms experienced by long-time users, with variations in severity. Symptoms can come and go in waves, which makes it difficult to predict when the symptoms will stop for good.
Some users experience a lessening of symptoms over the course of a few days or weeks. Then suddenly, symptoms recur with the same severity as they had at the beginning, making them feel hopeless about their progress.
Though not everyone experiences withdrawal, the majority of long-term users do. The symptoms of benzo withdrawal include:
This is not a full list. No one experiences all of these symptoms at the same time. Most people will experience a combination of a few of them on an on-again-off-again basis. The intensity of symptoms also varies from person to person. One of the most frequently overlooked symptoms is the onset of adrenal crashes. This is when the body undergoes a massive loss of energy, resulting in extreme fatigue that may incapacitate a person.
In addition, some people experience psychosis, blackouts, and hallucinations. Rarely, people can experience physical symptoms of nosebleeds, hair loss, rectal bleeding, hemorrhoids, sinus pain, and sensitivity to touch. Depersonalization can also be a benzo withdrawal symptom.
Due to some of these symptoms, other problems may also arise, such as an increased risk of accidents and falling. Those going through very challenging withdrawals can experience suicidal ideation.
Benzo withdrawal can take weeks, months, or even years, depending on how long and how often the drugs were used. For long-term users, it can take two years for the brain and nervous system to fully return to a healthy state. The damage done to GABA receptors and the different hormonal systems in the body needs time to regain balance.
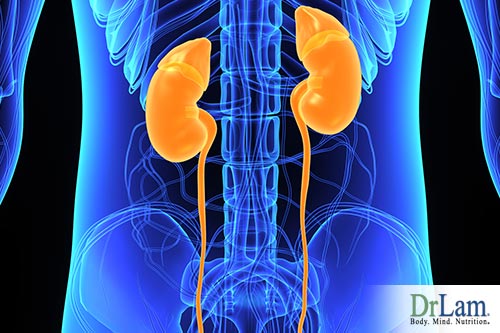
The hypothalamic-pituitary-adrenal (HPA) hormonal axis is the system of interactions between the hypothalamus and pituitary glands. The adrenal glands sit on top of the kidneys and have important functions such as regulating the immune system, digestion, sexuality, energy, emotions, and the stress response.
 The HPA axis is basically a hormone cascade, releasing a hormone that then signals for the release of the next hormone that then signals for the release of the next.
The HPA axis is basically a hormone cascade, releasing a hormone that then signals for the release of the next hormone that then signals for the release of the next.
This begins in the paraventricular nucleus (PVN) of the hypothalamus, which contains neurons that “switch on” when there is stress or a change in the physiological state. Depending on the input signal to the brain, the PVN will secrete the appropriate peptides.
The PVN releases two hormones that begin the hormone cascade of the HPA axis: the anti-diuretic hormone (ADH) and the corticotropin releasing factor (CRF). These peptides leave the hypothalamus and, upon arrival, stimulate the pituitary gland to secrete the adrenocorticotropic hormone (ACTH).
ACTH then binds to the receptors in the adrenal glands, signaling them to release pregnenolone, which then is converted into a variety of other hormones, and ultimately, cortisol. Over 50 hormones are produced in the entire cascade. Once the cortisol has completed its job (neutralizing stress, for example), any excess will then signal the hypothalamus to stop its production of CRF.
GABAs inhibit the PVN, which is what releases the hormones that activate the HPA hormone cascade in the first place. It does this by suppressing the output of CRF and ADH, the two hormones that stimulate the pituitary gland to secrete ACTH.
When functioning properly, this inhibition is part of the natural balance between the GABAs and the excitatory glutamates that stimulate the PVN and therefore the HPA axis. This is part of the body’s regulatory system to ensure no single hormone dominates during normal daily living. However, a disturbance in this equilibrium will also disrupt the normal functioning of the HPA axis. This imbalance can have many causes, including the use of benzodiazepines and excessive stress.
 GABAs and benzos calm the body and mind when stress is present. Thus, it is important to understand the body’s natural anti-stress mechanisms to understand how benzo withdrawal fit into the overall picture.
GABAs and benzos calm the body and mind when stress is present. Thus, it is important to understand the body’s natural anti-stress mechanisms to understand how benzo withdrawal fit into the overall picture.
The NeuroEndoMetabolic (NEM) Stress Response is the body’s global strategy in the handling of stress, whether physical or mental. It is composed of six circuits that work together as an ecosystem: the cardionomic, the neuroaffect, the metabolism, the hormone, the detoxification and the inflammation responses. Together, they form a holistic and functional apparatus to help the body deal with stress. The HPA hormonal axis is part of the hormonal circuit, but the body’s approach to stress is much more complex than simply the HPA axis.
The central nervous system, the autonomic nervous system, and the gut regulate one of the circuits of the NEM: the neuroaffect response. When this response is dysfunctional, the neurotransmitters that helped keep it in balance are also dysregulated. This leads to an increase of adrenaline and norepinephrine and a decrease in GABA. This can result in anxiety, tension, restlessness, sleep disturbances, racing thoughts, panic attacks, fears, and constant worrying.
The adrenals, part of the HPA axis, are central to the hormonal circuit of the NEM stress response. They are the first and main defense against stress. They secrete cortisol, the most important stress-fighting hormone, as well as over 50 other hormones. Cortisol helps regulate blood pressure, normalize blood sugar, maintain heart and blood vessels, suppress the immune system, and fight inflammation.
Though fully equipped to handle short-term stress, when stress becomes chronic or severe, the adrenals are overworked and cortisol levels dysregulate. This dysregulation produces a set of symptoms known as Adrenal Fatigue Syndrome (AFS).
AFS symptoms include fatigue, difficulty falling asleep, waking up in the middle of the night, easily gaining weight, difficulty losing weight, brain fog, poor concentration, anxiety, depression, hypoglycemia, heart palpitations, sensitivity to certain foods and drugs, heart palpitations, PMS, low libido, fertility issues, and more.
The type and severity of the symptoms experienced will depend on the stage of AFS.
In the beginning stage of AFS, the adrenal glands will increase their production of cortisol to meet the growing demand. After a while, though, they begin to weaken, and their output eventually decreases. This leaves the rest of the NEM to compensate, and the body is even more exposed to the dangers of constant stress. If left this way, the rest of NEM begins to dysregulate as well.
Cortisol and GABA are not directly related. Each one acts on stress through different channels. GABA acts through the brain and nervous system, while cortisol acts through the HPA axis. However, they both affect stress, allowing one to partially relieve symptoms of stress when the other is out of balance.
For example, if you suffer from AFS, GABA becomes a very important component in recovery, helping you get more rest and react less intensely to stressful triggers. This is especially true during the later stages of AFS when cortisol levels are low. However, prolonged stress can also affect GABA levels, reducing its ability to compensate for low cortisol and help with AFS recovery.
One study, The Netherlands Study of Depression and Anxiety (NESDA), researched this link between benzodiazepine and cortisol.
They categorized 1531 people who have had a lifetime diagnosis of depression or anxiety into three groups: (1) daily benzo users, (2) infrequent benzo users, and (3) nonusers. There were 93 people in the first category, 172 in the second, and 1263 in the third. Dosage, duration, and dependence were also taken into consideration.
 The subjects had their salivary cortisol recorded during different phases. What the NESDA found was that daily and infrequent users of benzodiazepines had lower evening cortisol than nonusers. The results did not show that long-term use has a role in dysregulating the HPA axis, however.
The subjects had their salivary cortisol recorded during different phases. What the NESDA found was that daily and infrequent users of benzodiazepines had lower evening cortisol than nonusers. The results did not show that long-term use has a role in dysregulating the HPA axis, however.
For those in the later stages of AFS, a reduction in the level of cortisol can lead to an adrenal crash. The body is already struggling to neutralize chronic stress with the little cortisol it can produce. Add to that the cortisol-suppressive effects of benzodiazepines, and you have a recipe for such low levels of cortisol that the stress can overwhelm the system.
The NEM stress response and the adrenals are weakened by long-term benzo use and withdrawal. This is another important aspect of the relationship between benzodiazepines and cortisol.
At first, benzos and sleeping pills reduce cortisol production. But as tolerance to the drugs builds, side effects and symptoms begin to emerge that are stressful to the body and mind, making the adrenal glands produce more cortisol to counter this stress.
This is especially true for those going through benzo withdrawal, as the symptoms can be quite stressful and take a long time to disappear. This puts pressure on the adrenals to produce enough cortisol to neutralize that added stress. Also, sleep disturbances and fatigue demand higher cortisol production, taxing the adrenals heavily.
As benzos increase GABA activity, they also lessen the output of excitatory neurotransmitters like adrenaline and dopamine. Although initially, that’s what benzos are meant to do, these neurotransmitters facilitate normal functioning of memory, coordination, muscle tone, blood pressure, heart rate, alertness, and emotional response. When they’re lacking in the system, all of these functions suffer.
Additionally, there are benzodiazepine receptors in the blood cells, adrenal glands, colon, and kidneys, making these areas susceptible to damage by long-term use as well. This is why there is such a wide variety of symptoms and side effects, ranging from hormonal imbalance to endocrine problems, including problems with the pituitary, pineal, adrenal, thyroid, and reproductive glands.
For someone struggling with AFS, the high levels of cortisol over long periods of time can affect the production of dopamine and serotonin. This can then lead to anxiety, depression, insomnia, and other symptoms. When such symptoms persist, this person may go to a doctor and receive benzodiazepines. This affects cortisol levels in turn, creating a problematic cycle.
When reducing benzo use, it is of utmost importance that you do not go cold turkey. Suddenly stopping benzodiazepine medication can increase your risk of having a stroke, seizures, heart attack, or hallucinations.
When the level of benzodiazepine in your system dips too low, the panic and anxiety you may experience can be overwhelming, forcing you to seek relief by either upping the dosage again or taking another drug.
 It is important to prepare yourself with the understanding that this will be a long process. In fact, the slower you taper off benzos, the gentler the process can be. Consider aiming for months or, in extreme cases, years before getting completely off the medication. This is especially wise if you have AFS as well.
It is important to prepare yourself with the understanding that this will be a long process. In fact, the slower you taper off benzos, the gentler the process can be. Consider aiming for months or, in extreme cases, years before getting completely off the medication. This is especially wise if you have AFS as well.
Also, it is very important to make sure you are supervised by a doctor who is well versed in benzo withdrawal. Avoid medications to ease withdrawal symptoms, but that actually worsen your condition. This is a common mistake that can prolong the process.
The good news is that what you do during the benzo withdrawal phase will influence how quickly and fully you return to good health. For example, during your withdrawal, avoid consuming alcohol, caffeine, honey, monosodium glutamate (MSG), artificial additives, and sugars.
Also, if you can avoid it safely, do not take hormone supplementation or hormone replacement therapy without proper supervision. Steroids such as DHEA supplements, progesterone creams, and hydrocortisones can have an adverse effect on your recovery.
Your main aim should be to let your body restore its hormonal balance naturally. If you supplement with hormones at this time, your body’s own production will be inhibited and remain in a weak state. Many of these preparations can also be too stimulating, adding to the anxiety and excitation that is experienced in benzo withdrawal.
When working towards AFS recovery, GABA can play a supportive role. Some may find GABA supplements help relax the body and mind. They can also help with some AFS symptoms, such as anxiety and sleep disturbances. Herbal supplements that stimulate GABA receptors are also an option.
Unfortunately, most people tend to overlook the need to pre-plan their exit strategy when it comes to GABA enhancement drugs. As a result, they can end up being chronic benzo users.
Not everyone with AFS can tolerate GABA. The weaker the body, the higher the risk. For those who can tolerate them, GABA supplements can help reduce reactions to stressful triggers. Because stress is the main cause of adrenal fatigue, reducing and managing it is one of the most important steps you can take. Giving your system the break it needs to relax and repair can help rebalance to your HPA hormonal axis.
It is important that, if you’ve been on benzo drugs, you do not try adjusting your GABA levels on your own. The receptors may have been damaged by long-term use, and benzo withdrawal can be very stressful on the body. Thus, any changes you intend to make to your supplementations, medications, or diet should first be discussed with an experienced medical professional. You should have medical supervision in order to start weaning off of benzo drugs.
There are several other things you can do to make this process easier and safer. These steps can also help you handle benzo withdrawal properly while you recover from AFS.
The most important step is to reduce as much stress, physical or mental, as possible. For example, if your blood sugar levels are not stable, this is a big stressor. Stabilizing your blood sugar could do wonders for your stress levels and AFS recovery. Following an adrenal fatigue diet may also be helpful and support your adrenals.
 Have honest conversations with your family and friends about what you are about to undertake. Have your doctor explain to them the process and what to expect. Show them how they can best support you during this time.
Have honest conversations with your family and friends about what you are about to undertake. Have your doctor explain to them the process and what to expect. Show them how they can best support you during this time.
Be careful about joining online or offline support groups if you have AFS. A body with adrenal fatigue cannot be handled the same as a body that is healthy. What works for one person can backfire for another. Everyone is different.
Keep regular mealtimes and sleeping/waking times. Make sure you give yourself the best possible chance at a good night’s rest by keeping your room dark and cool, eating a small snack before bed so you don’t wake up from hypoglycemia, limiting caffeine during the day, and avoiding electronic devices for at least two hours before bed.
Light exercise is okay, but this also depends on your stage of AFS. If you are going through benzo withdrawal, you should keep your exercise regiment light. Avoid anything strenuous. You can try adrenal breathing exercises and adrenal yoga exercises. Walking in nature can also be calming and refreshing at the same time.
Remember, if you are going through AFS, benzo withdrawal, or both, you can regain your health and well-being with the right strategy, medical guidance, and community support.
A healthier, happier and more energetic day-to-day life is very possible. Just take it one step at a time in the right direction. The process may take months or longer. All six circuits of the NEM response must be healed. A holistic approach is necessary, along with a comprehensive adrenal support plan that helps the body regain its balance. Some setbacks are expected. Having an expert to coach you each step of the way will help facilitate your recovery in a smooth and comfortable manner.